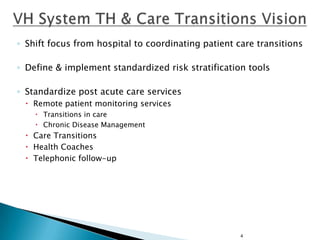
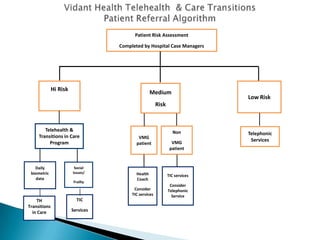
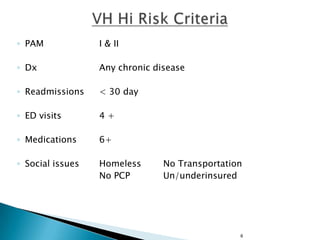
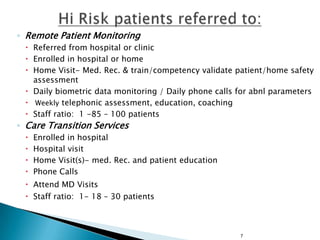
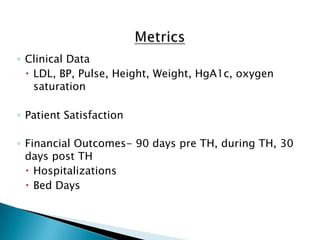
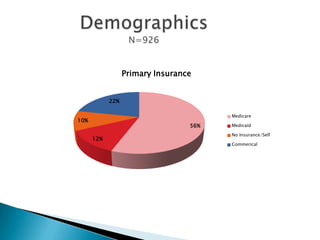
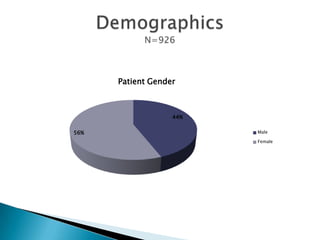
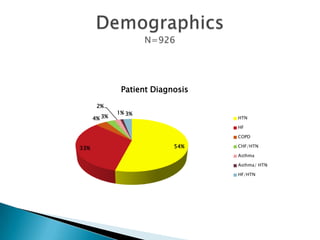
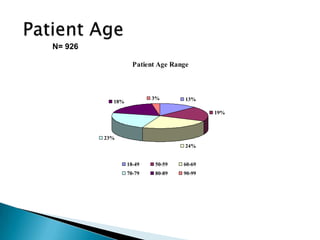
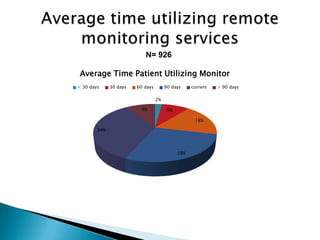
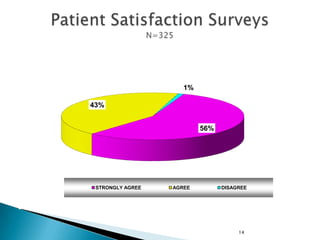
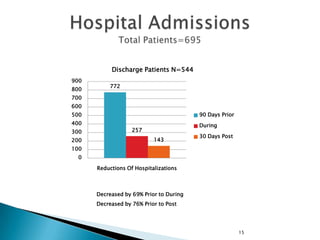
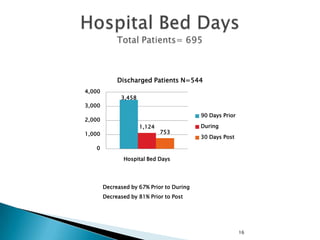
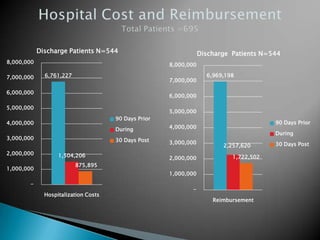
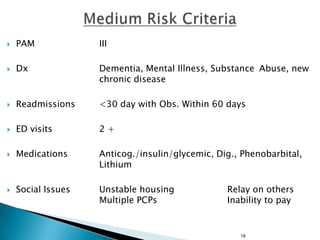
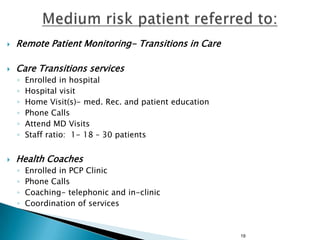
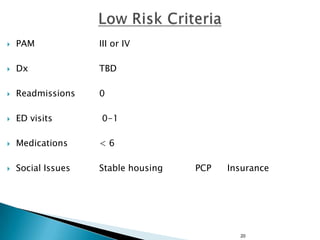
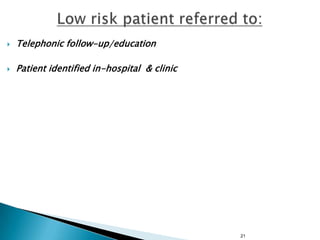
This document discusses Vidant Health's telehealth and care transitions program. It describes how the program aims to shift the focus from hospital care to coordinating patient care transitions. It outlines the risk stratification process used to determine which services patients receive, from remote patient monitoring and daily biometrics for high-risk patients, to telephonic follow-up for low-risk patients. It provides data on outcomes for patients in the program, showing reductions in hospitalizations, bed days, and costs after participating in the program.