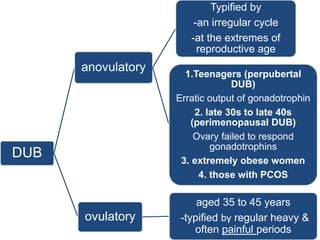
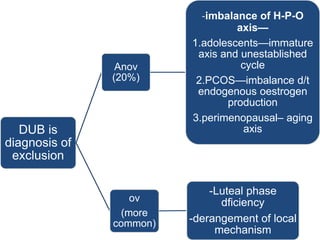
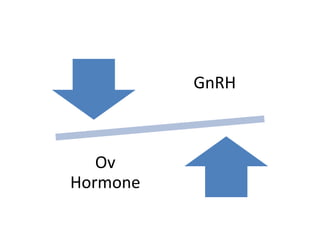
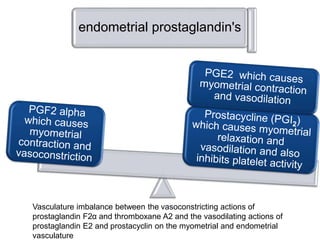
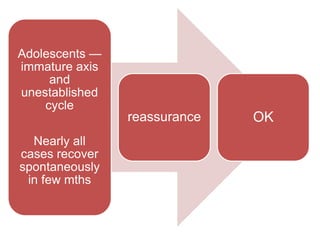
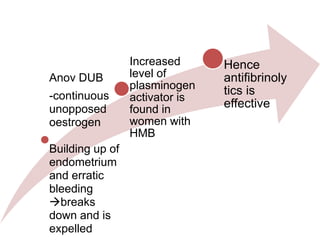
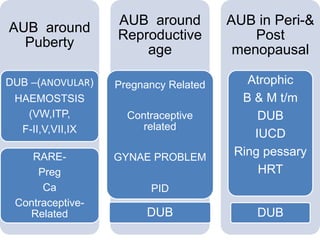
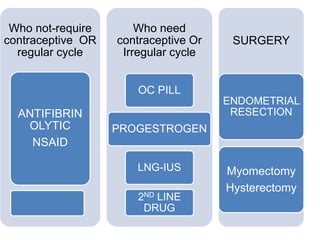
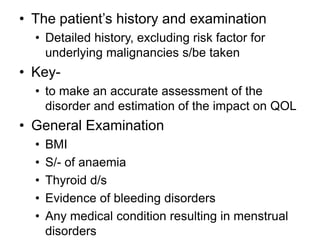
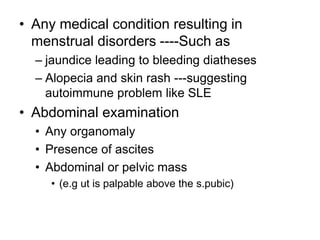
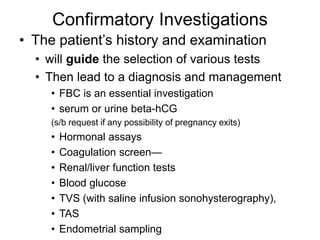
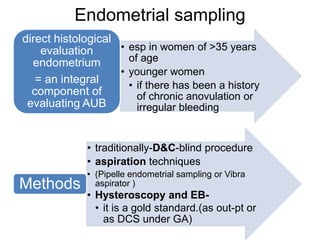
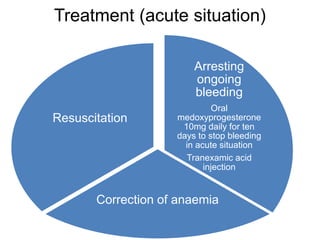
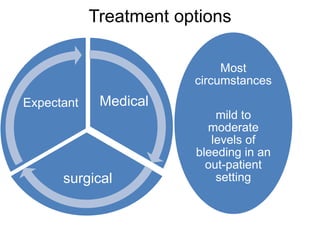
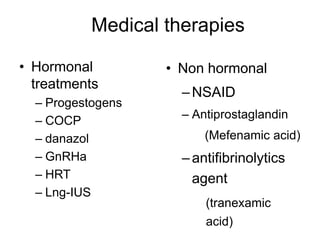
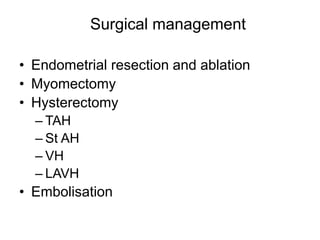
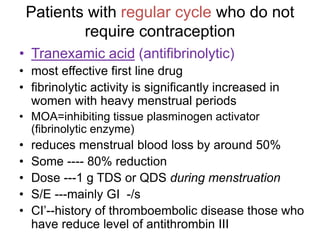
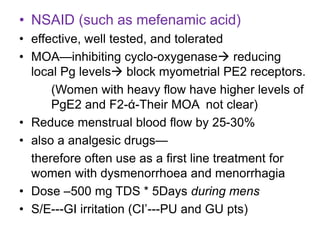
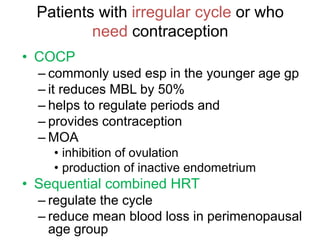
