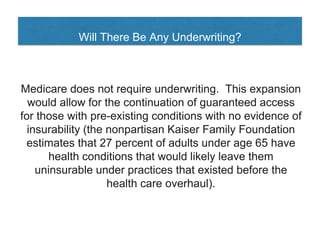
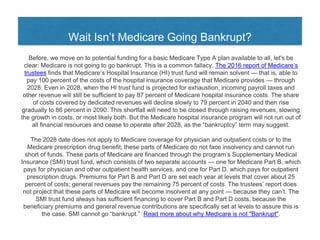
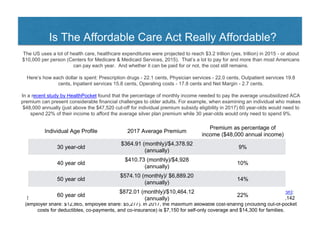
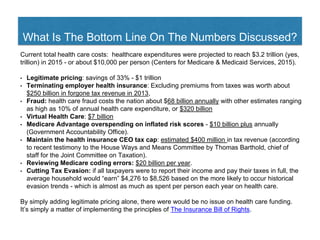
The document outlines proposed solutions to improve the U.S. health insurance system, focusing on Medicare expansion and the challenges of access, cost, and quality. It highlights the existing complexities of health coverage post-Affordable Care Act and suggests using Medicare as a baseline to address issues such as emergency care and prescription drug coverage. The recommendations emphasize simplifying health insurance while ensuring everyone has basic, affordable coverage without pre-existing condition exclusions.