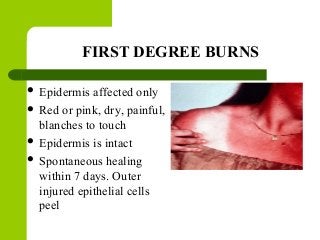
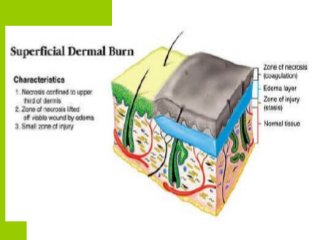
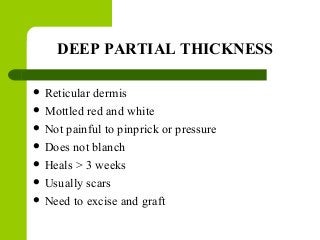
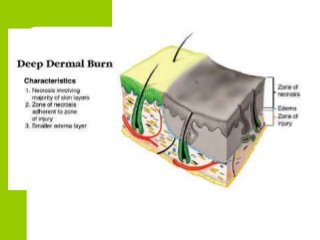
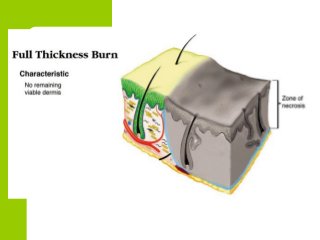
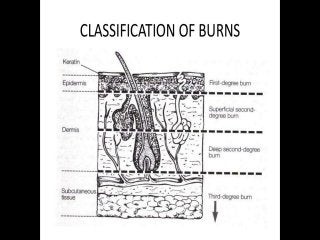
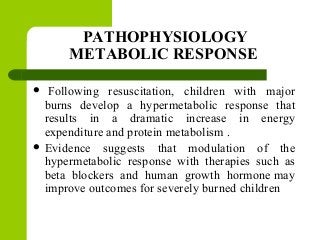
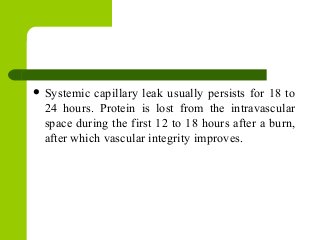
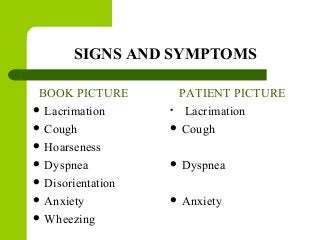
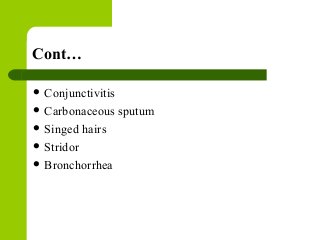
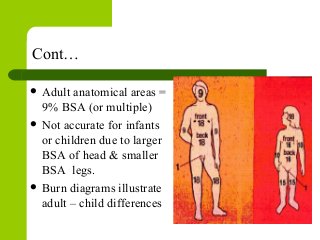
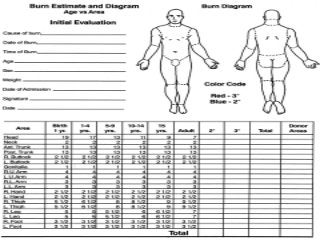
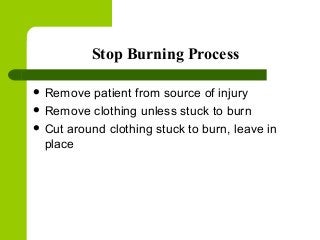
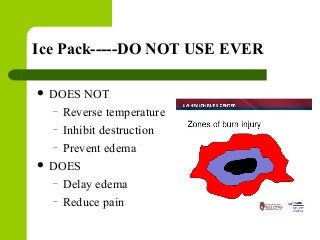
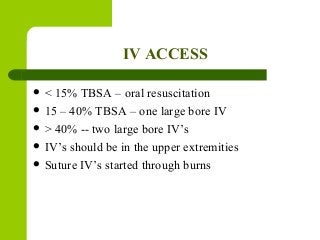
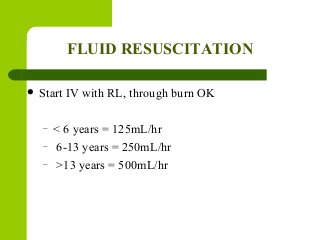
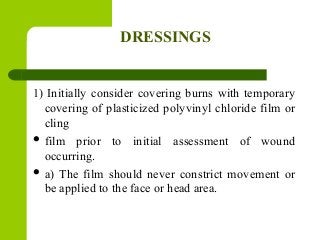
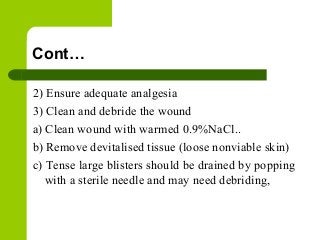
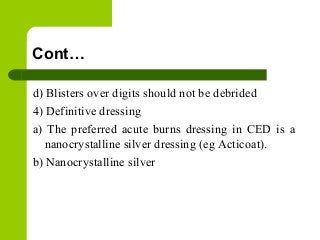
The document presents an overview of burn injuries in children, highlighting the types and classifications of burns, their causes, and the associated risks, particularly in young children. It emphasizes the need for prompt management and the significance of understanding burn depth, initial first aid, and medical treatment for various degrees of burns. The document concludes with nursing care theories and references for further reading on pediatric nursing related to burn care.