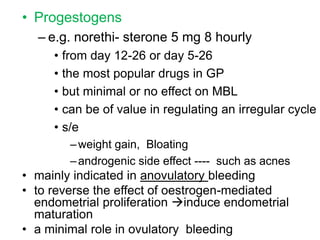
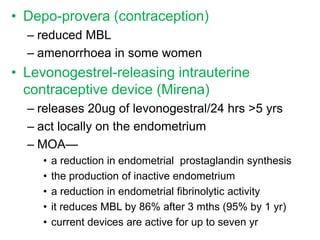
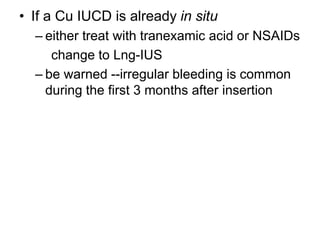
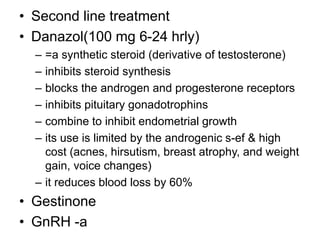
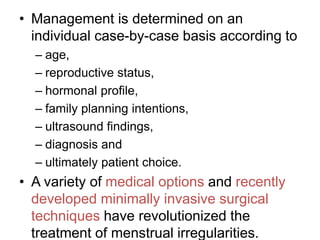
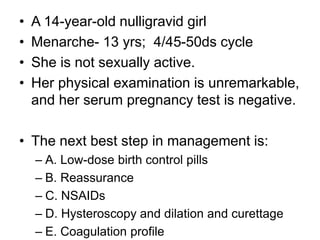
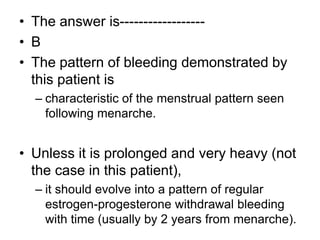
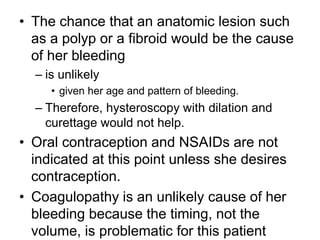
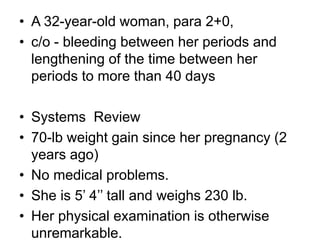
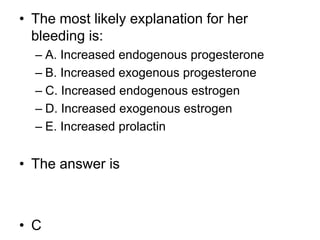
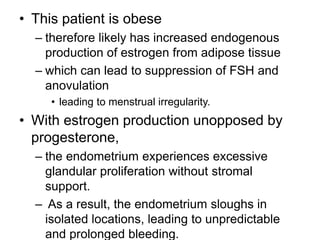
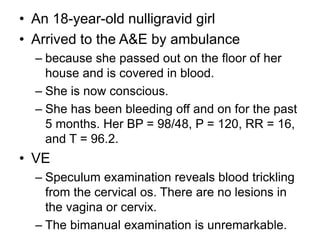
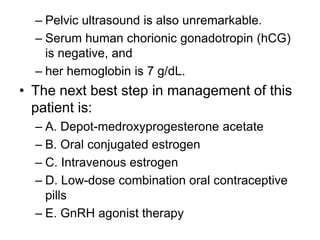
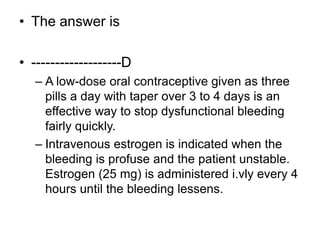
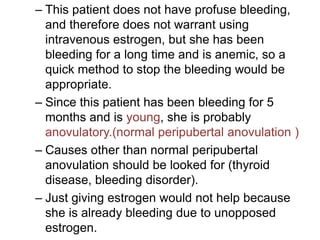
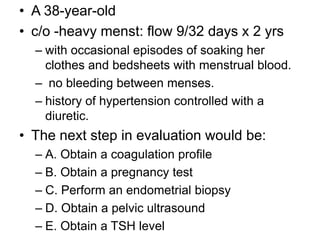
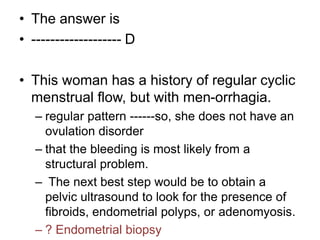
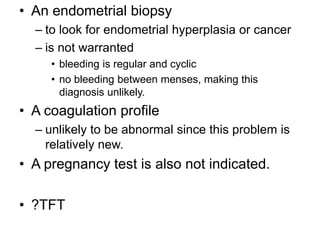
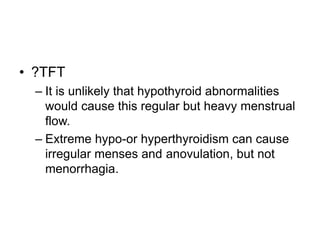
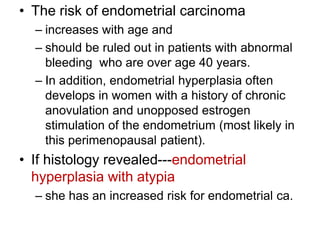
