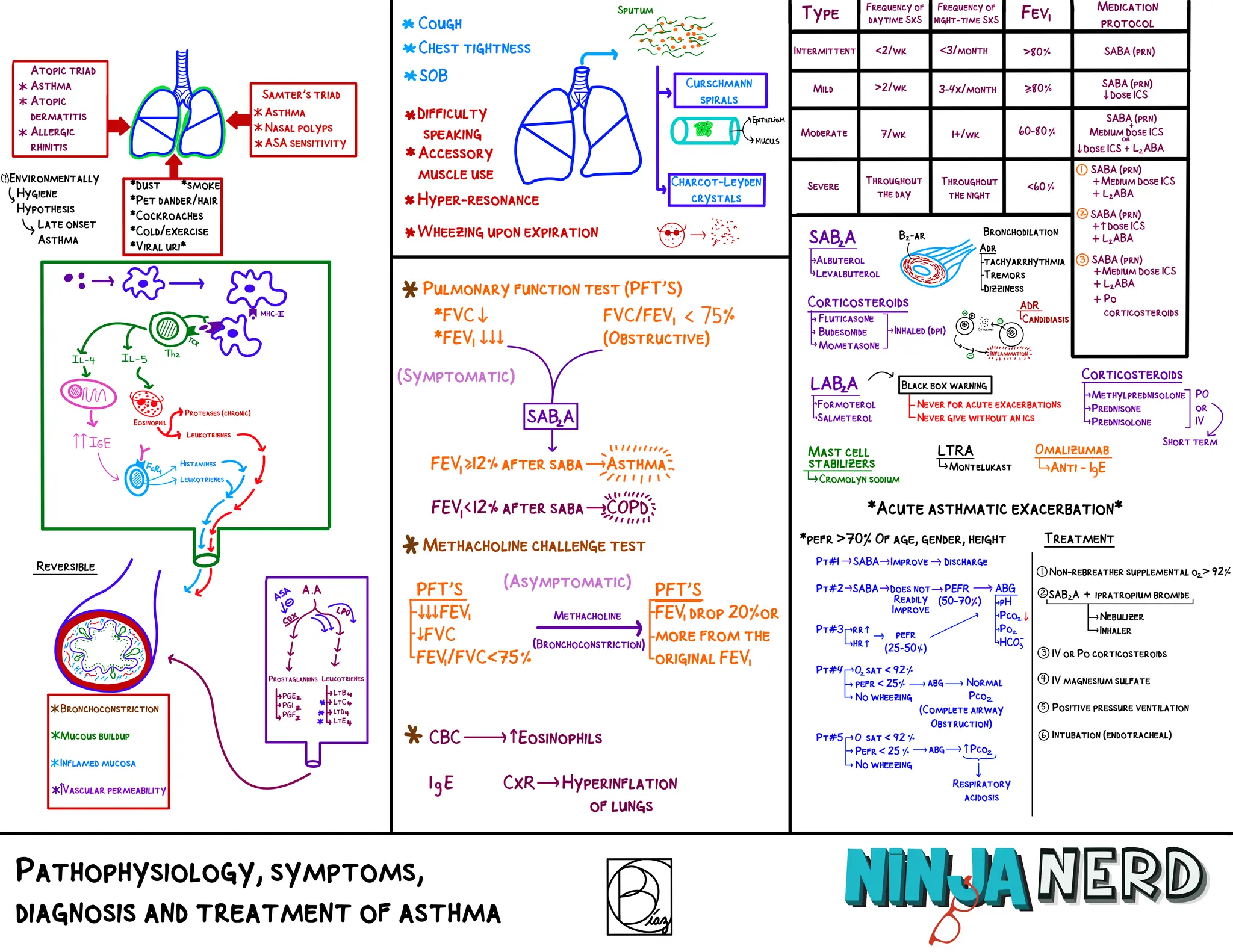
The document discusses the pathophysiology, symptoms, diagnosis, and treatment of asthma, including triggers like dust and pet dander. It details the use of various medications such as bronchodilators and corticosteroids, as well as protocols for managing acute asthma exacerbations. Diagnostic measures like pulmonary function tests and assessment of symptoms are emphasized for effective asthma management.