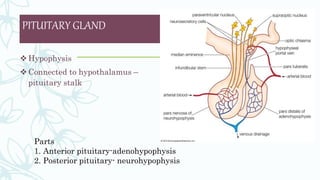
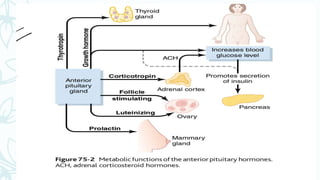
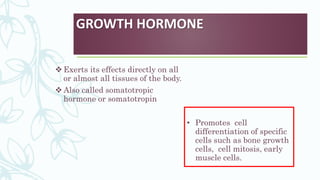
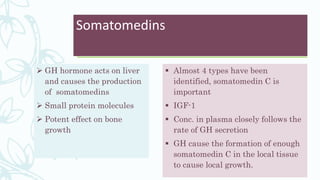
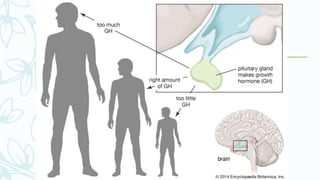
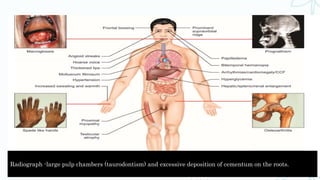
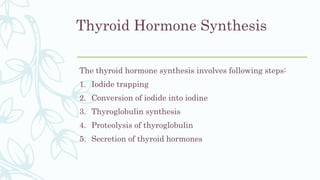
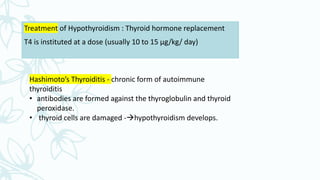
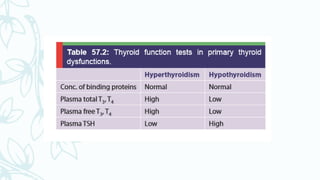
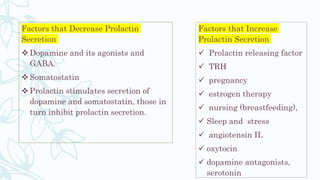
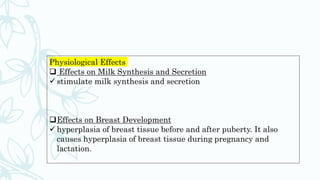
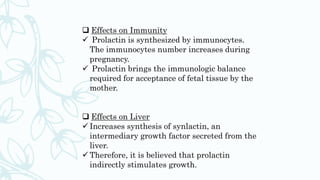
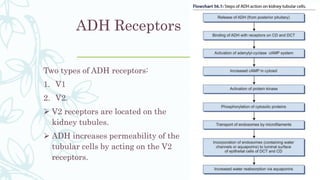
The document provides a comprehensive overview of endocrinology, detailing the hormone systems that regulate various bodily functions, including the roles of the pituitary gland and specific hormones like growth hormone and thyroid hormones. It discusses the physiological impacts of hormonal excess and deficiency, such as acromegaly, gigantism, and dwarfism, and their clinical manifestations and treatments. Additionally, it covers hormonal interactions, mechanisms of hormone action, and implications for dental health related to endocrine disorders.