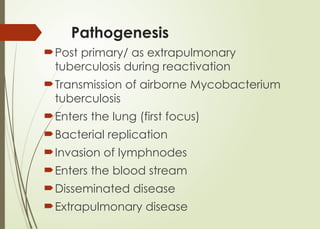
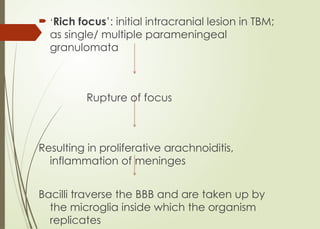
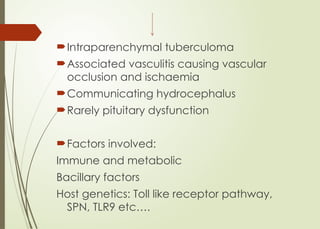
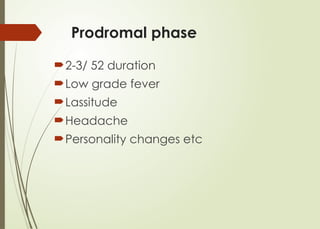
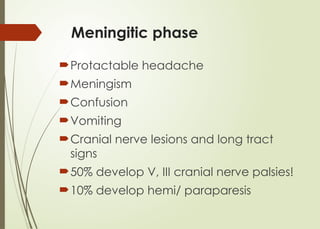
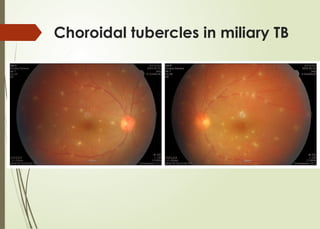
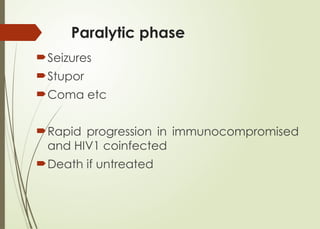
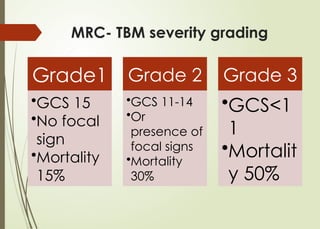
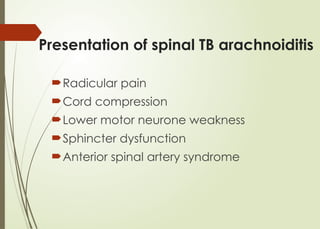
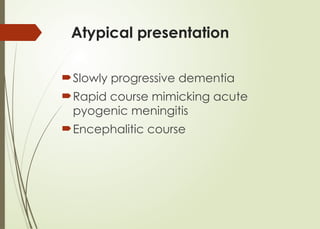
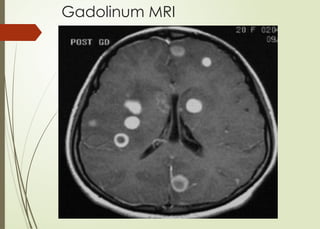
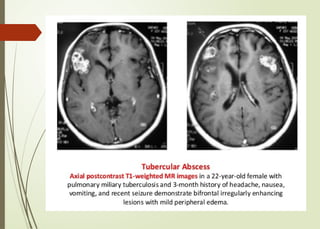
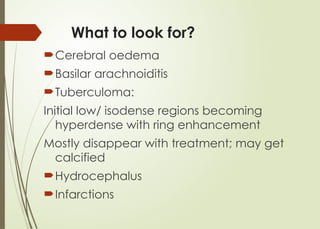
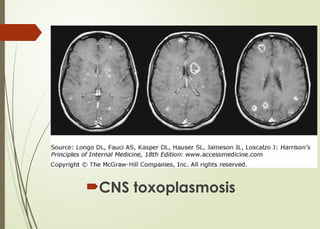
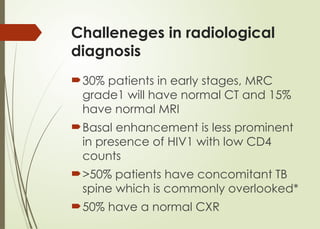
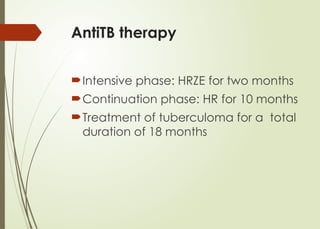
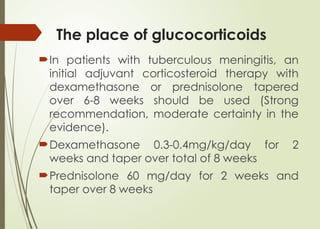
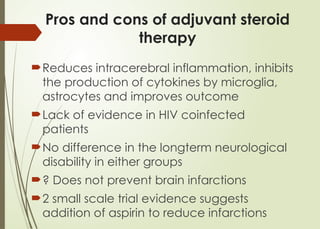
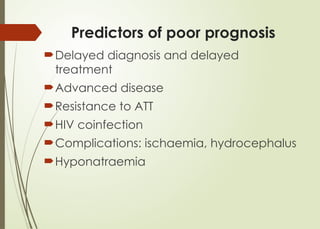
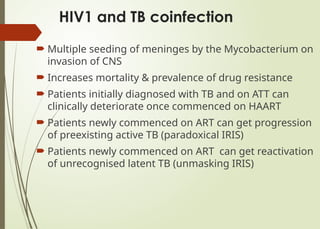
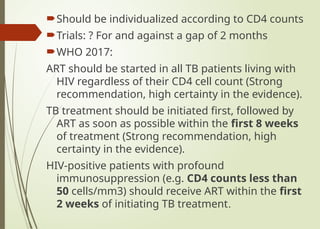
The document details the complexities surrounding central nervous system (CNS) tuberculosis, including its epidemiology, pathogenesis, clinical presentation, and diagnostic approaches. It emphasizes the rising incidence rates, particularly among vulnerable populations such as those co-infected with HIV, and outlines challenges in diagnosis and treatment. Recent advancements in drug therapy and recommendations from the World Health Organization (WHO) are discussed, indicating a critical need for timely diagnosis and treatment to improve patient outcomes.