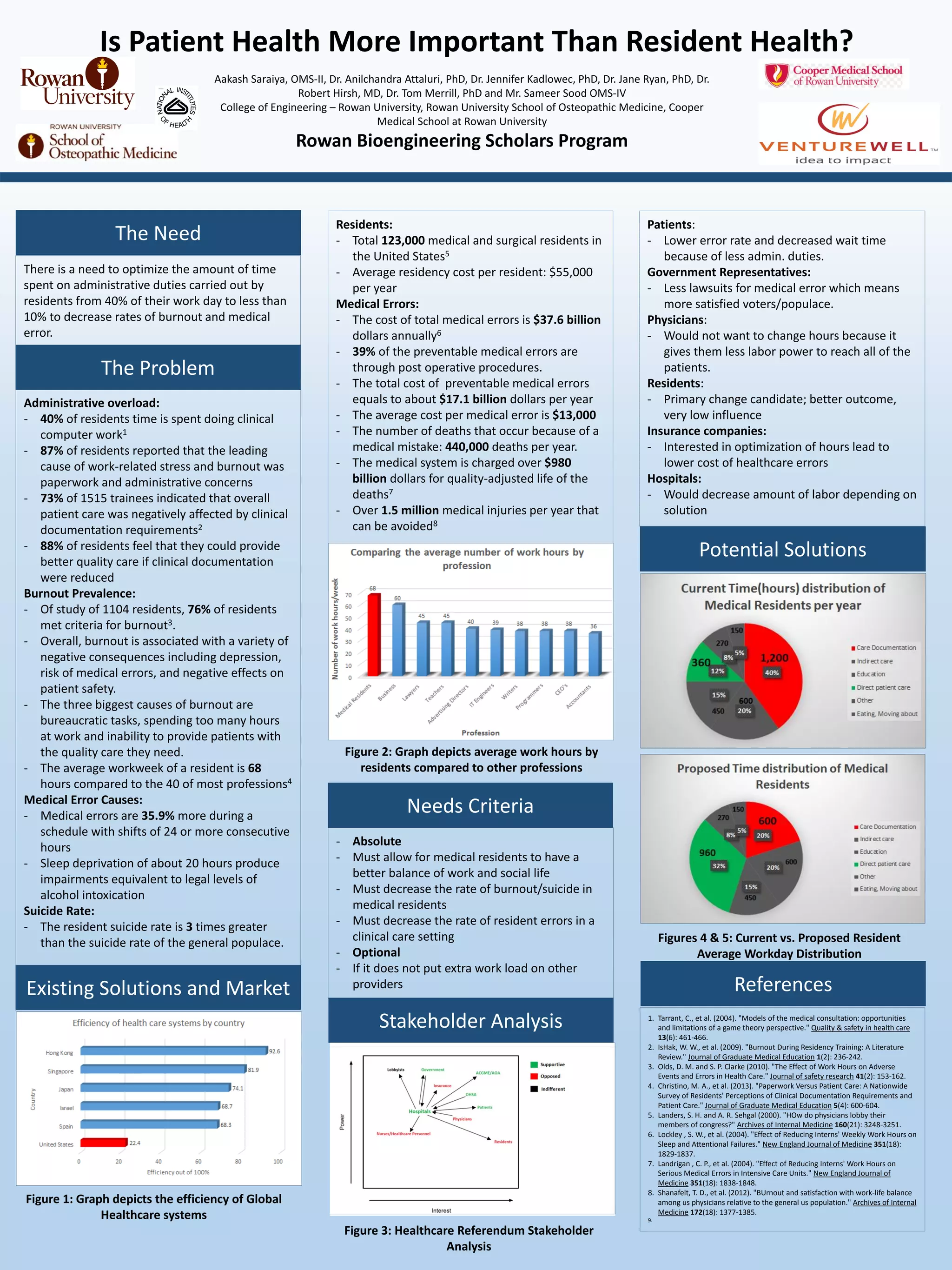
There is a need to reduce the amount of time medical residents spend on administrative duties from 40% of their workday to less than 10% in order to decrease rates of burnout, medical error, and improve patient care. Existing solutions have not adequately addressed this problem. The average workweek for residents is 68 hours compared to 40 for most other professions, and administrative tasks are a leading cause of work-related stress and burnout for residents. This can negatively impact patient safety and outcomes, as burnout and long work hours are associated with increased medical errors. Finding a solution that reduces administrative burdens on residents could decrease error rates, improve work-life balance and quality of care.