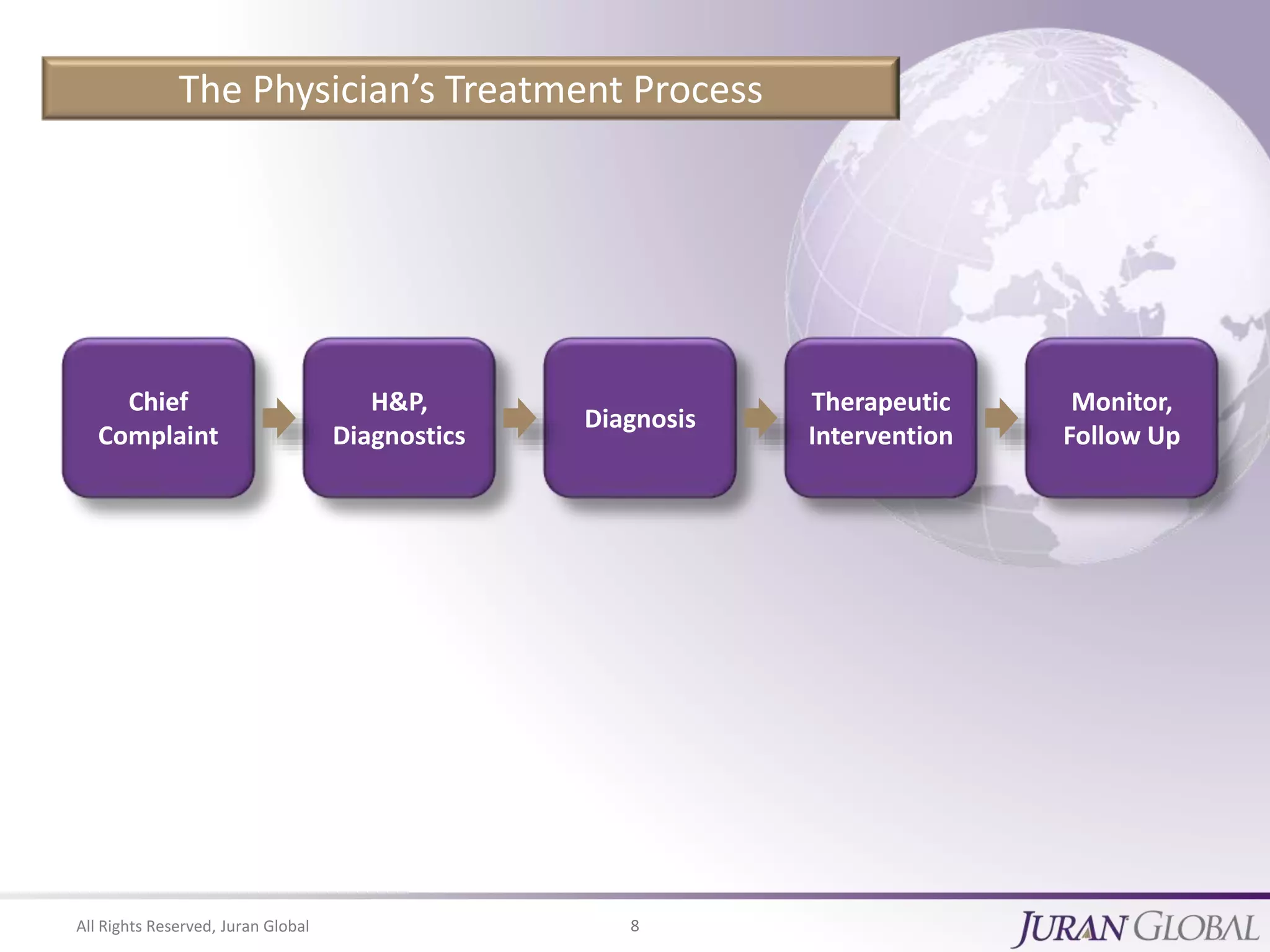
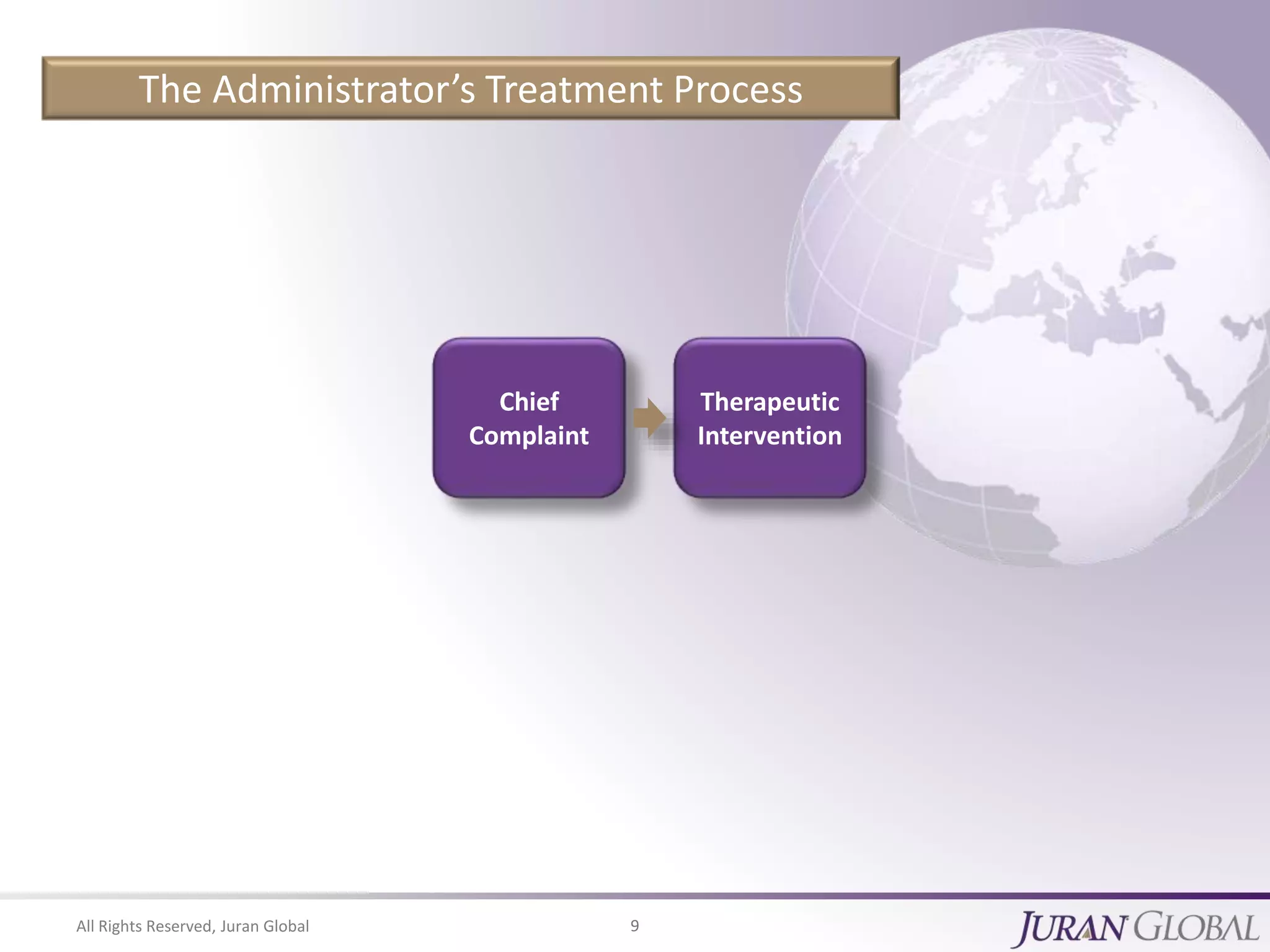
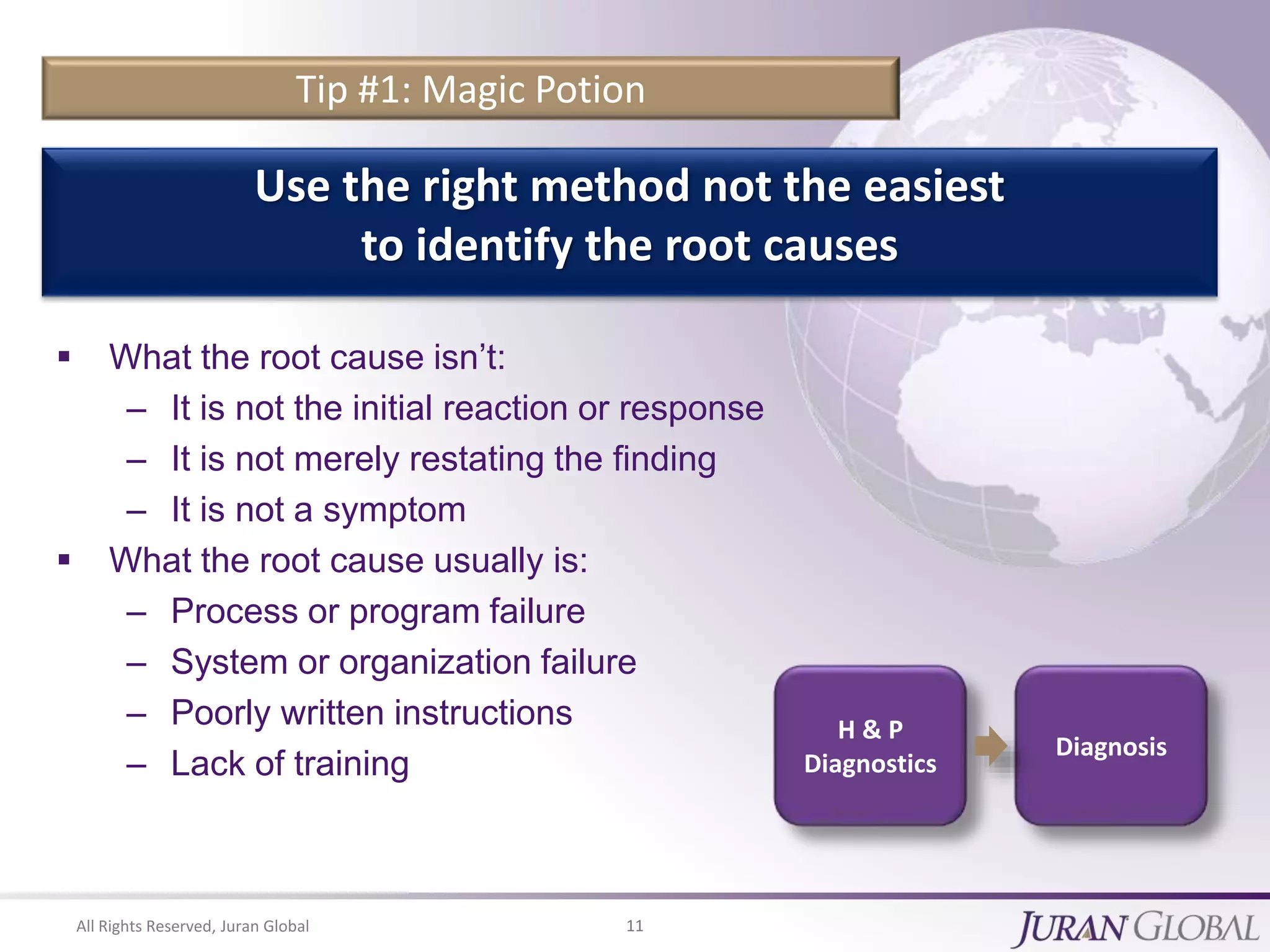
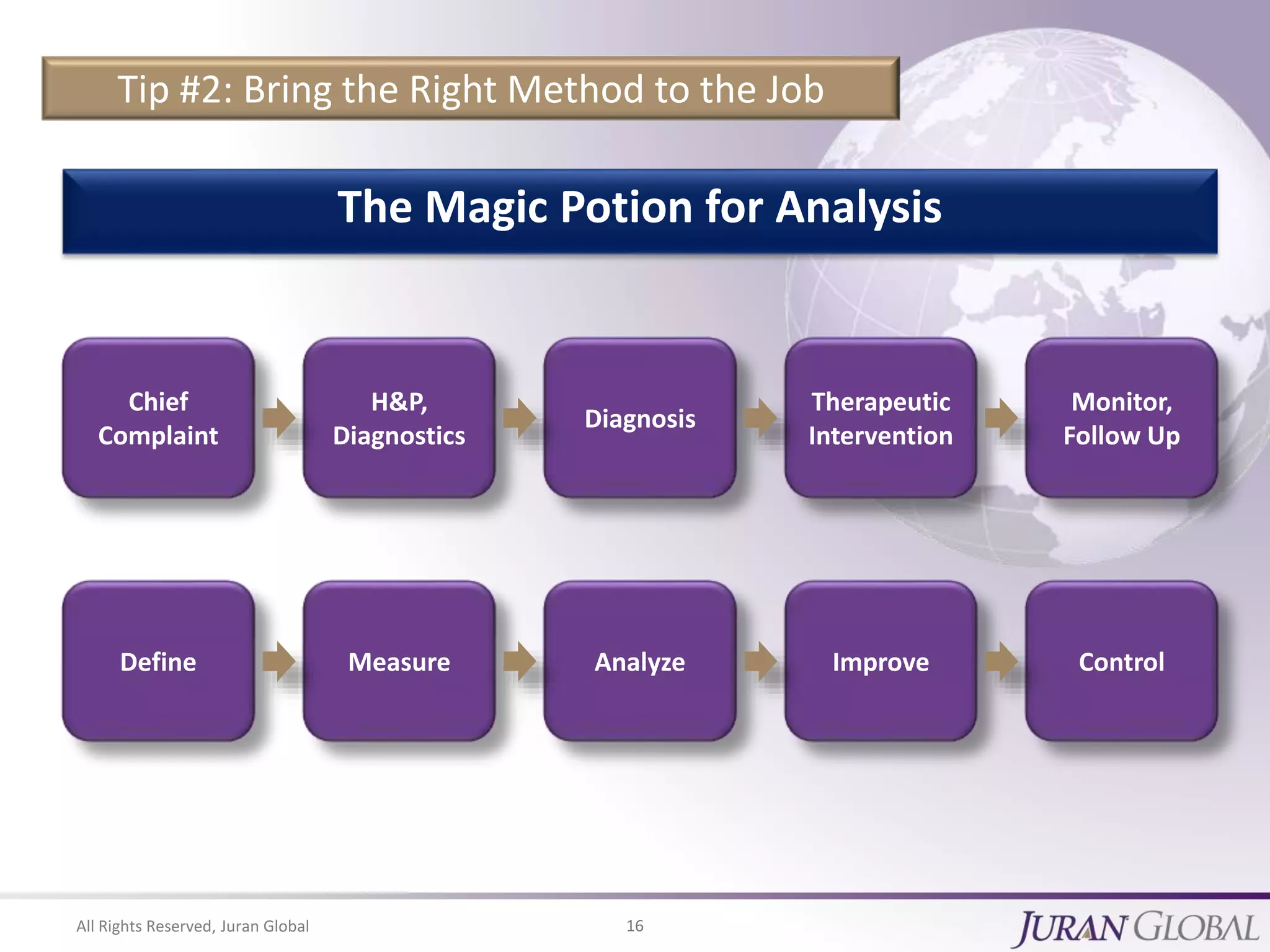
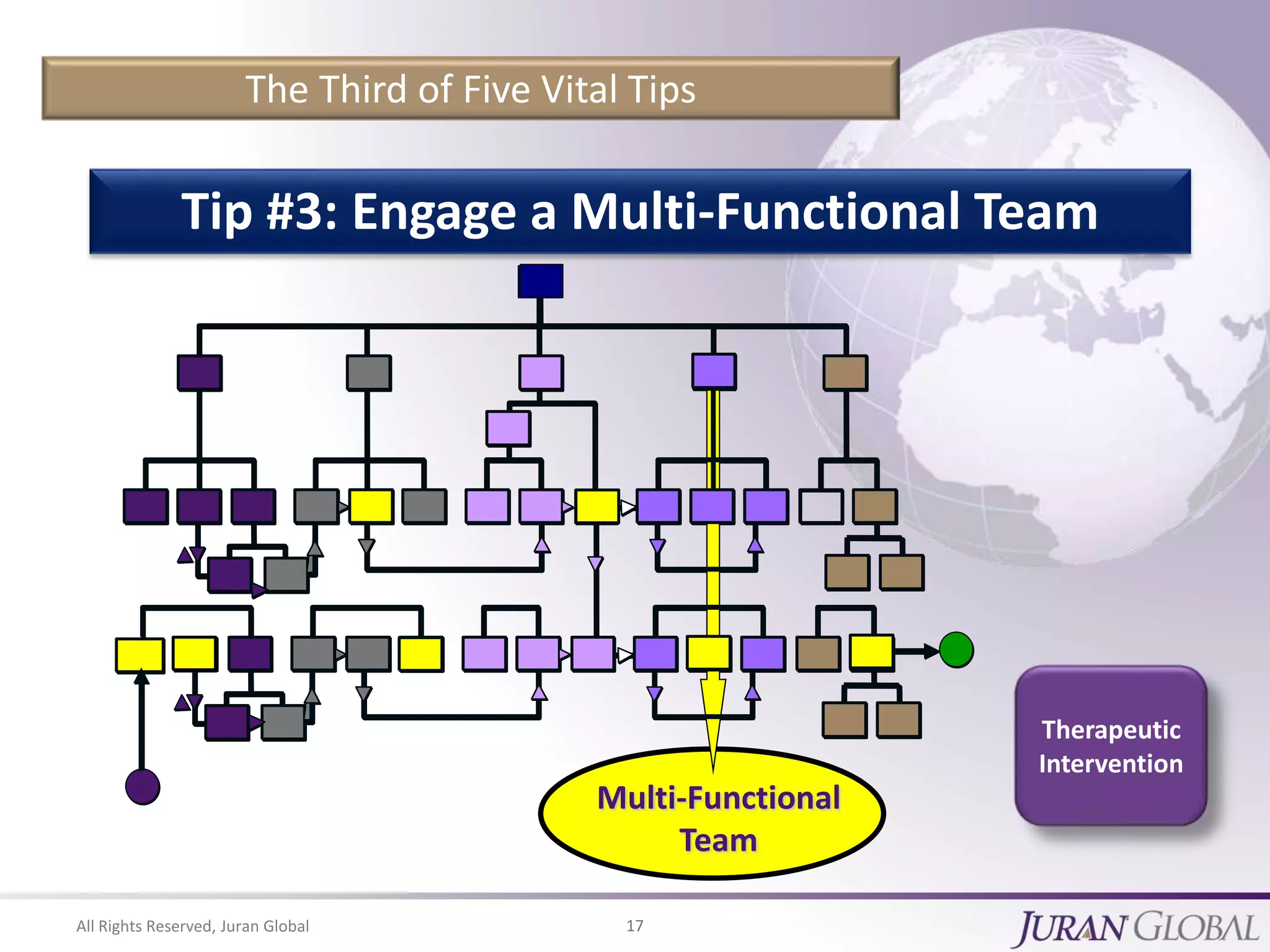
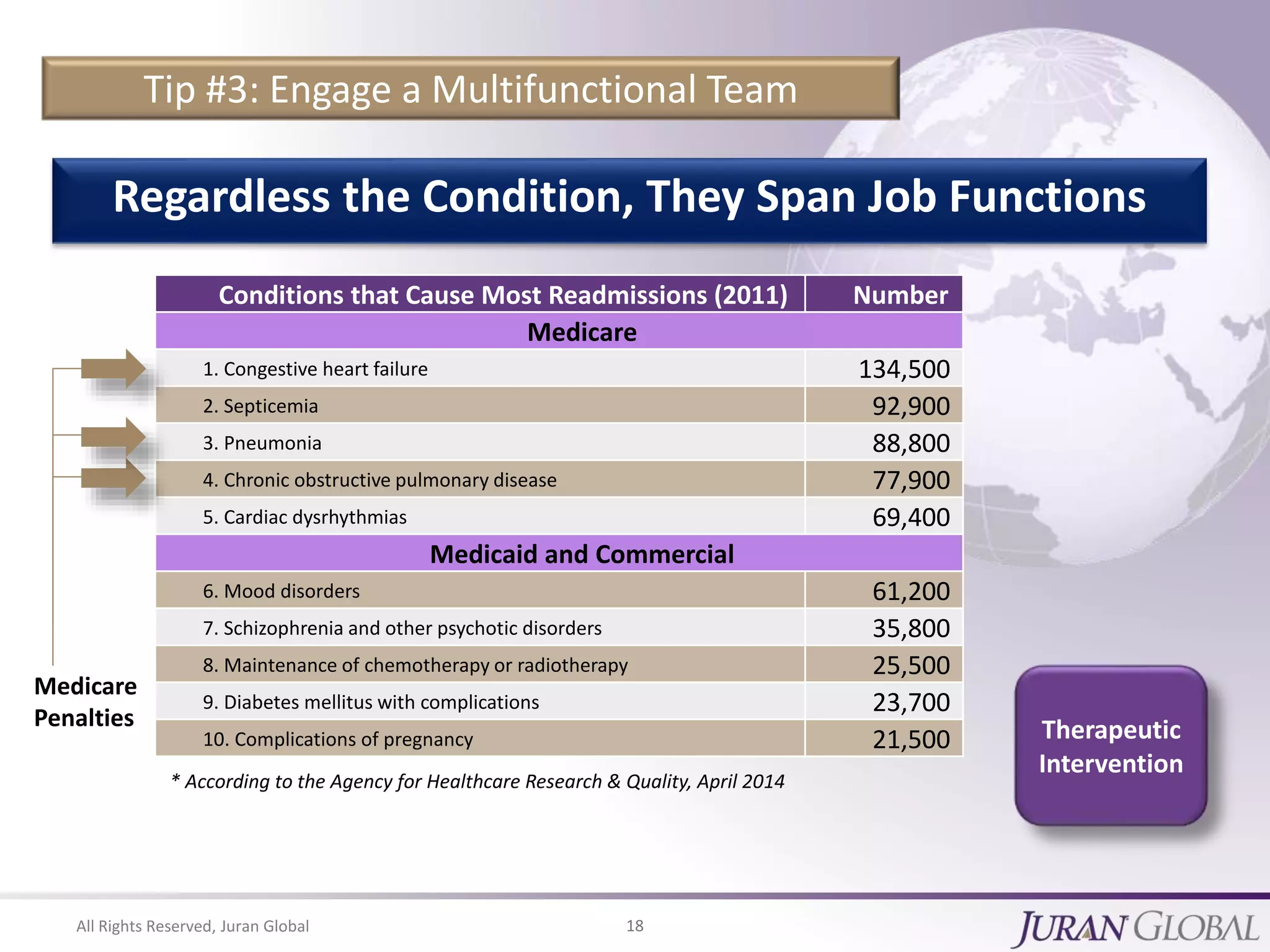
