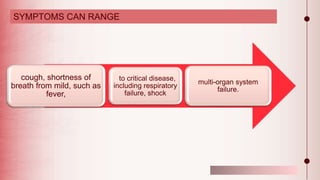
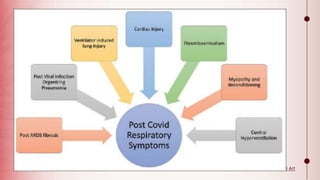
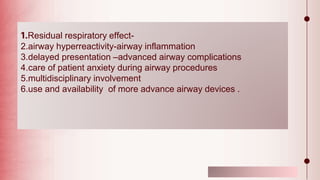
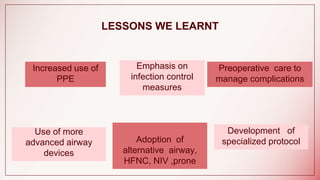
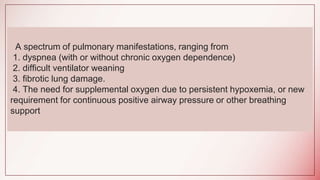
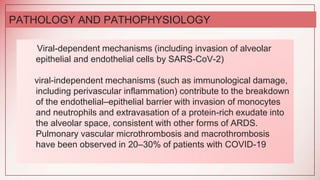
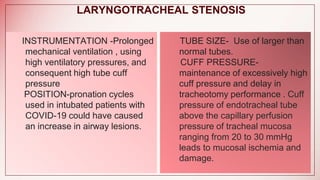
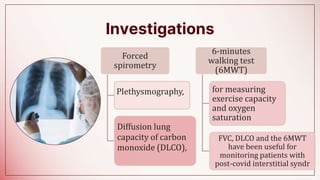
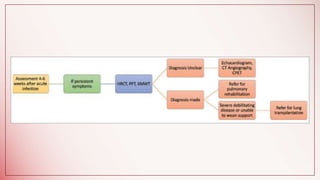
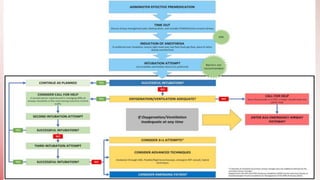
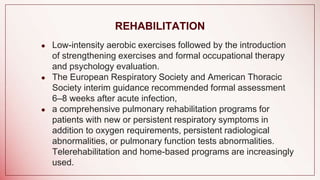
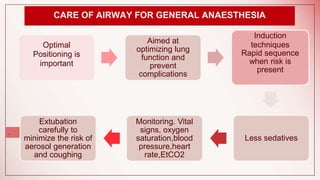
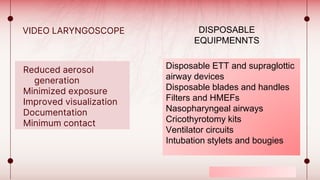
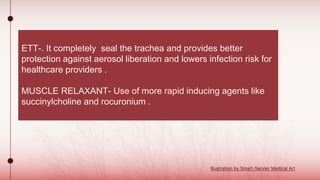
The document discusses changes to airway management in the post-COVID pandemic era. It notes that COVID-19 often leads to respiratory complications and sequelae. Some key points discussed include: increased use of protective equipment and infection control measures during airway procedures; adoption of alternative techniques like HFNC and NIV; training on specialized post-COVID airway management protocols; and monitoring patients for long-term effects like pulmonary fibrosis using tests like CT scans and pulmonary function tests. The challenges of potential increased airway injuries and need for multidisciplinary care are also addressed.