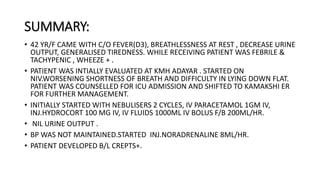
- 42 year old female housemaid presented with 3 days of fever and dry cough, and worsening shortness of breath.
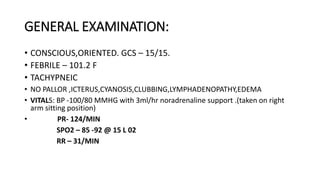
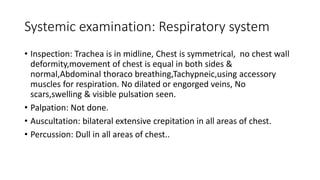
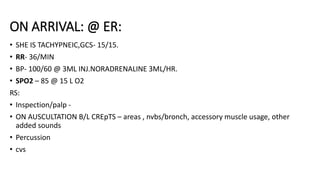
- On examination, she was febrile, tachypneic, and had bilateral crackles on lung auscultation.
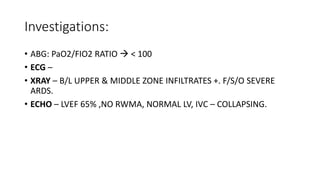
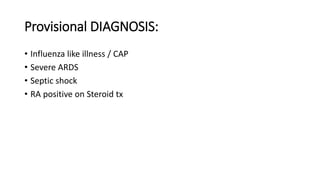
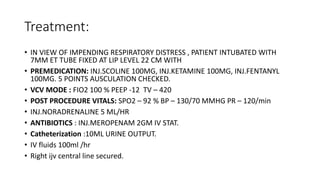
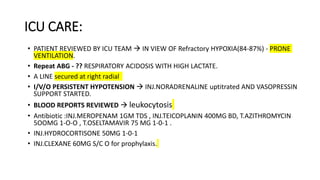
- Chest X-ray showed bilateral infiltrates consistent with severe ARDS. She was intubated and required multiple vasopressors and renal replacement therapy due to refractory shock. Her condition continued to deteriorate despite ECMO and she passed away on the third day.

![Chief complaints: HOPI
- Fever * 3 days
- Dry cough * 3 days
- Breathlessness since yesterday night.
Patient was apparently normal three days back & she developed fever which is low
grade, continuous type associated with cough which is dry not continuous not blood
stained and not associated with chills/rigor. After that She developed
breathlessness[MMRC III] since the night before ER Presentation, which was
progressive in nature and worsened since today morning. No relieving factor. H/o
generalized tiredness (+). H/o decrease urine output (~ 100 -200 ml)since yesterday
night.
HOPI:](https://image.slidesharecdn.com/casepresentationards-231218062720-b603e1a0/85/Case-presentation-ARDS-pptx-3-320.jpg)