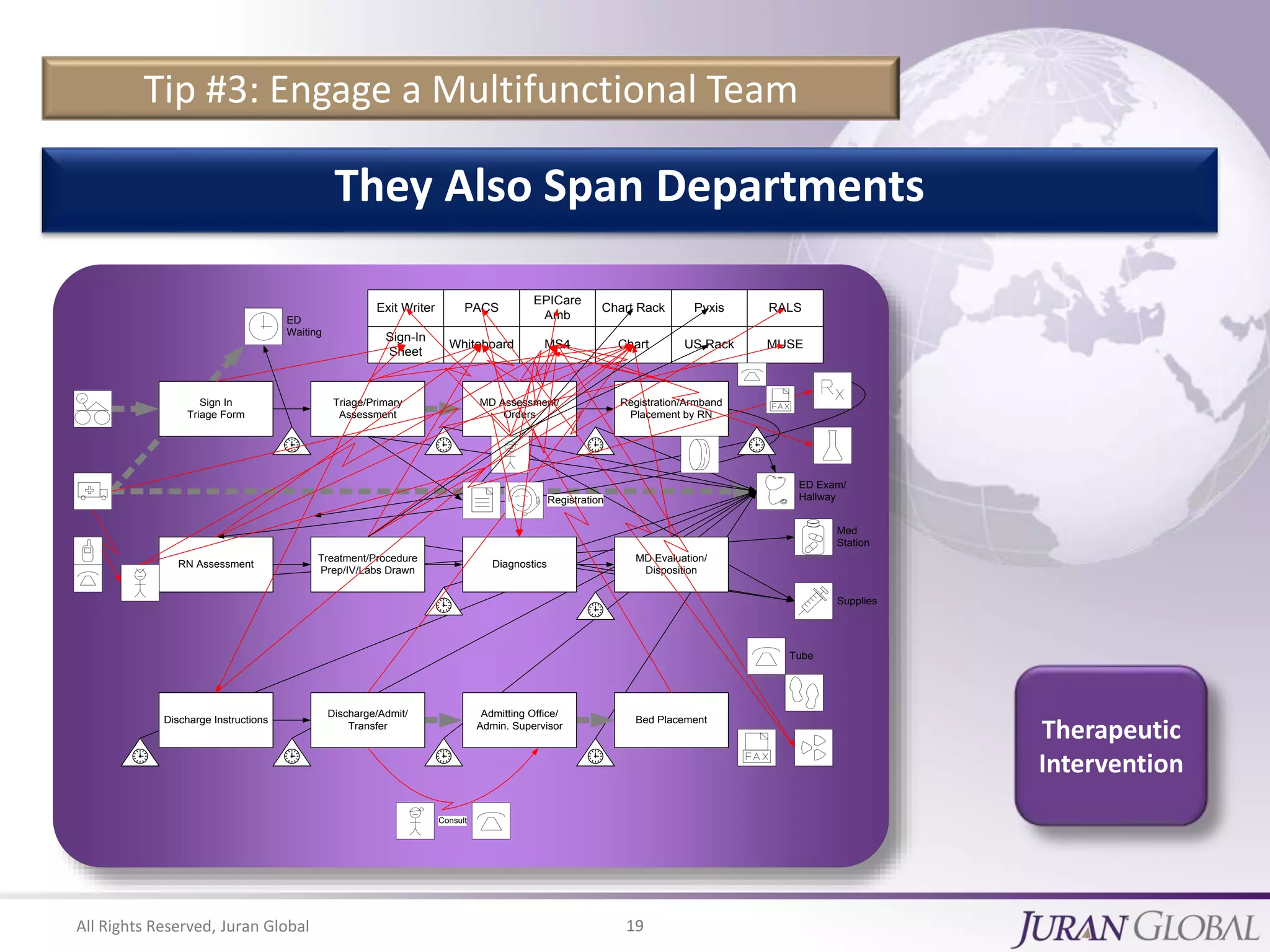
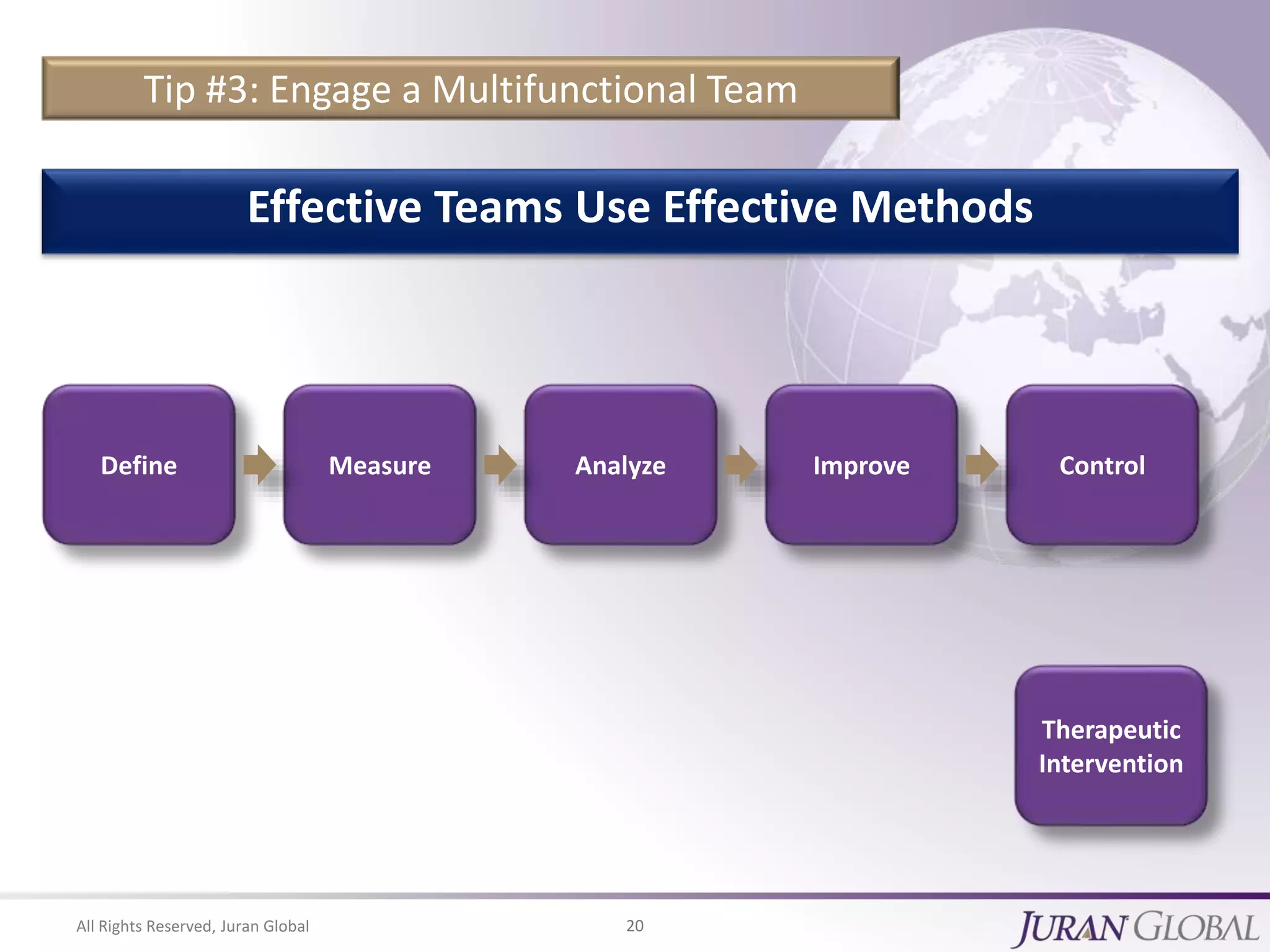
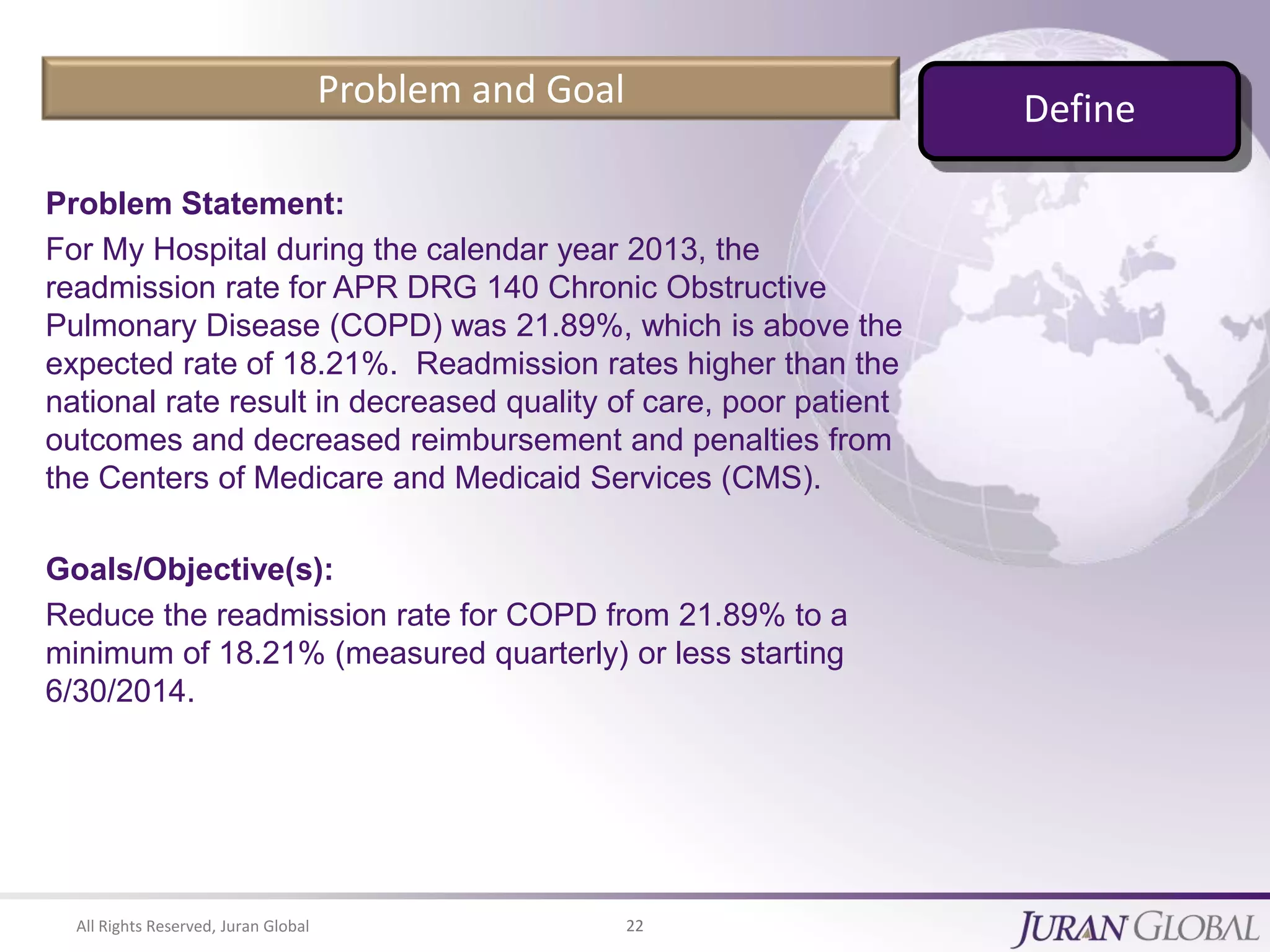
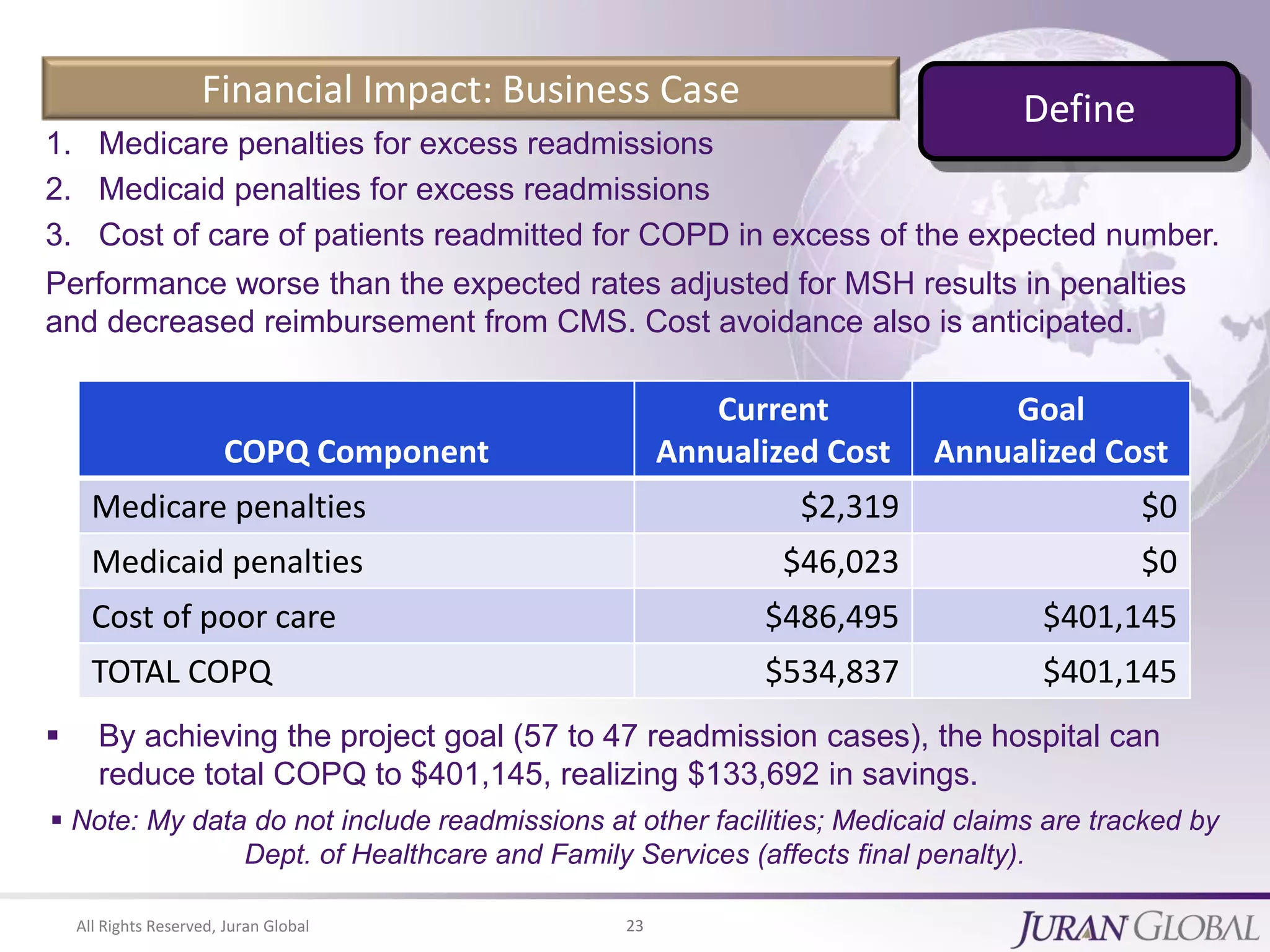
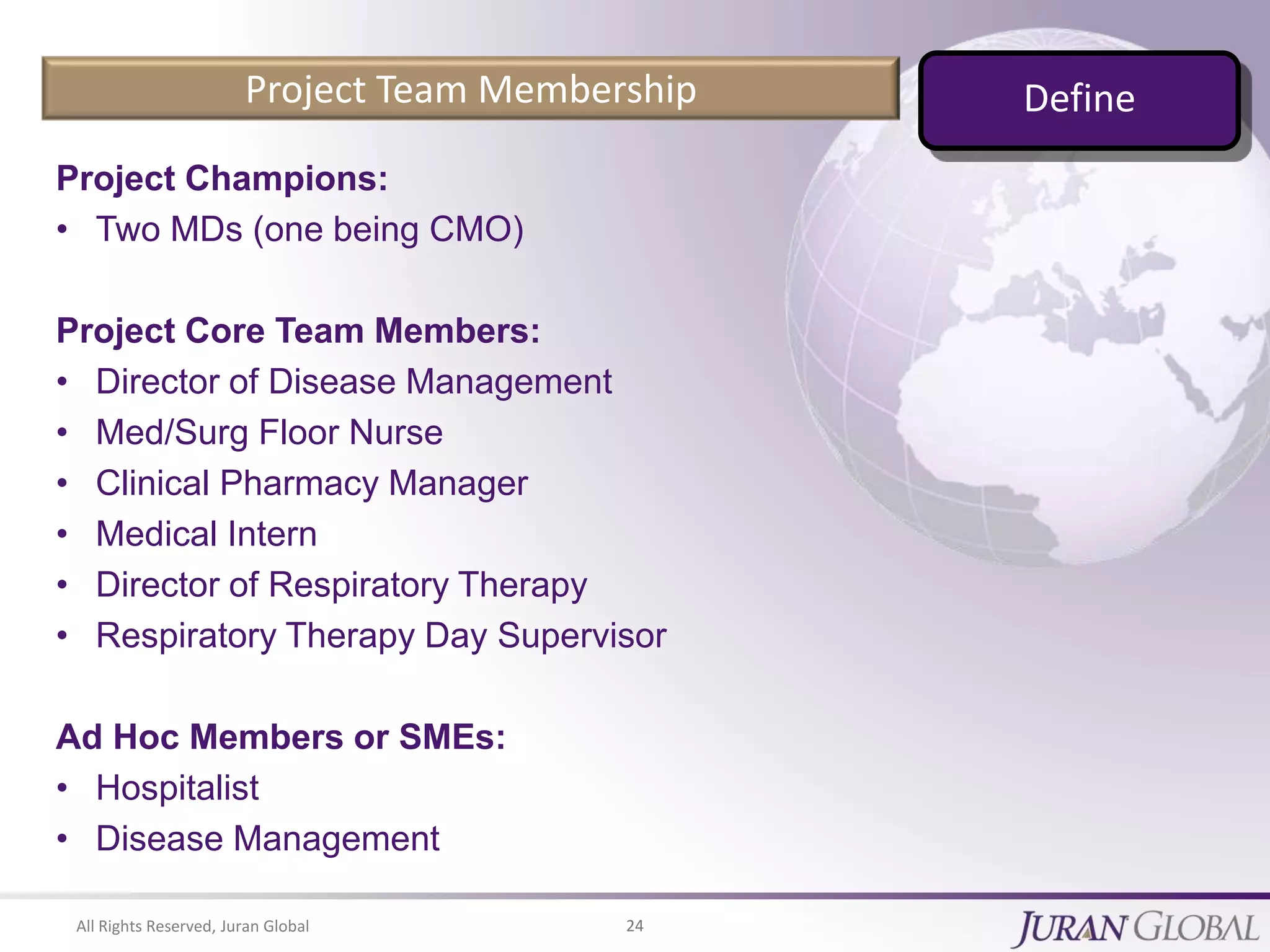
