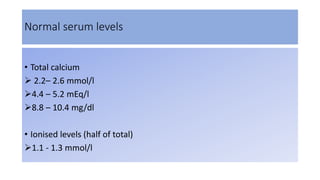
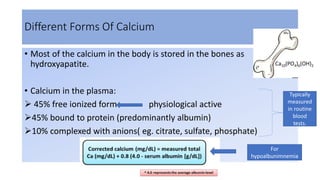
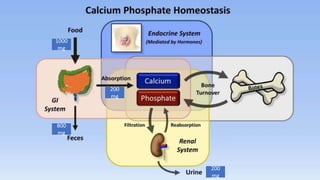
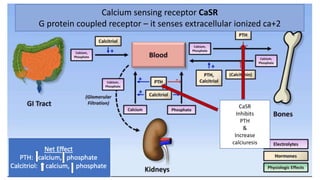
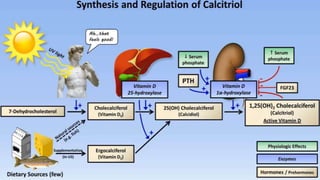
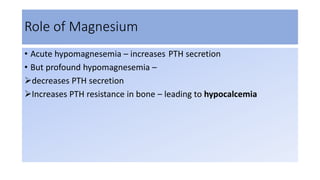
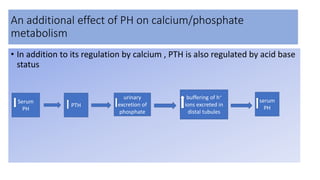
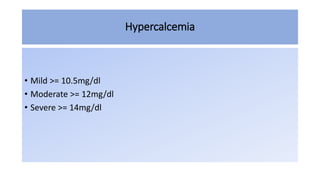
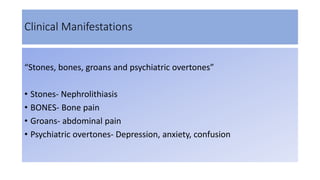
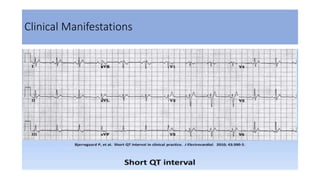
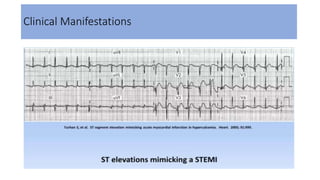
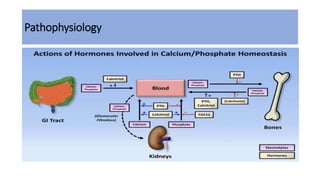
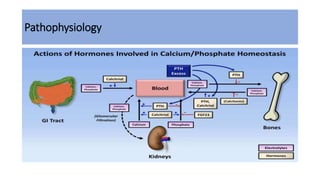
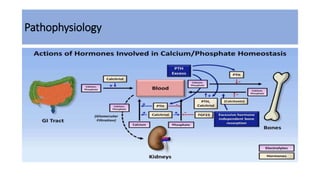
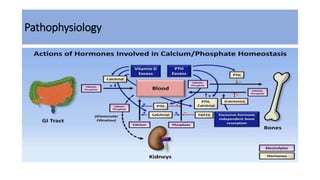
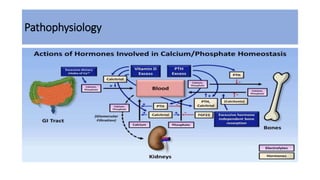
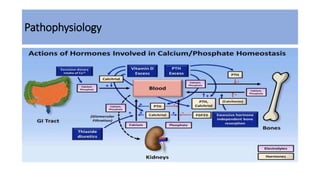
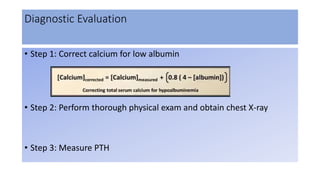
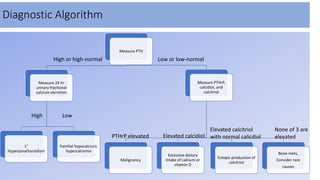
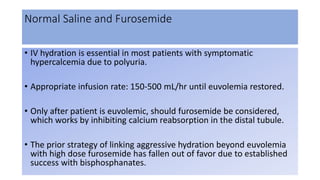
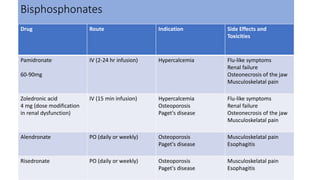
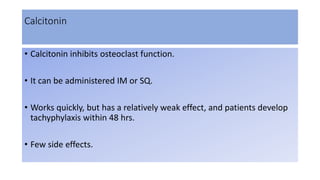
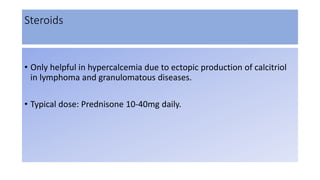
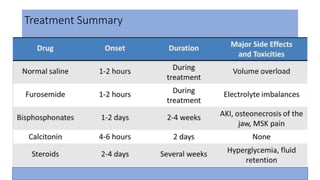
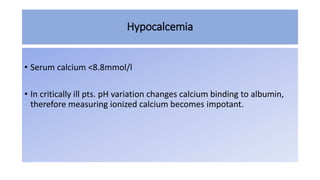
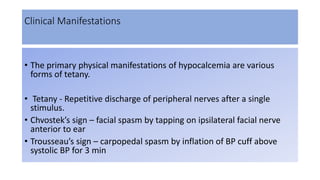
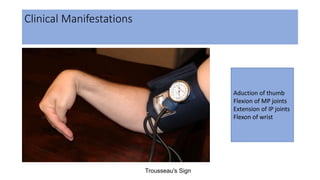
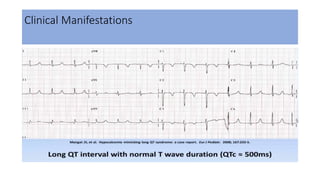
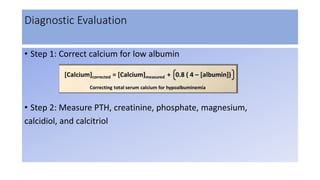
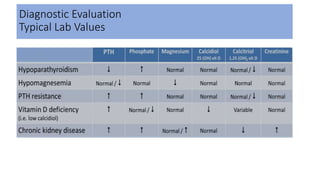
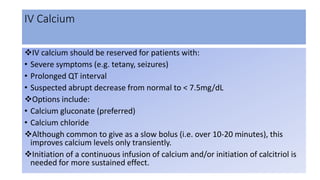
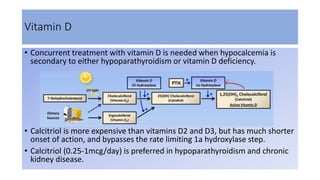
This document discusses hypercalcemia and hypocalcemia in the ICU. It covers the normal levels and functions of calcium, pathophysiology, clinical manifestations, diagnostic evaluation, and treatment options for hypercalcemia and hypocalcemia. The main treatment approaches for hypercalcemia include intravenous fluids, furosemide, bisphosphonates, calcitonin, and steroids. For hypocalcemia, treatment focuses on oral calcium, intravenous calcium, vitamin D, and magnesium supplementation.