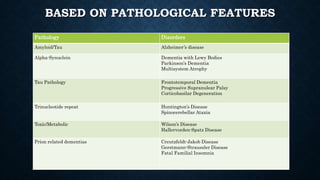
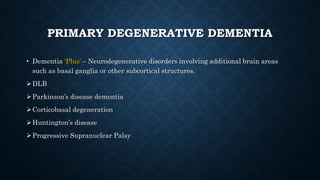
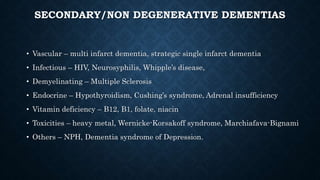
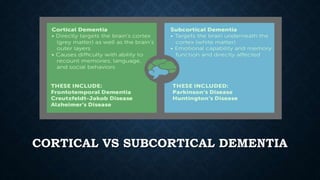
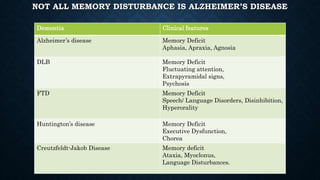
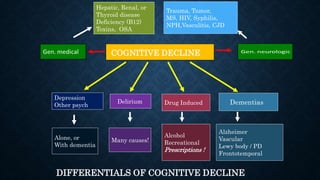
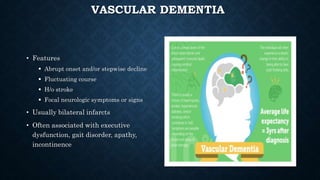
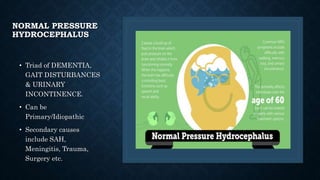
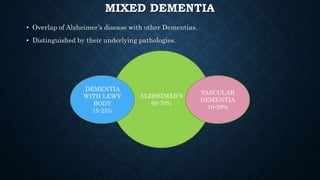
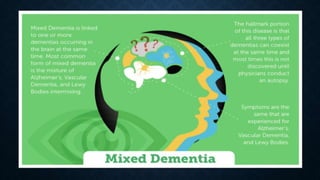
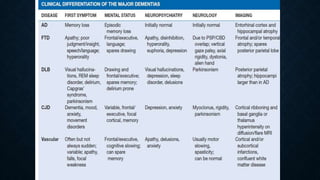
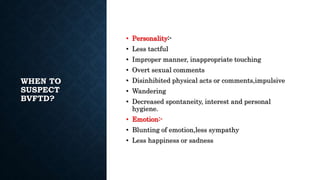
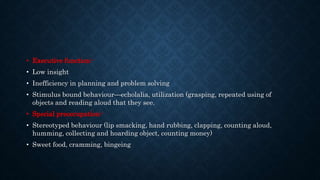
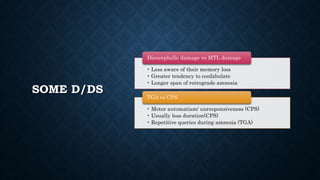
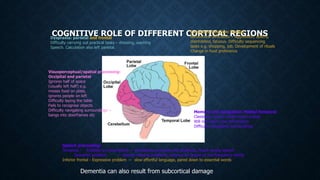
This document discusses the classification and pathological features of various types of dementia. It describes how dementia can be classified based on the pathological proteins involved, such as amyloid/tau in Alzheimer's disease or alpha-synuclein in dementia with Lewy bodies. It also discusses primary degenerative dementias that primarily affect the cerebral cortex, as well as primary degenerative dementias that involve other brain areas. Secondary and non-degenerative dementias are also outlined. The clinical features and distinguishing characteristics of different types of dementia like Alzheimer's disease, vascular dementia, dementia with Lewy bodies, and frontotemporal dementia are summarized.