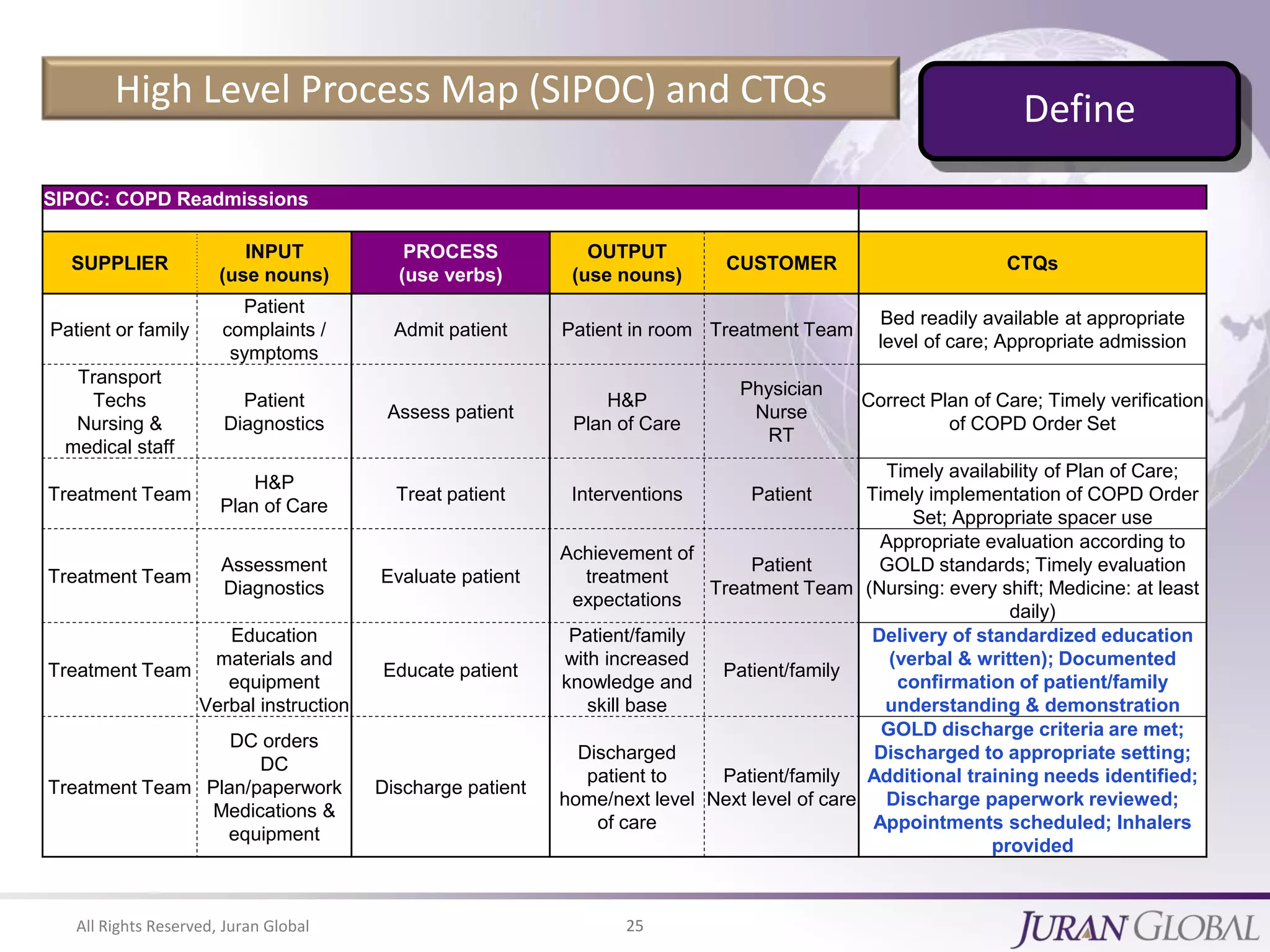
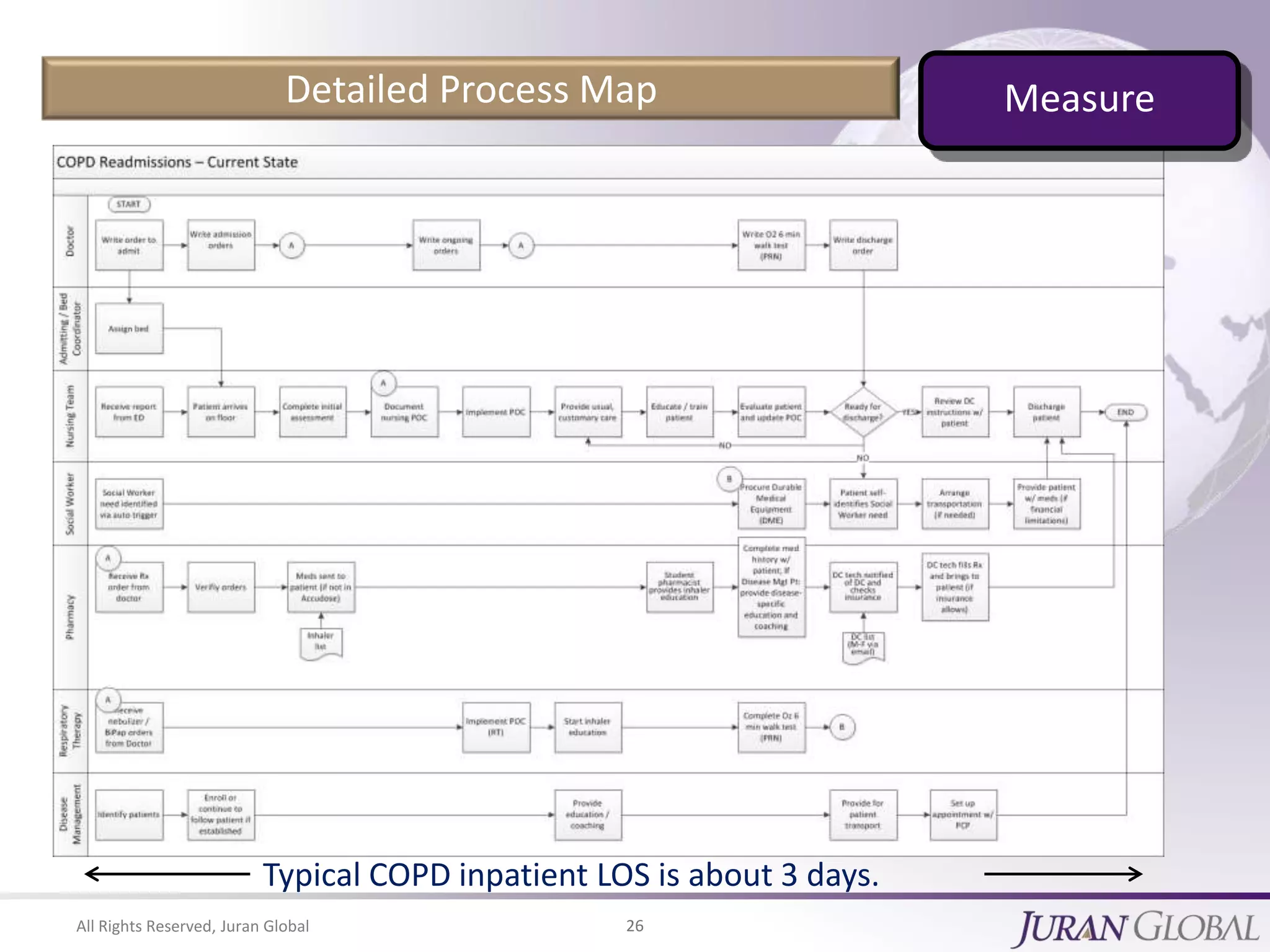
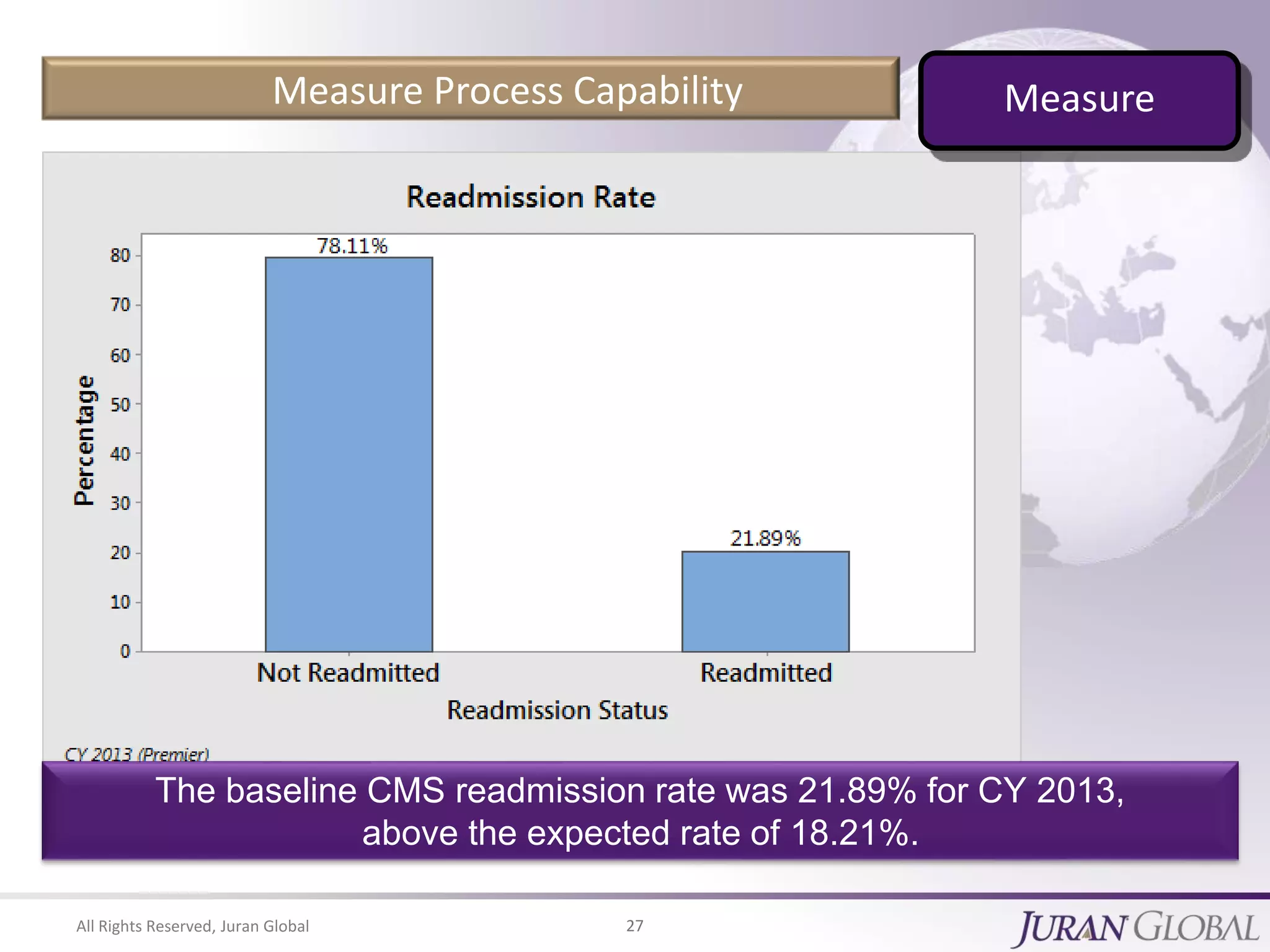
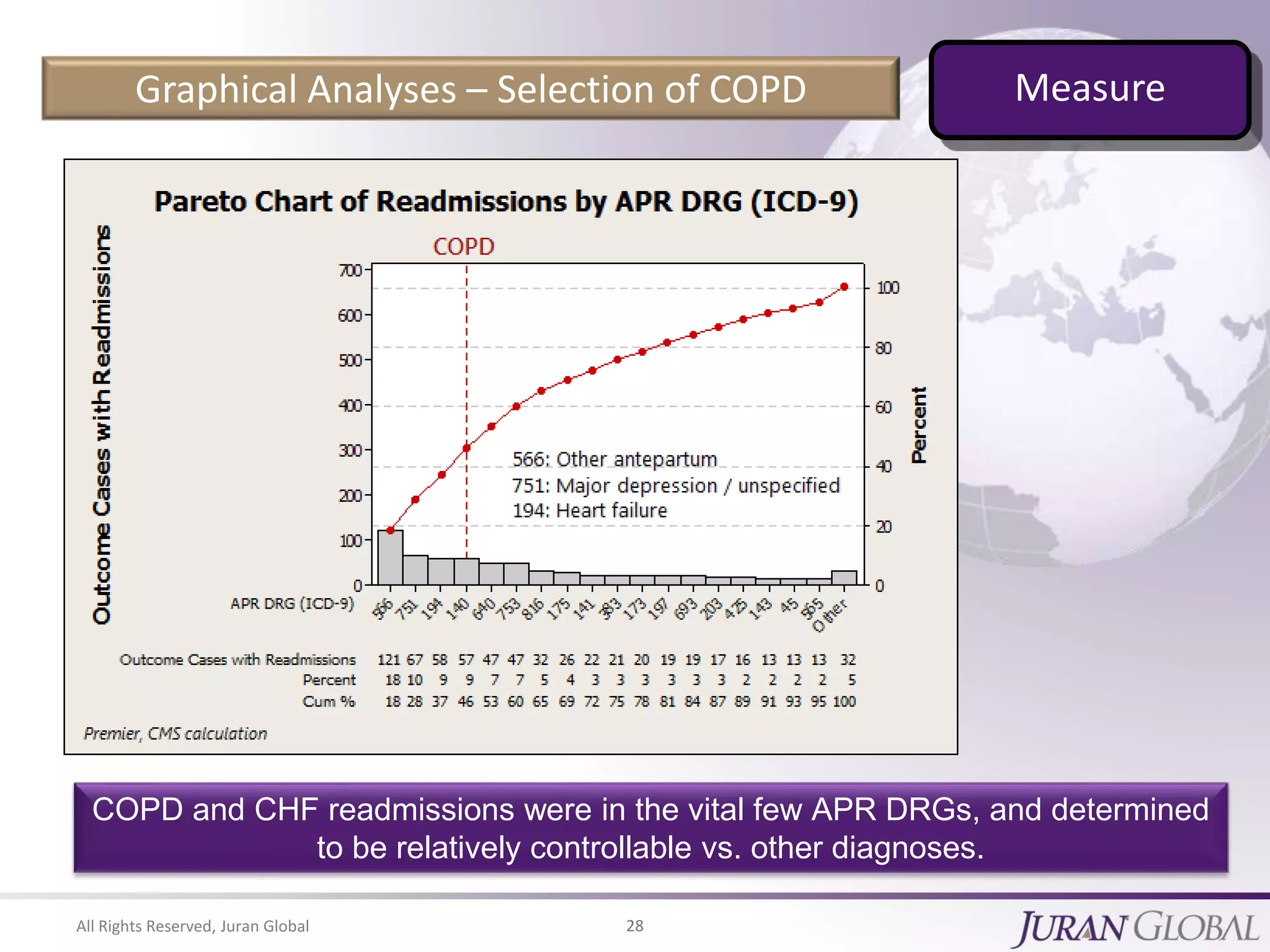
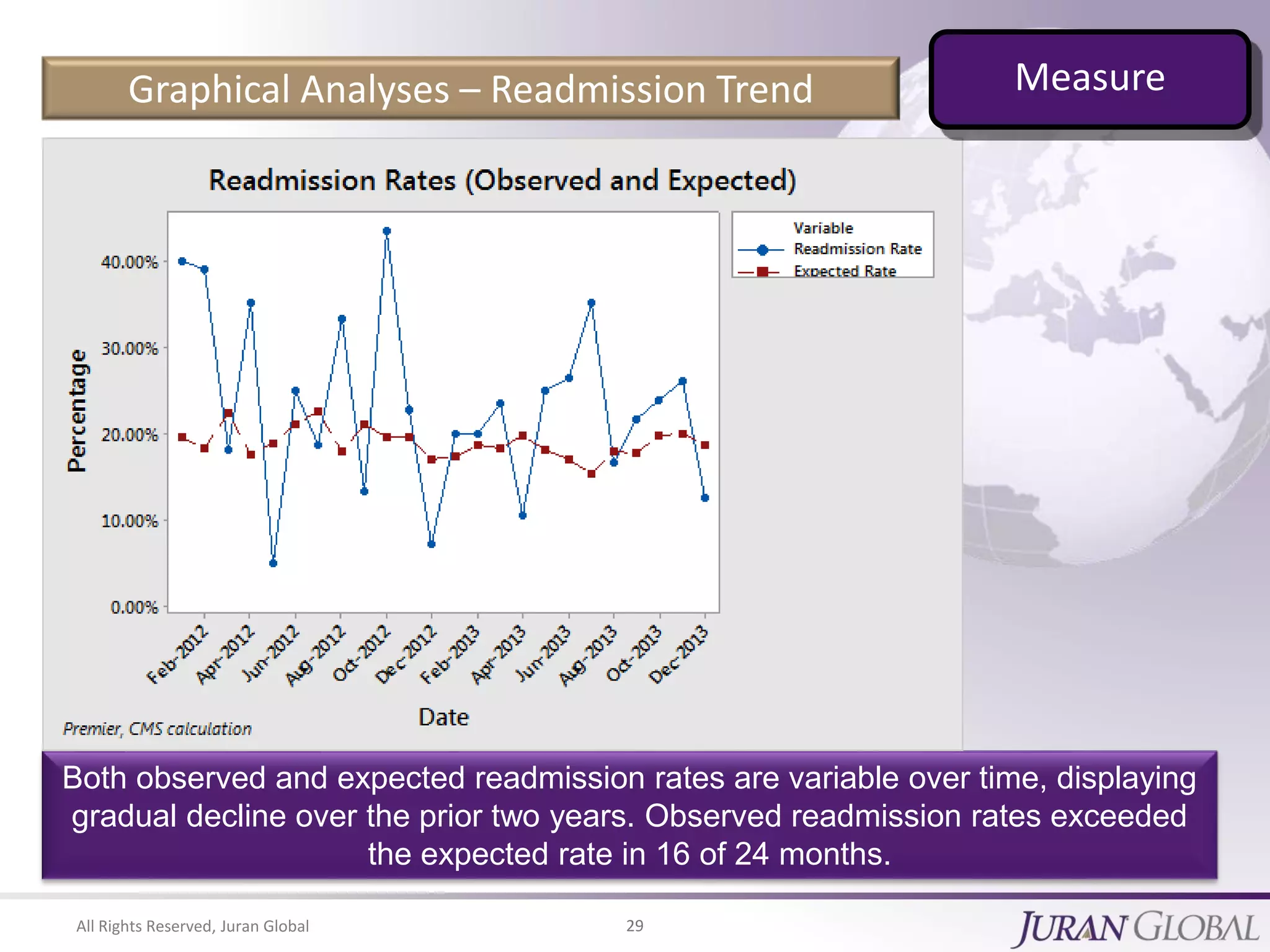
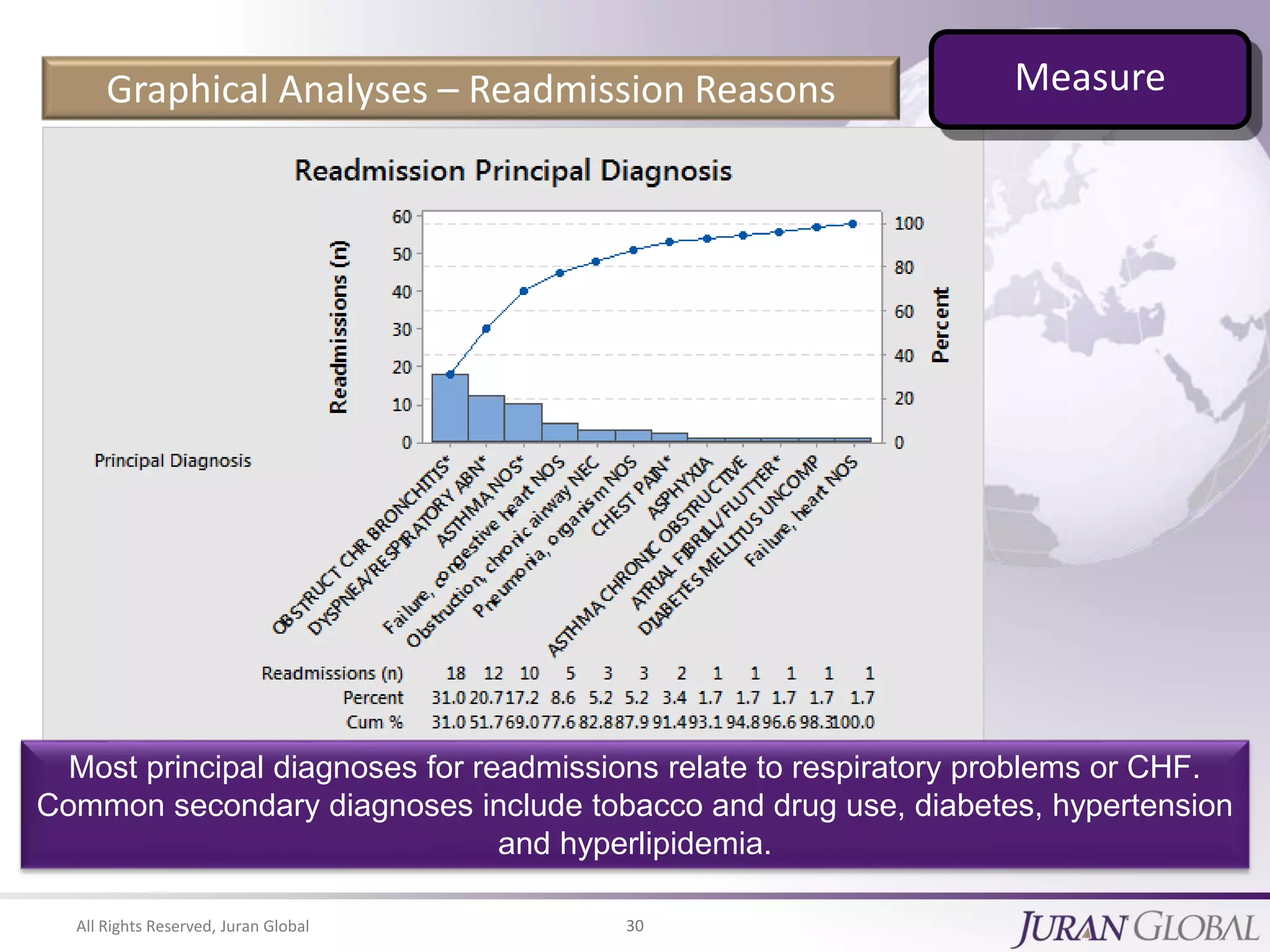
