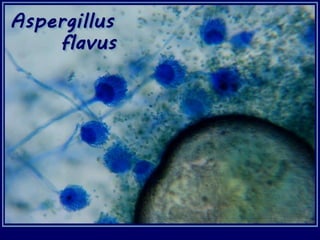
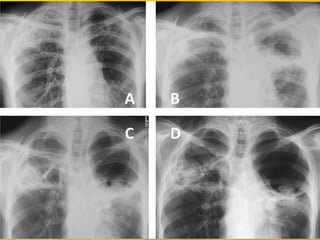
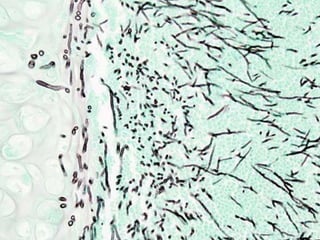
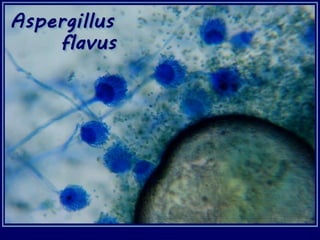
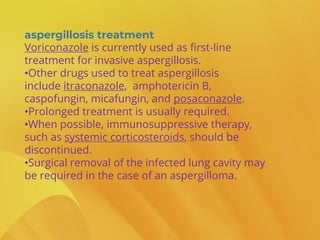
Aspergillus is a common environmental fungus that can cause disease in humans under certain conditions. It is commonly inhaled, but usually does not cause illness in healthy individuals. However, in people with weakened immune systems, it can infect the lungs and spread throughout the body. The most common types of aspergillosis are acute invasive infection, allergic reaction, aspergilloma (fungus ball), and chronic necrotizing pulmonary infection. Diagnosis involves culturing samples, biopsy, or imaging tests. Voriconazole is usually the first-line treatment, along with surgery in some cases. Risk can be reduced by avoiding dusty areas and using protective masks.