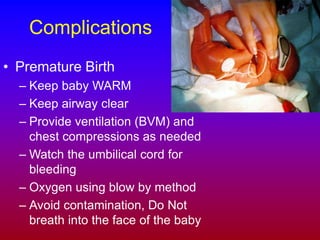
This document provides an overview of obstetric and gynecological emergencies for first responders. It covers topics such as normal childbirth procedures, newborn resuscitation, and complications including abnormal deliveries, pre-delivery emergencies, and gynecological issues. Guidelines are provided for responding to situations such as premature birth, bleeding, trauma, sexual assault, and miscarriage. The focus is on providing emergency medical care and emotional support to pregnant or gynecological patients until they can be transported to the hospital.