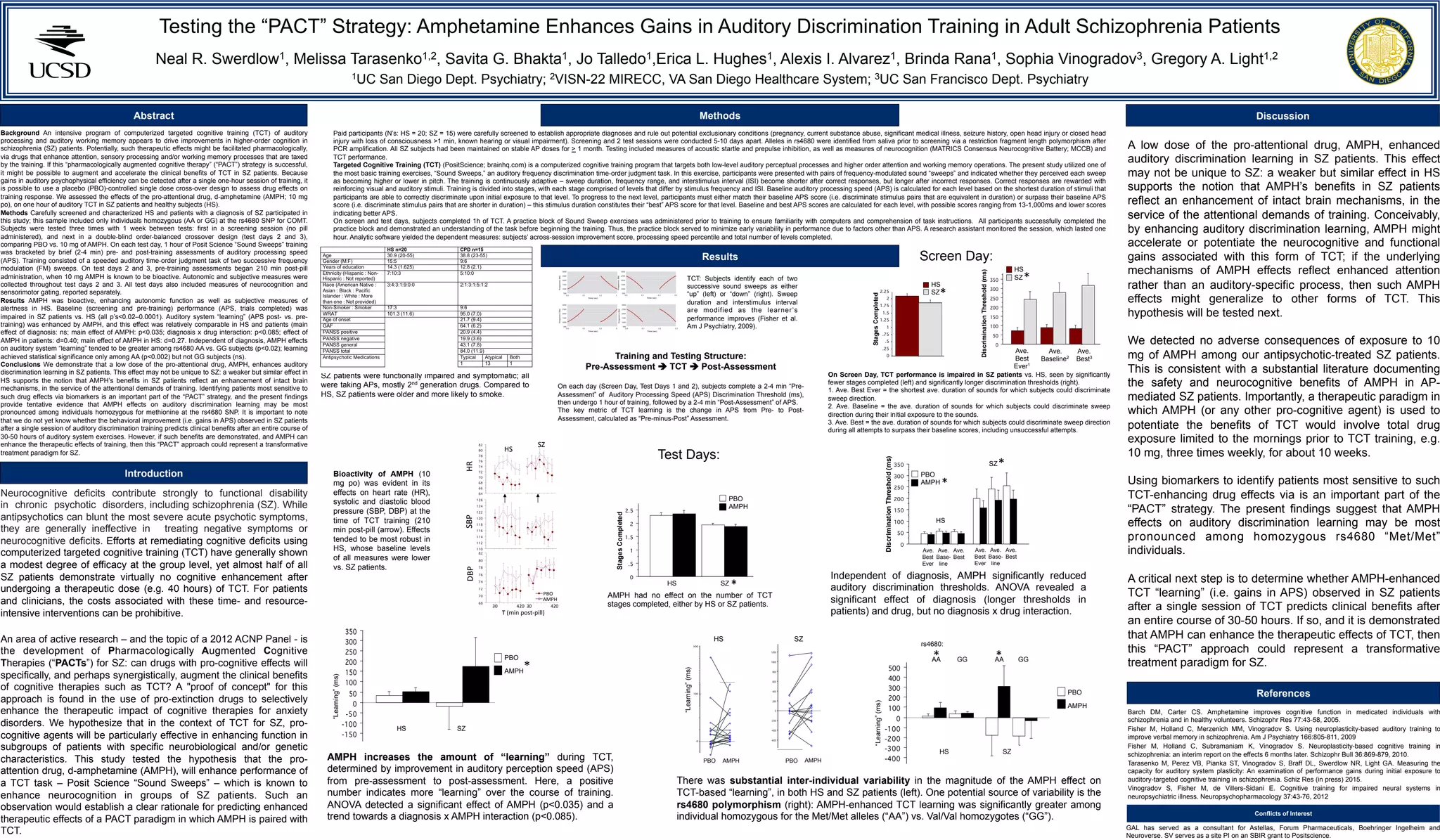
This study tested whether the drug d-amphetamine (AMPH) could enhance performance on an auditory discrimination training task in schizophrenia patients and healthy subjects. Participants completed one hour of "Sound Sweeps" training, which was designed to improve auditory processing speed. Training was completed after receiving either AMPH or a placebo. AMPH enhanced auditory learning in both patients and healthy subjects, as measured by greater improvements in auditory processing speed from pre- to post-training. This effect was greater in schizophrenia patients and in subjects with a specific genotype. The results provide preliminary evidence that AMPH may augment the effects of targeted cognitive training and accelerate neurocognitive gains in schizophrenia patients.