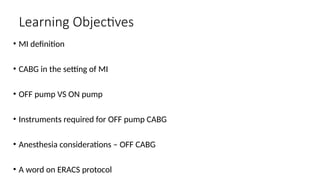
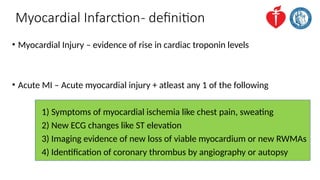
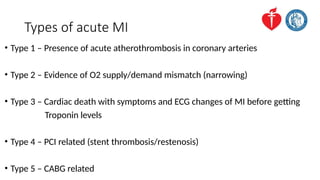
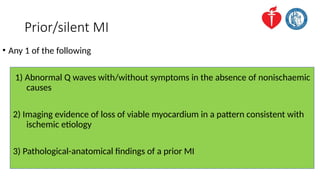
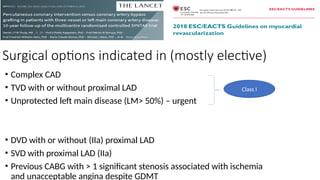
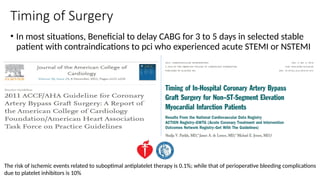
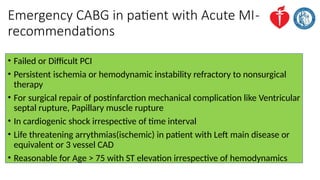
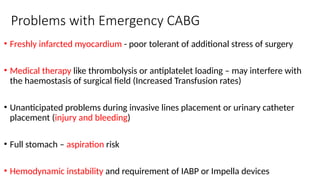
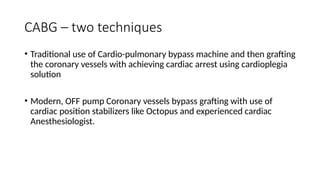
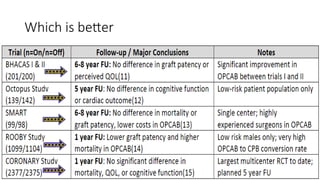
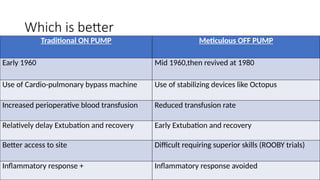
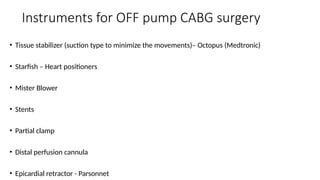
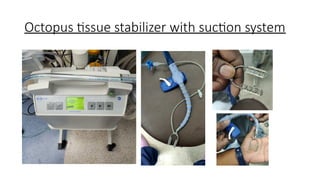
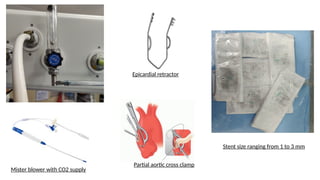
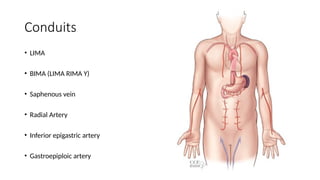
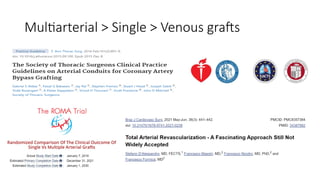
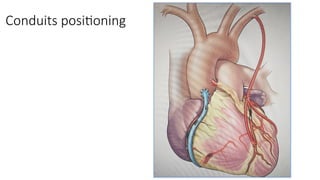
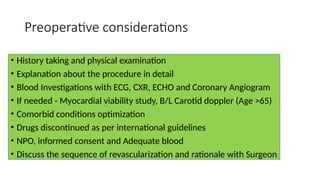
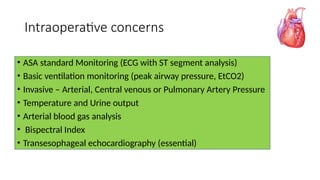
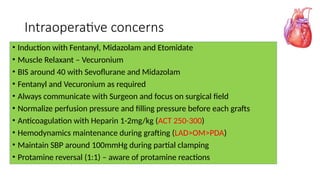
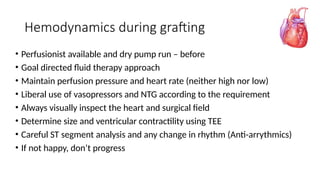
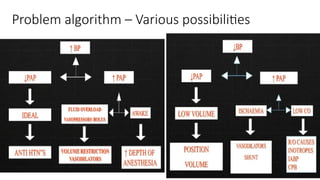
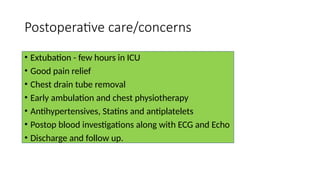
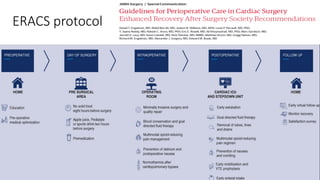
The document reviews anesthesia management for myocardial infarction (MI) patients undergoing coronary artery bypass grafting (CABG) surgery, emphasizing definitions, types of MI, and surgical options. It discusses anesthesia considerations for both on-pump and off-pump techniques, along with required instruments, intraoperative monitoring, and postoperative care. Additionally, it highlights the importance of patient management, including preoperative evaluations, intraoperative concerns, and adherence to the Enhanced Recovery After Cardiac Surgery (ERACS) protocol.