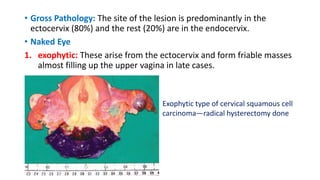
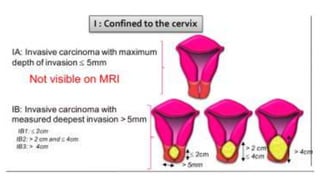
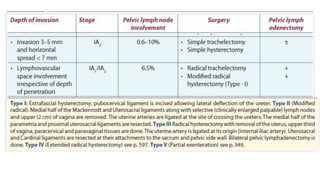
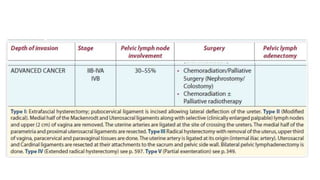
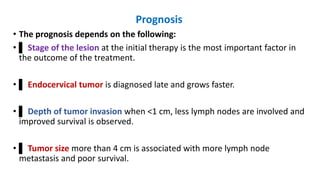
This document discusses cervical cancer, including its incidence, risk factors, diagnosis, staging, treatment, and prognosis in Bangladesh. It notes that cervical cancer rates are high in Bangladesh due to lack of screening and various social risk factors. Diagnosis involves examination, biopsy, and imaging. Staging follows the FIGO system and considers tumor size and spread. Treatment options include surgery, radiation, chemotherapy, or combinations. Prognosis depends on stage, tumor size and type, age, lymph node involvement, and HPV status.