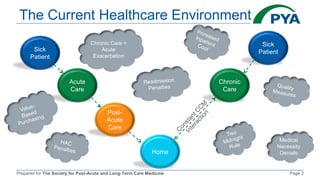
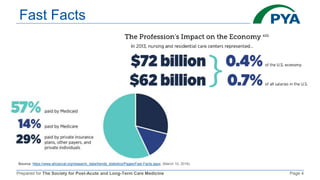
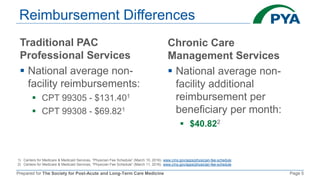
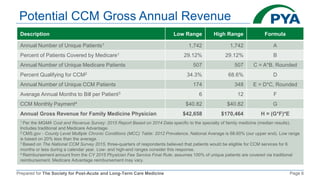
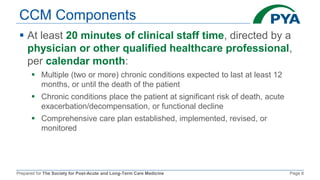
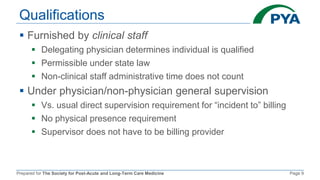
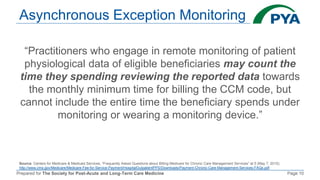
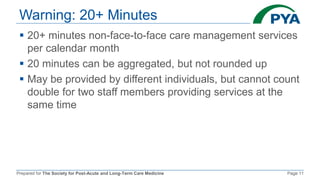
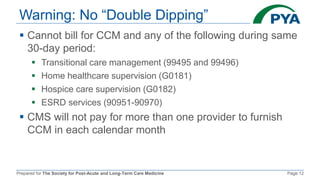
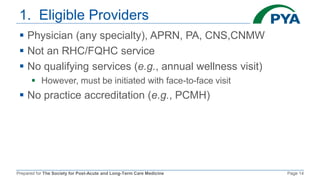
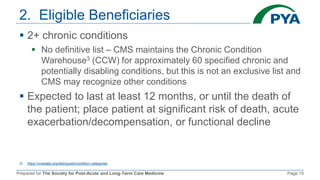
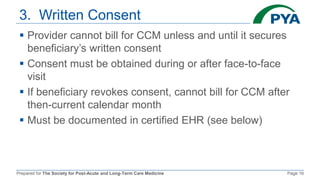
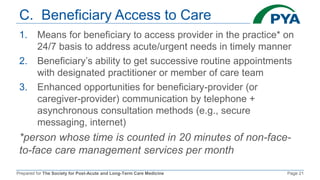
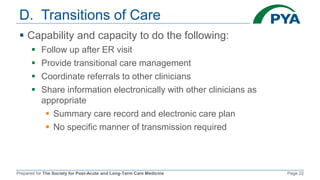
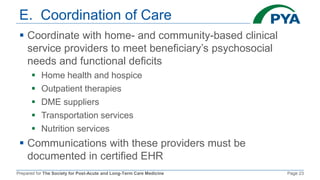
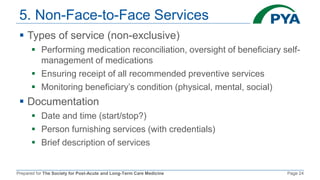
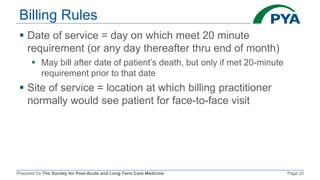
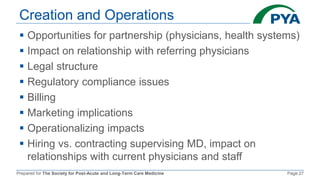
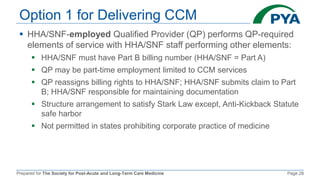
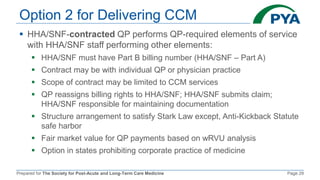
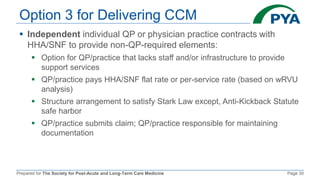
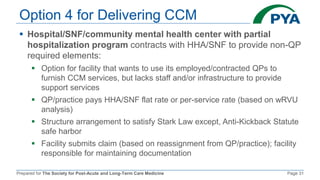
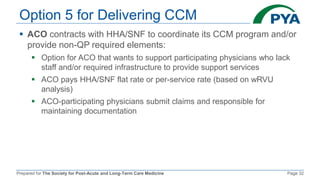
The document outlines the components and billing criteria for Chronic Care Management (CCM) services in a post-acute care setting, emphasizing the requirement of 20 minutes of non-face-to-face care management services per month led by a healthcare professional for patients with multiple chronic conditions. It also details eligible providers and beneficiaries, the necessity of patient consent, and various options for delivering CCM services. Additionally, it discusses potential revenue and reimbursement structures for CCM, highlighting the financial implications for healthcare providers.