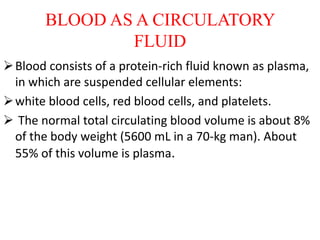
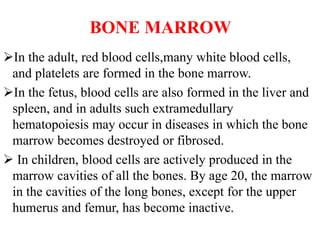
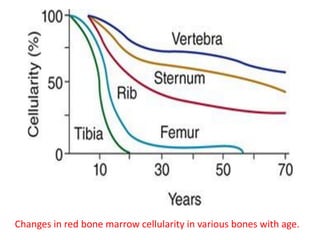
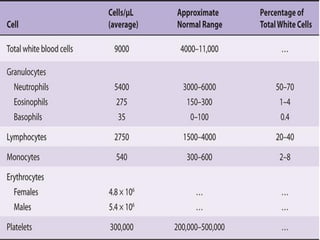
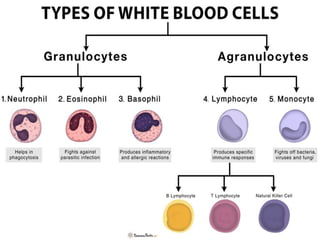
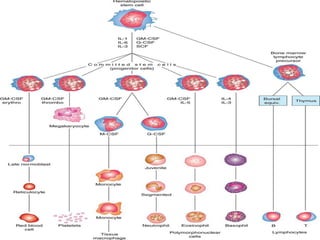
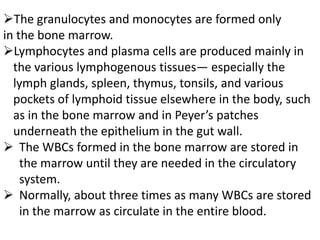
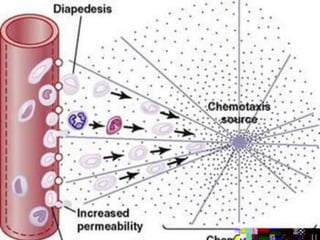
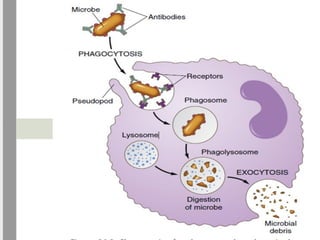
Blood consists of plasma and cellular elements including red blood cells, white blood cells, and platelets. Red blood cells, many white blood cells, and platelets are formed in the bone marrow from hematopoietic stem cells. There are several types of white blood cells including neutrophils, lymphocytes, monocytes, eosinophils, and basophils that provide defense against infection. White blood cells enter tissues from blood vessels to fight infection using mechanisms like phagocytosis, chemotaxis, and bactericidal agents.