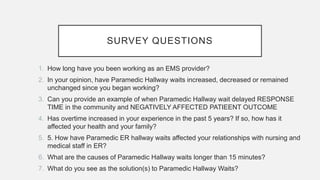
This document summarizes the results of a survey of EMS providers in Alberta about ambulance offload delays. It finds that overtime has increased significantly for EMS workers in the last 5 years, negatively impacting their health and families. Offload delays have led to delayed response times for emergencies, in some cases with negative patient outcomes like death. The primary causes of delays are lack of hospital beds and lengthy triage times. Recommended solutions include improving hospital patient flow, building long-term care facilities, and allowing EMS to leave once patients are handed over to the hospital.