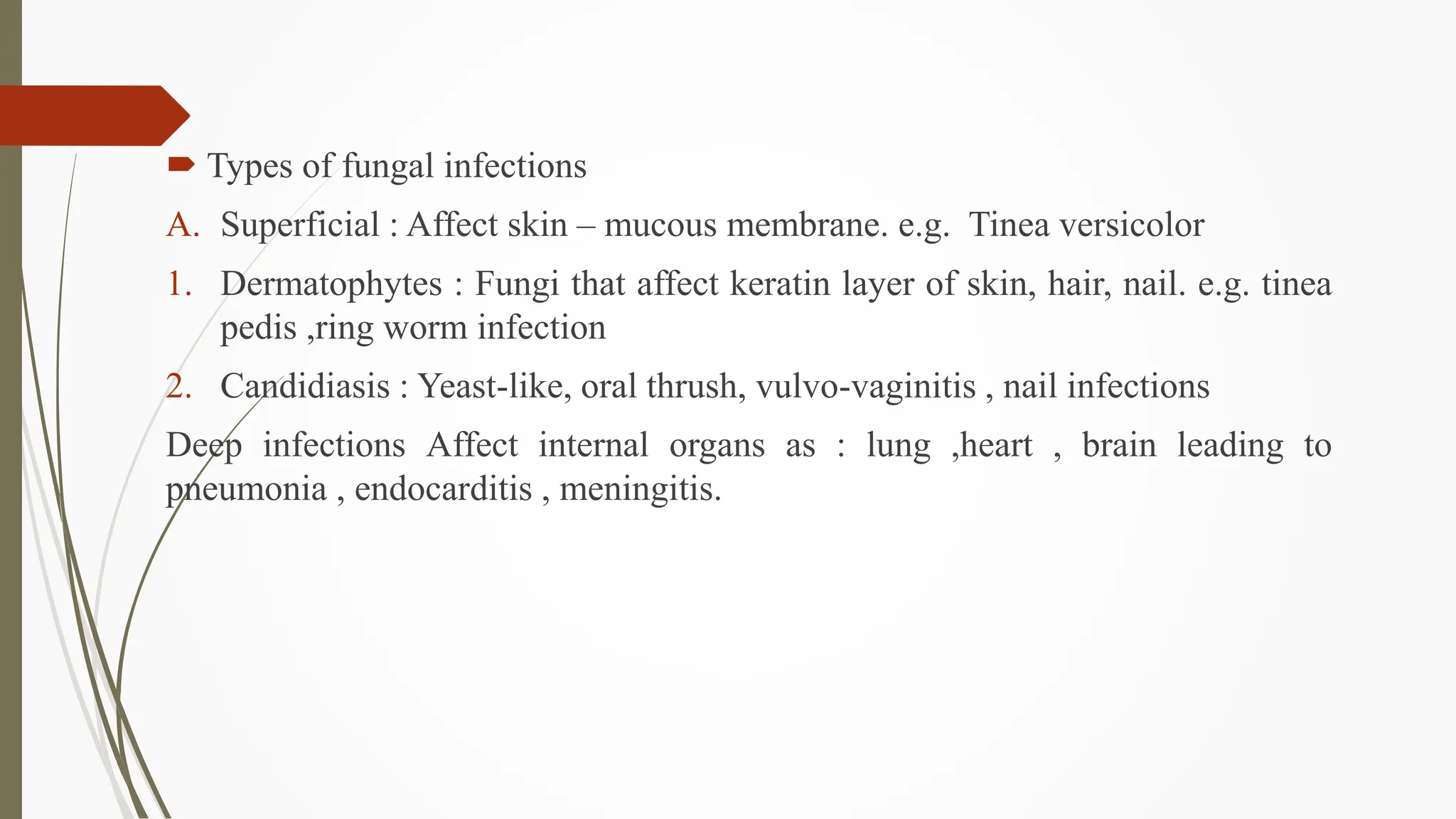
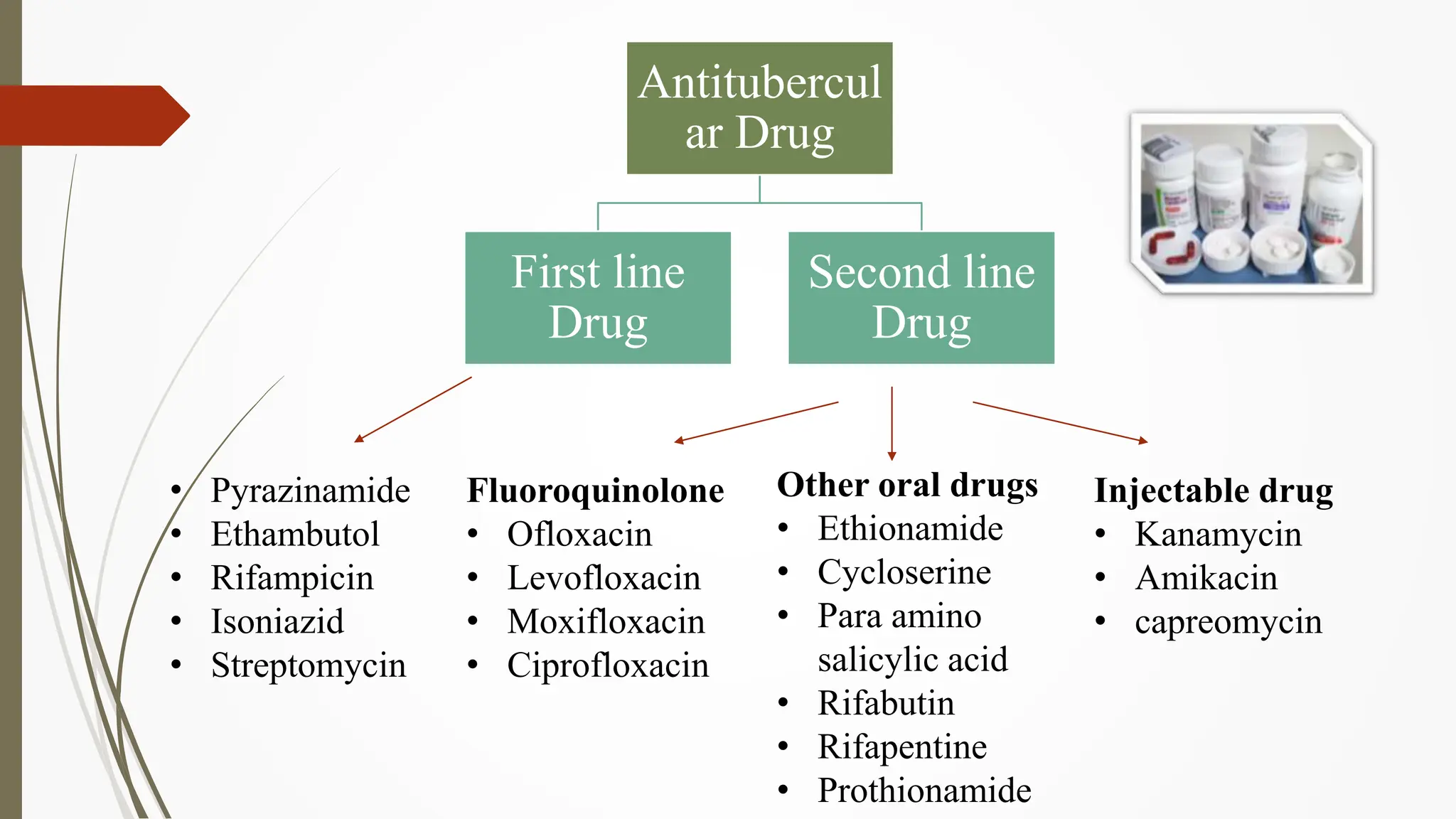
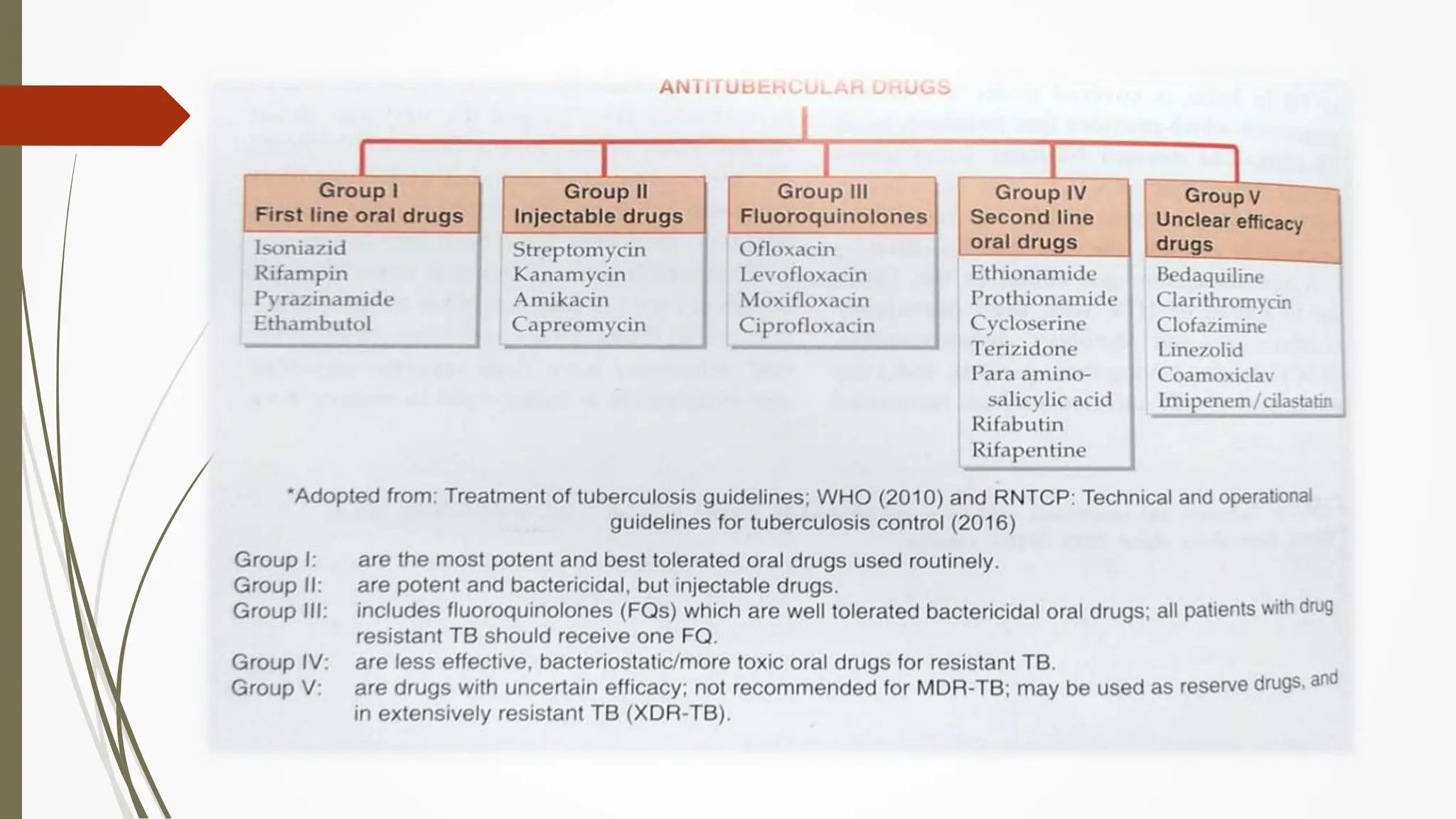
This document provides an overview of antifungal and anti-tuberculosis drugs, discussing their mechanisms, classifications, effects, and clinical uses. It covers various types of fungal infections and treatments, including polyenes, azoles, and echinocandins, as well as tuberculosis management with first and second-line drugs. The content emphasizes the importance of combination therapies and highlights emerging challenges such as multidrug-resistant tuberculosis.





























![First line drug :
1. Isoniazid [INH]
It is a prodrug activated by catlase peroxidase (coded by KatG), Active
metabolite Inhibits the enzyme ketoenoylreductase (coded by inh A) required
for mycolic acid synthesis, an essential component of mycobacterial cell wall.
It is the single dose important drug used in TB (Drug of choice for TB)
It is the drug of choice for prophylaxis of tuberculosis.
It cause peripheral neuritis that can be prevented and treated by
Pyridoxine(Vitamin B)
ISONIAZIDE
CONVERTED TO
ACTIVE FORM
INHIBIT THE
SYNTHESUS OF
MYCOLIC ACID
COMPONENT OF
MYCOBACTERIUM
CELL WALL
DEATH
OF
BACTER
IA
INSIDE
MYCOBACTERIA](https://image.slidesharecdn.com/antifungalandanti-tb-240318105431-dec0e45e/75/ANTIFUNGAL-AND-ANTI-TUBERCULOSIS-DRUGS-WITH-CLASSIFICATION-34-2048.jpg)