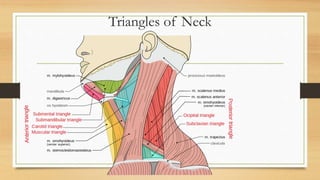
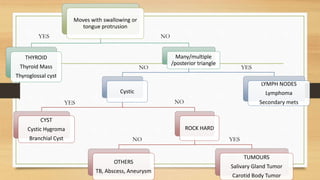
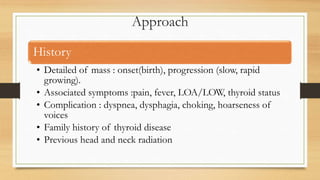
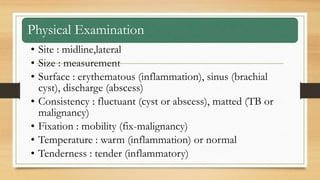
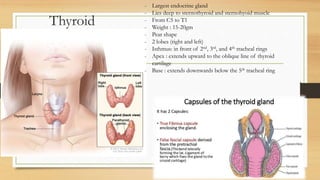
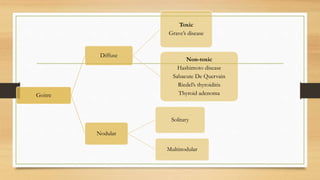
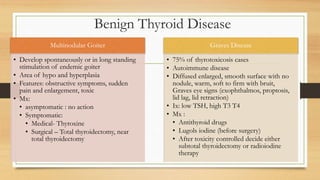
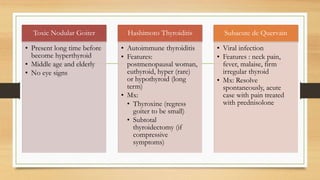
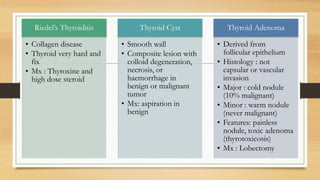
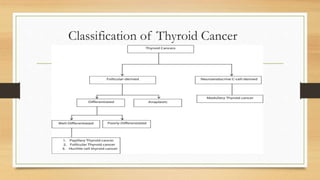
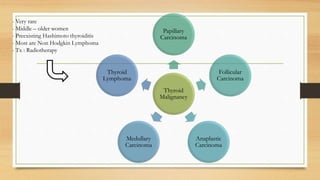
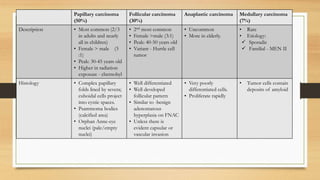
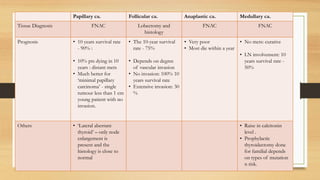
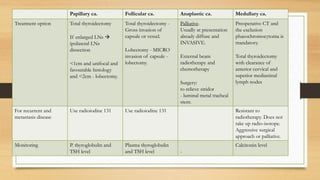
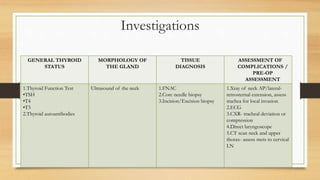
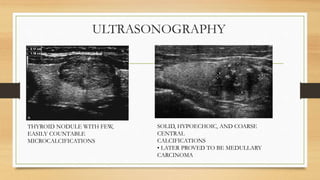
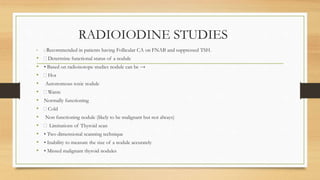
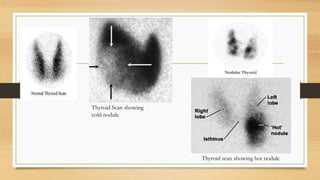
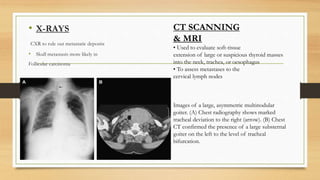
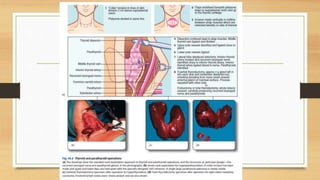
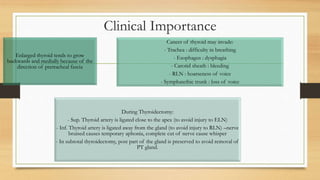
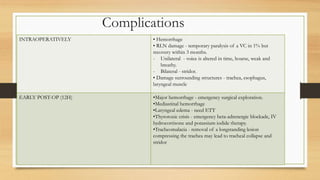
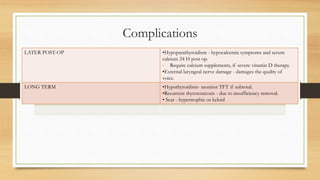
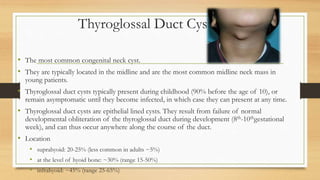
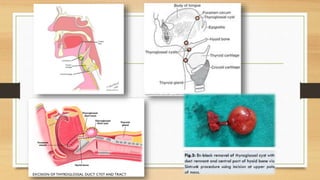
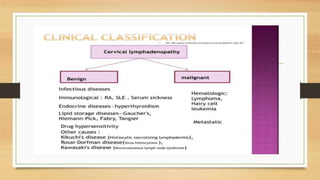
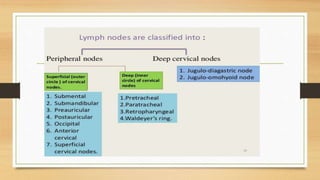
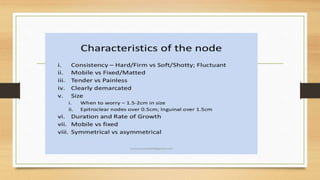
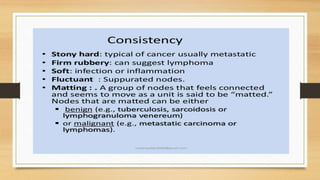
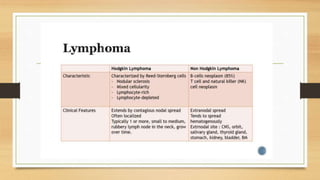
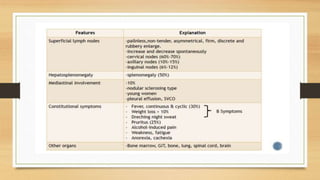
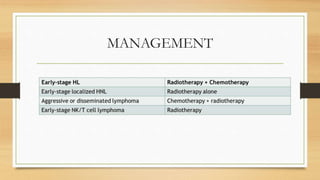
This document discusses neck swelling, including thyroid swelling and cervical lymph node swelling. It defines neck swelling as any congenital or acquired mass in the neck region. It describes the differential diagnoses and approach to evaluating neck swelling, focusing on thyroid swelling and cervical lymph nodes. Investigations like ultrasound, biopsy, and blood tests are discussed for evaluating the cause of neck swelling, whether benign thyroid conditions, thyroid cancer, infections, or other issues. The importance of properly diagnosing and treating neck lumps is emphasized.