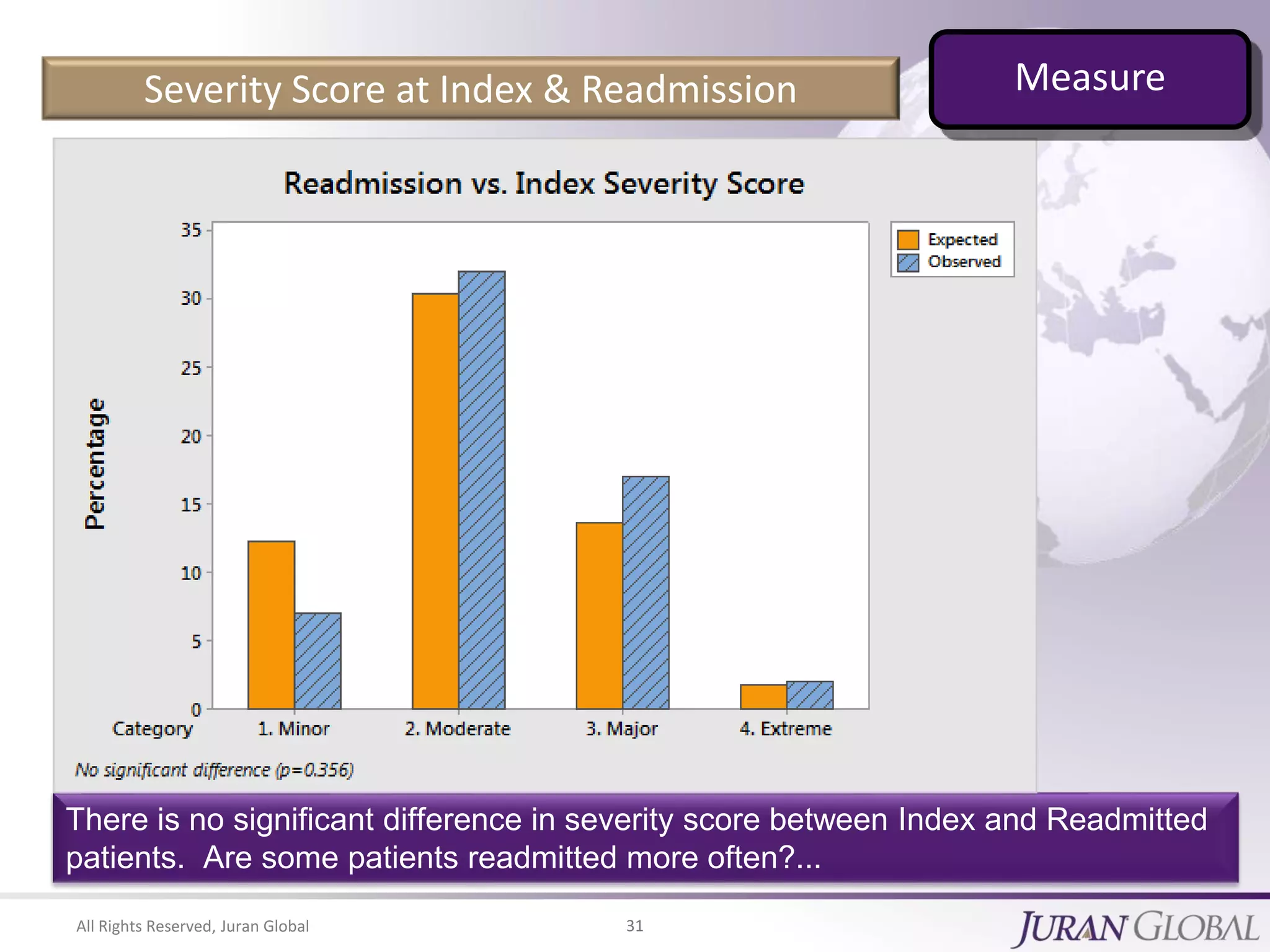
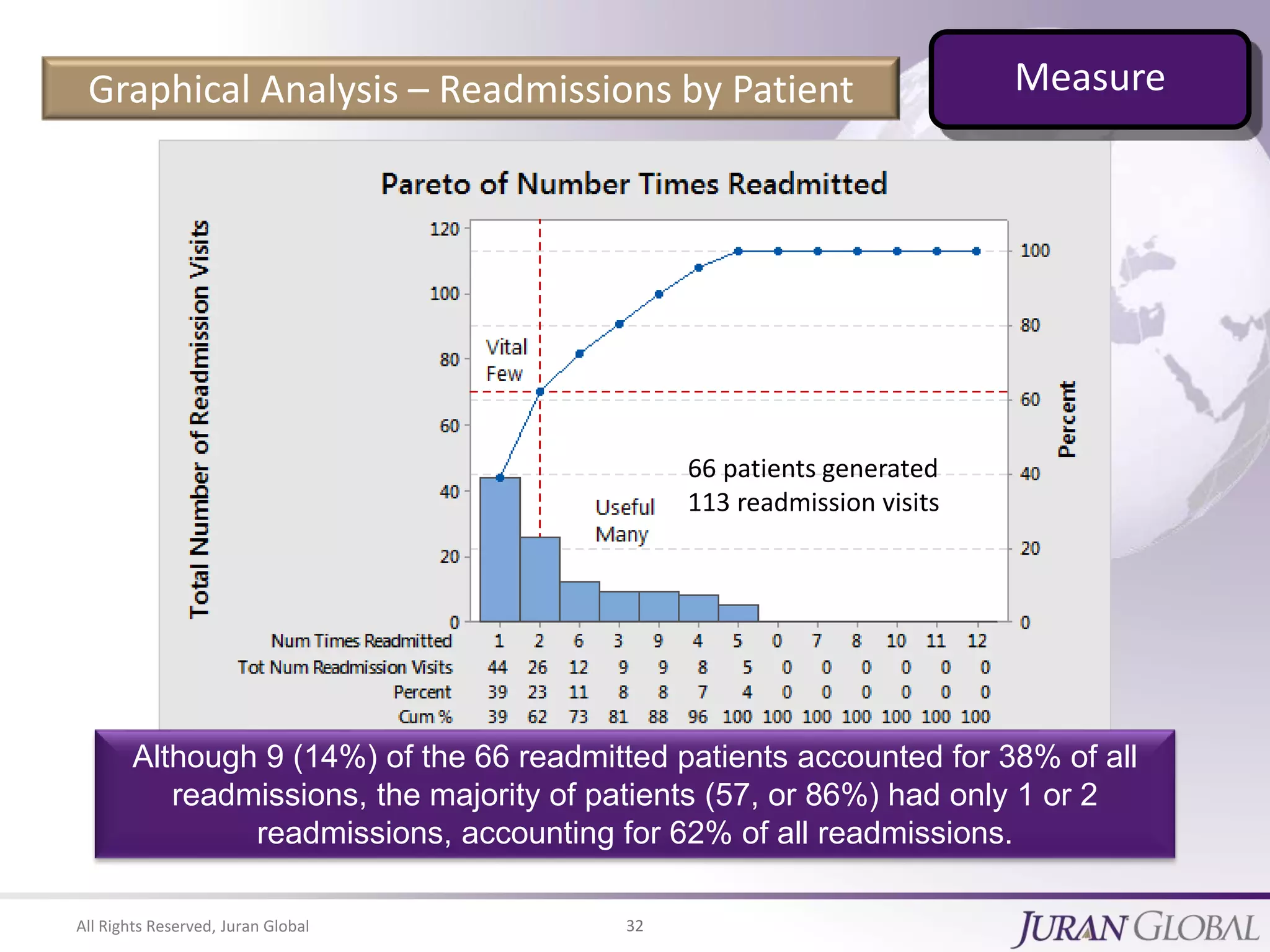
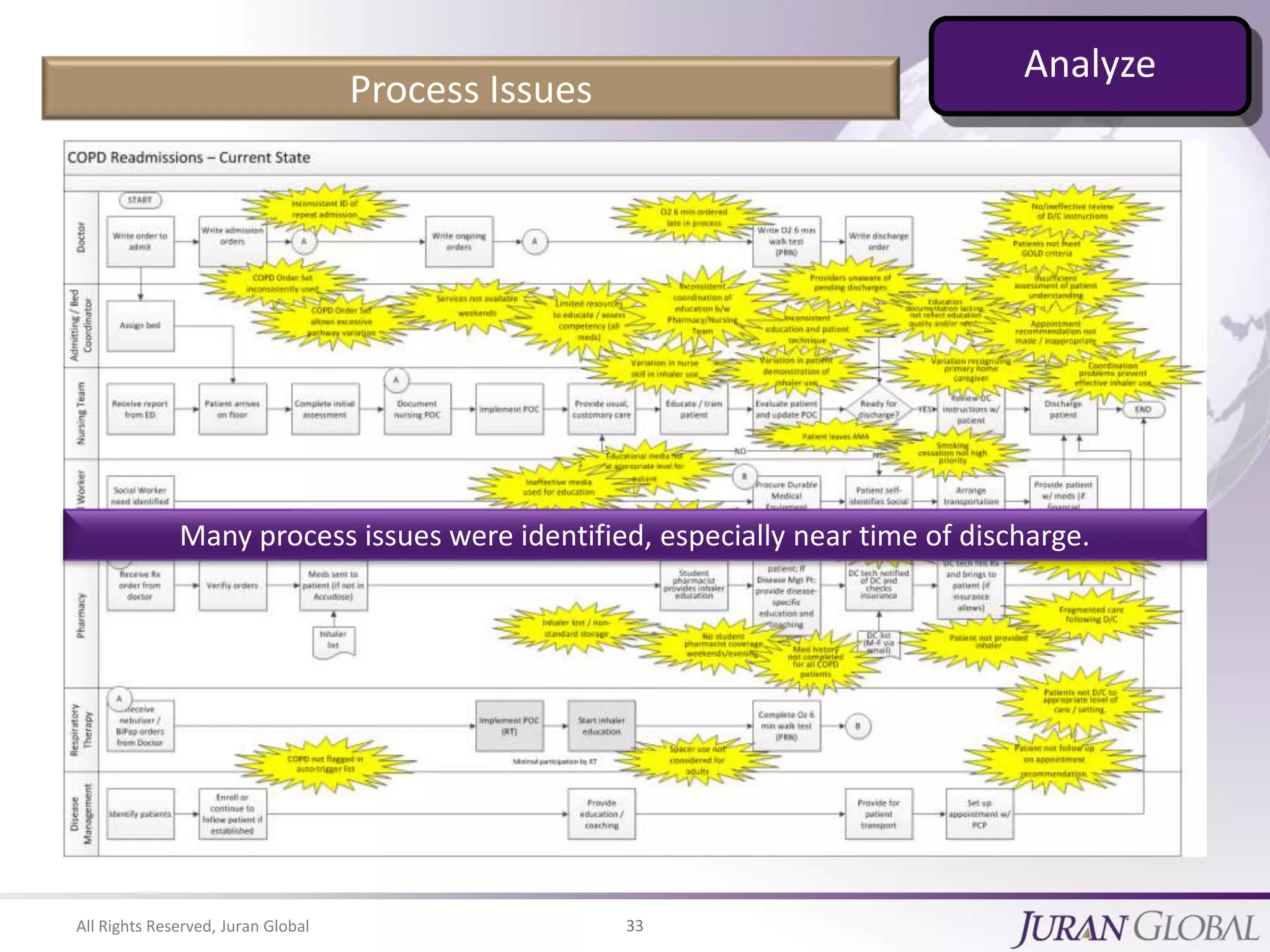
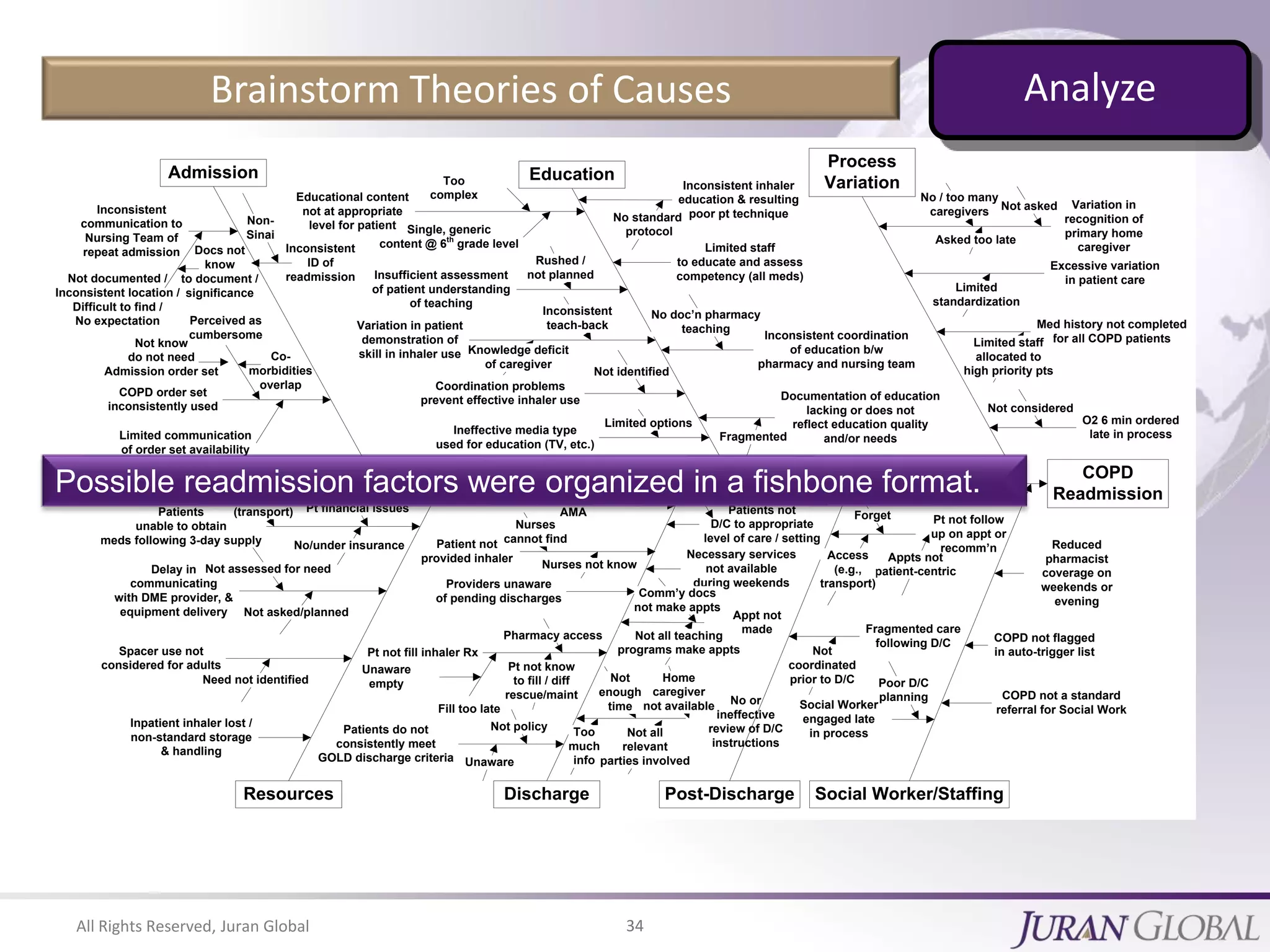
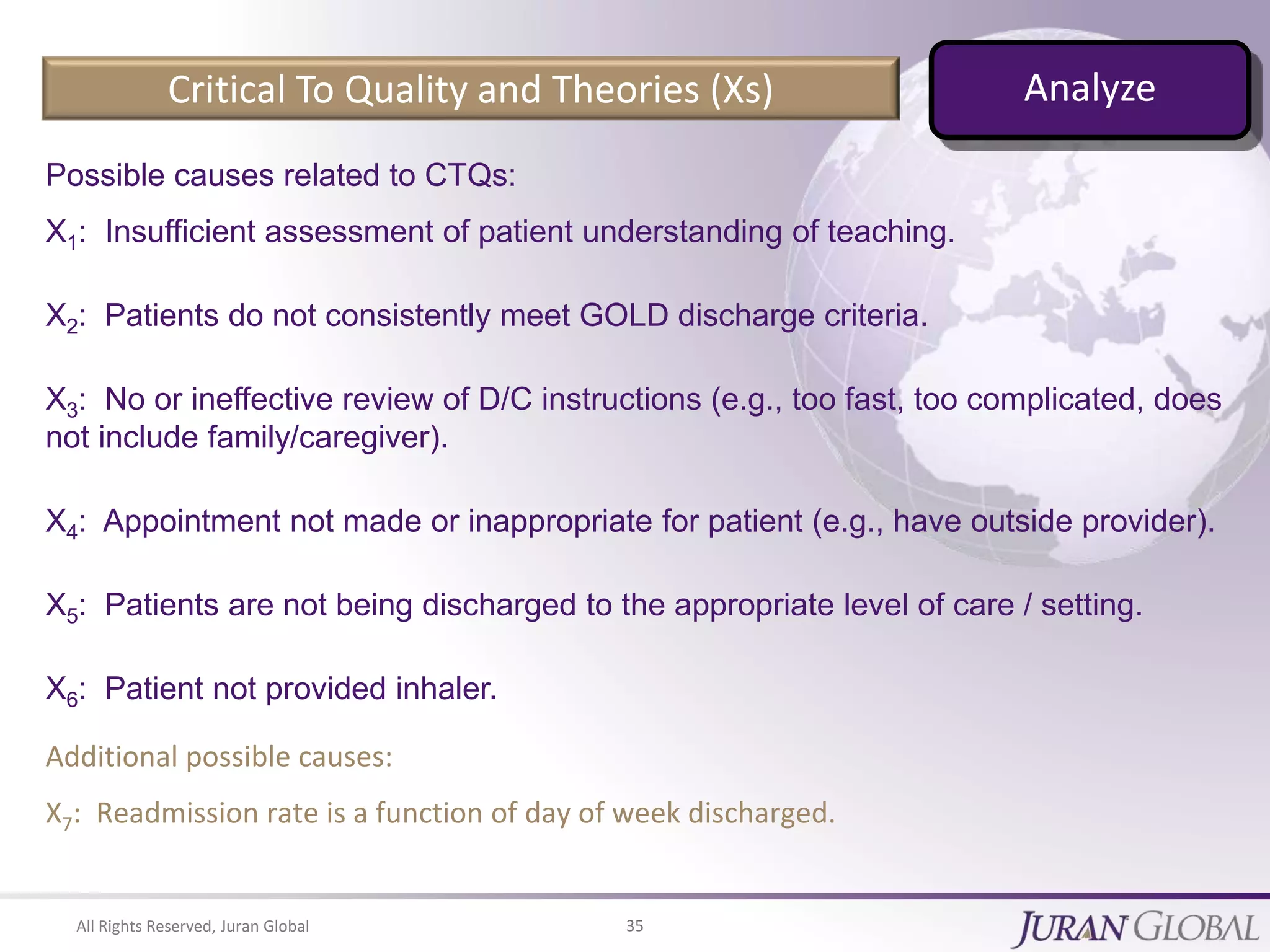
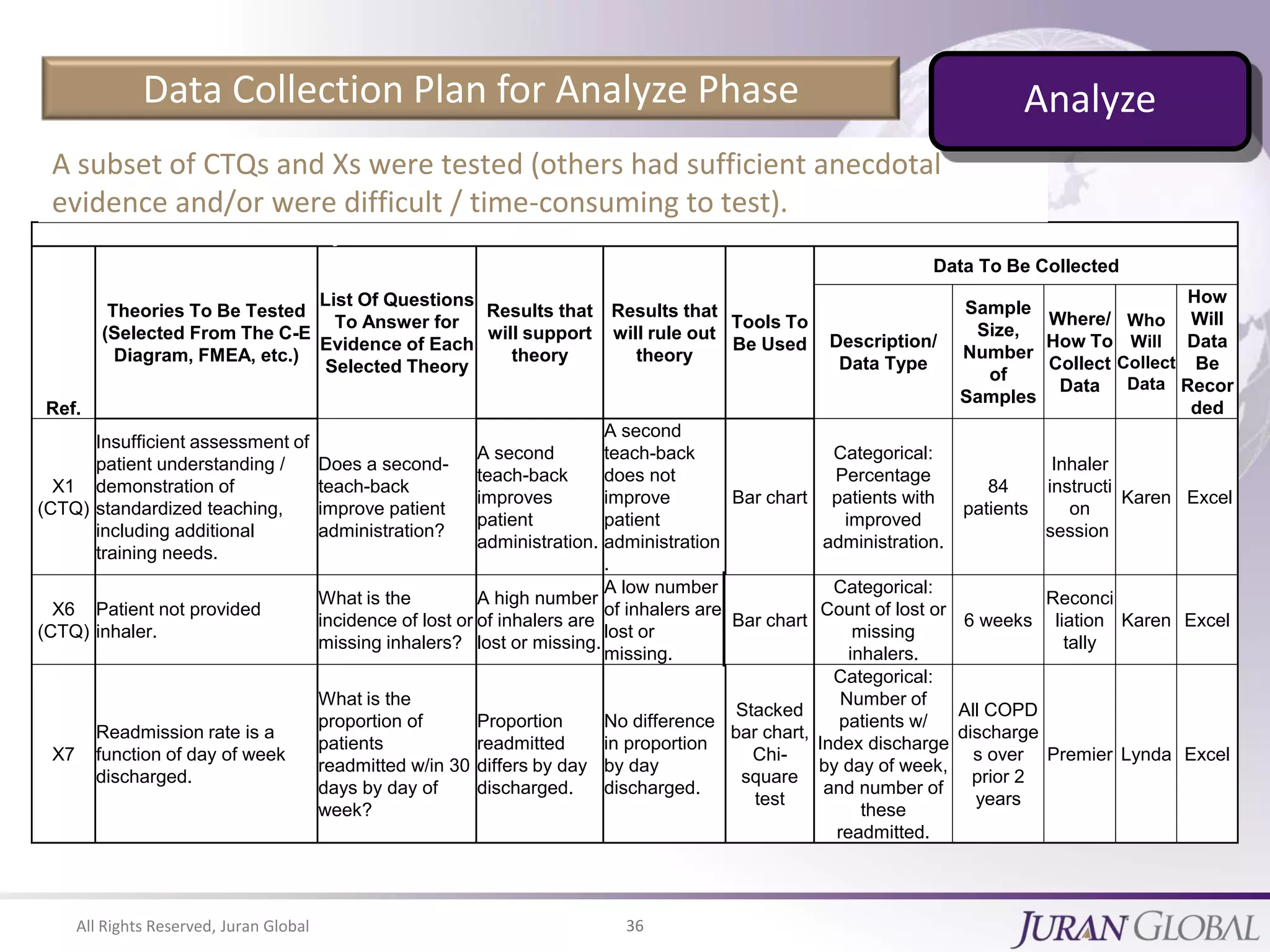