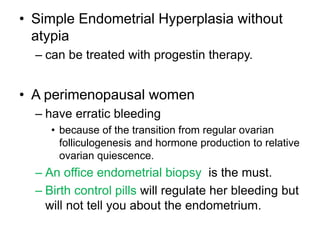
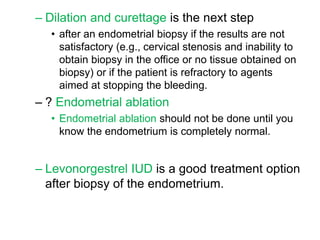
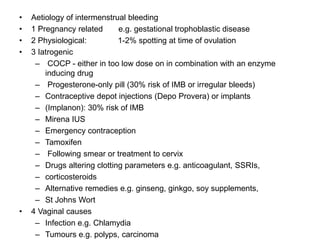
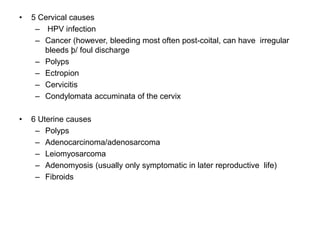
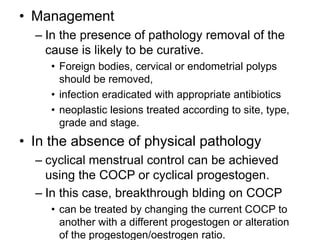
This document summarizes the management of abnormal uterine bleeding. It discusses various causes including organic local causes, systemic causes, and non-organic dysfunctional uterine bleeding. For dysfunctional bleeding, it describes anovulatory types seen in teenagers, late 30s to 40s, and extremely obese women, as well as ovulatory types seen in women aged 35 to 45. Evaluation and treatment options are also summarized, including medical treatments like hormones and NSAIDs, and surgical procedures. Management is tailored to each individual case based on various factors.