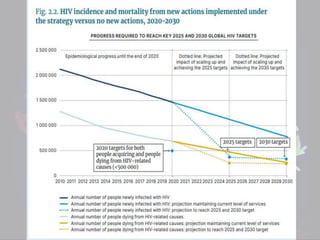
Challenges in HIV prevention were presented by a medical student. Some key challenges discussed include failure to implement prevention strategies effectively, with diagnosis, treatment coverage, and viral suppression varying widely between countries. Additional challenges include lack of awareness of HIV status, fear of testing, inability to maintain ongoing treatment, socioeconomic factors like poverty and lack of access to healthcare, unsafe sex practices, and inadequate resources for prevention. The conclusion calls for a focus on improved implementation of prevention strategies, increasing awareness, funding for treatment and prevention programs, and expanding access to preventive tools and services.
![Introduction
June 1981 first Case of AIDS.
past 40 years, 77.3 million HIV
infections
40.1 million [33.6–48.6 million]
Deaths
In 2017:-
< 1 million died of AIDS-related
causes
about 1.8 million acquired.
In 2020 :-
estimated 1.5 million (UI 1.0 to 2.0
million) people acquired HIV
people living with HIV globally to
37.7 million (UI 30.2 to 45.1 million
Currently, for every two people who
go on treatment for HIV and AIDS,
five People become infected.](https://image.slidesharecdn.com/challengesinhivpreventiontashfeenahmad-221201032124-4a322df2/85/Challenges-in-HIV-prevention-pptx-3-320.jpg)