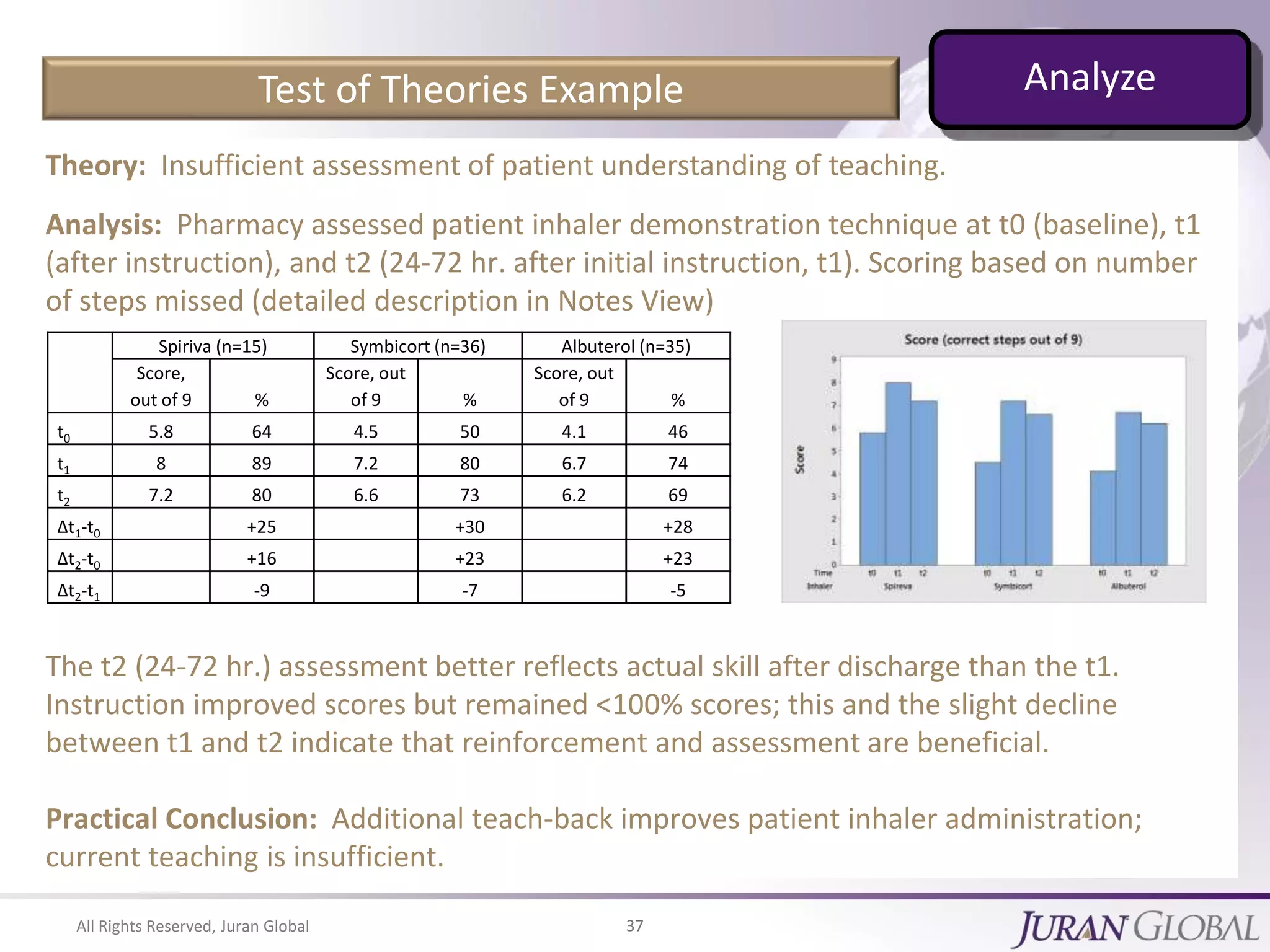
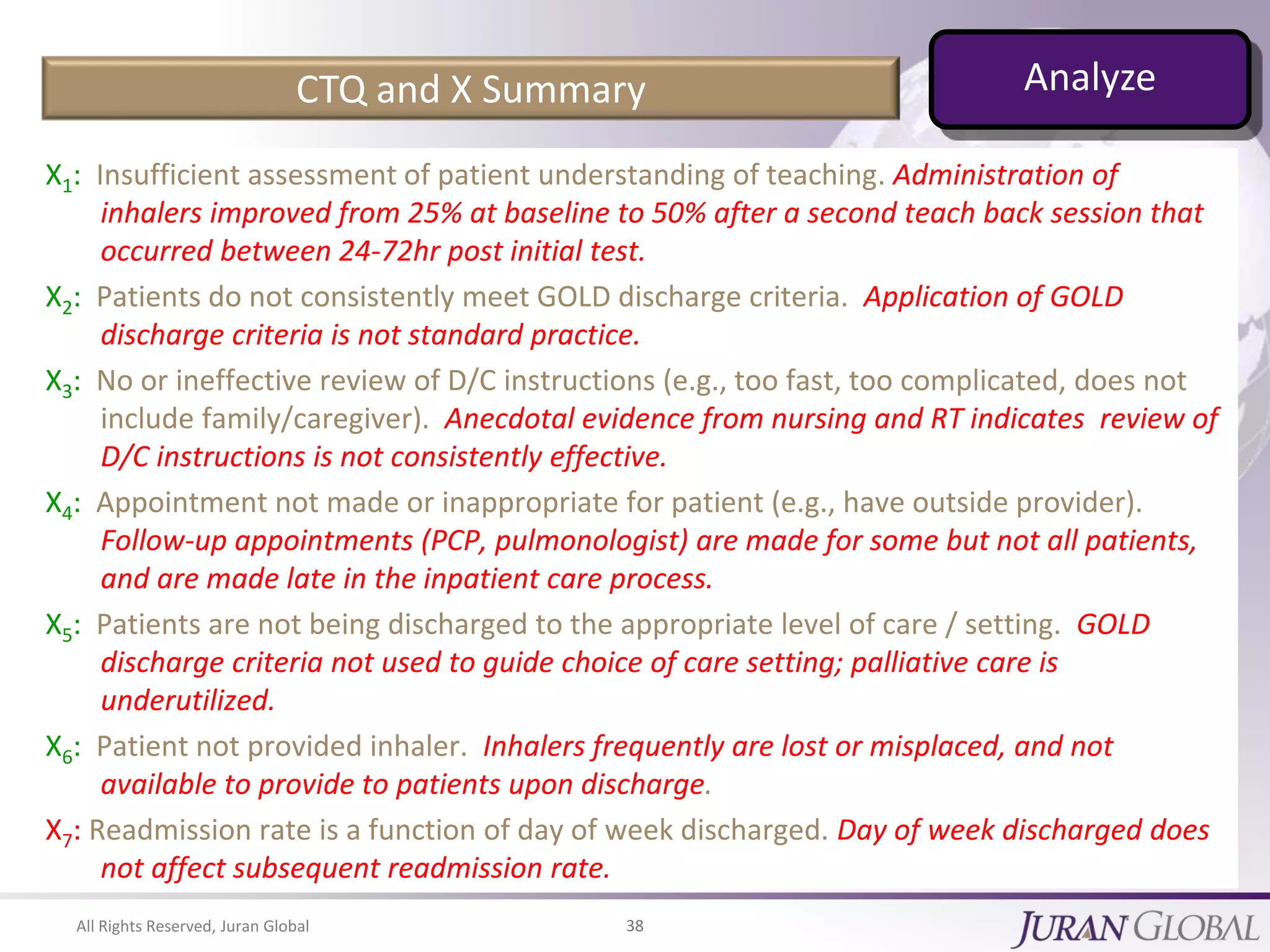
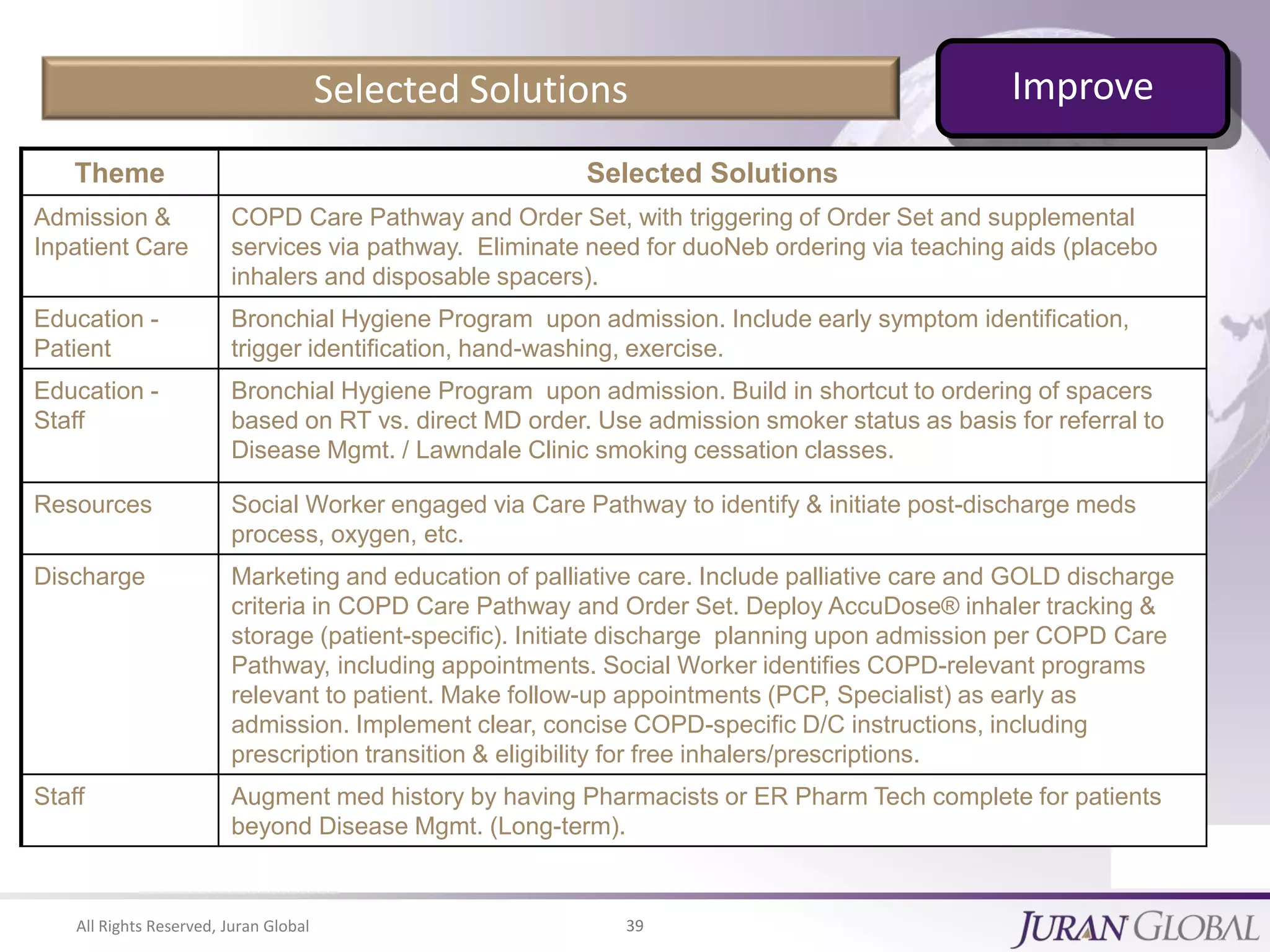
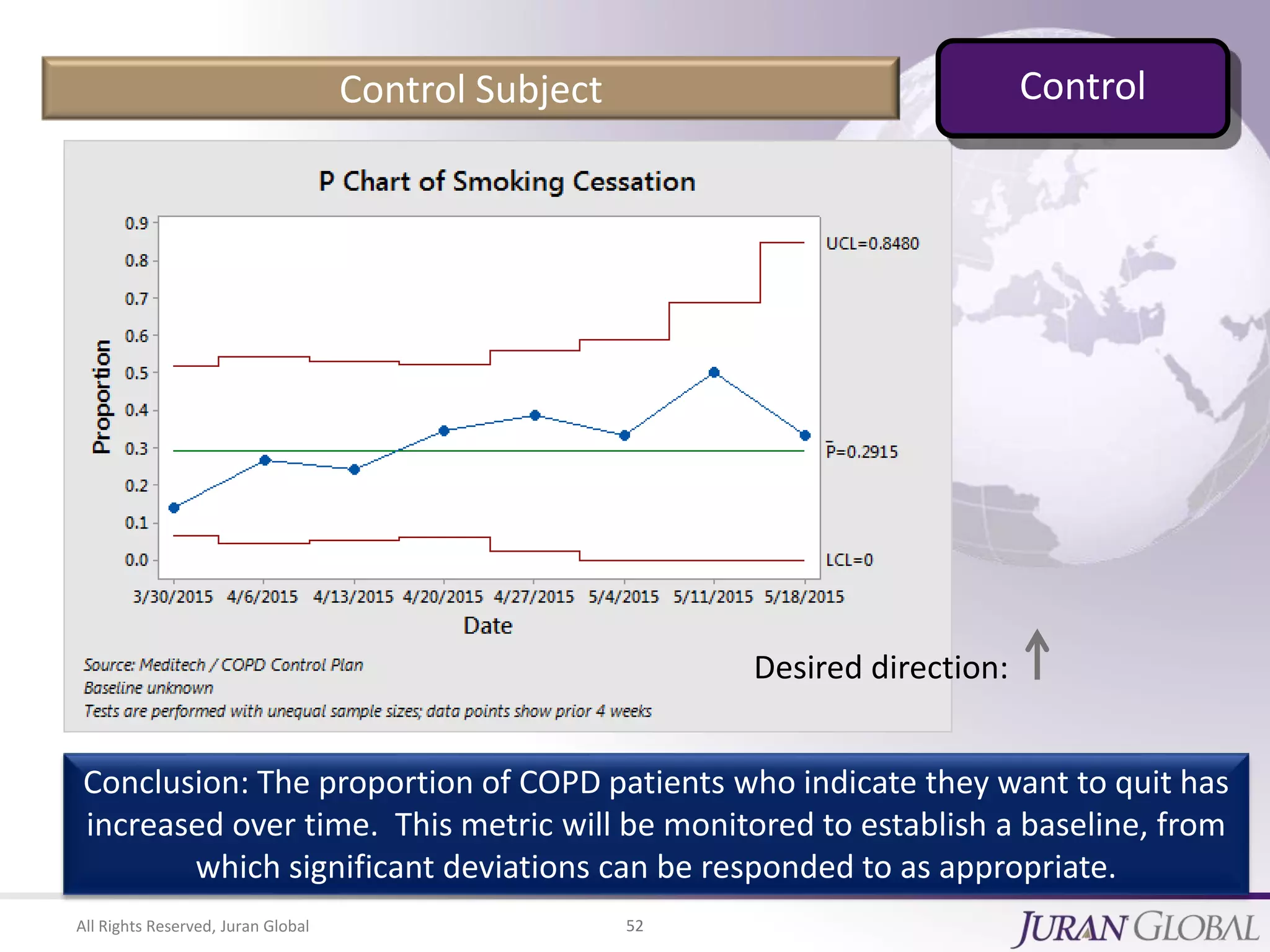
This document provides tips for reducing hospital readmissions. It discusses the importance of accurately analyzing the root causes of readmission problems using valid data and proven methods like Six Sigma. The first tip is that there are no "magic bullets" and organizations need to properly diagnose issues before implementing solutions. Additional tips include engaging a multi-functional team to address readmissions and ensuring leadership support. Data analysis methods like process mapping and cause-and-effect diagrams are recommended to identify factors contributing to excess readmissions. Overall the document emphasizes the need for rigorous problem analysis over quick fixes in order to successfully reduce readmission rates.