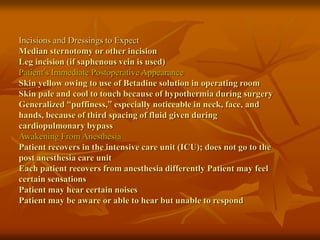
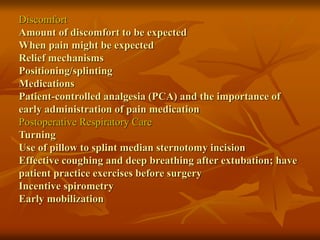
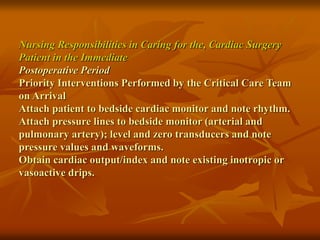
Cardiac surgery procedures like coronary artery bypass grafting and heart valve replacement are described. Postoperative complications involve decreased cardiac output, impaired tissue perfusion, impaired gas exchange, infections, and pain. Nursing assessments and interventions focus on hemodynamic monitoring, respiratory status, incision care, pain management, and health teaching about recovery.