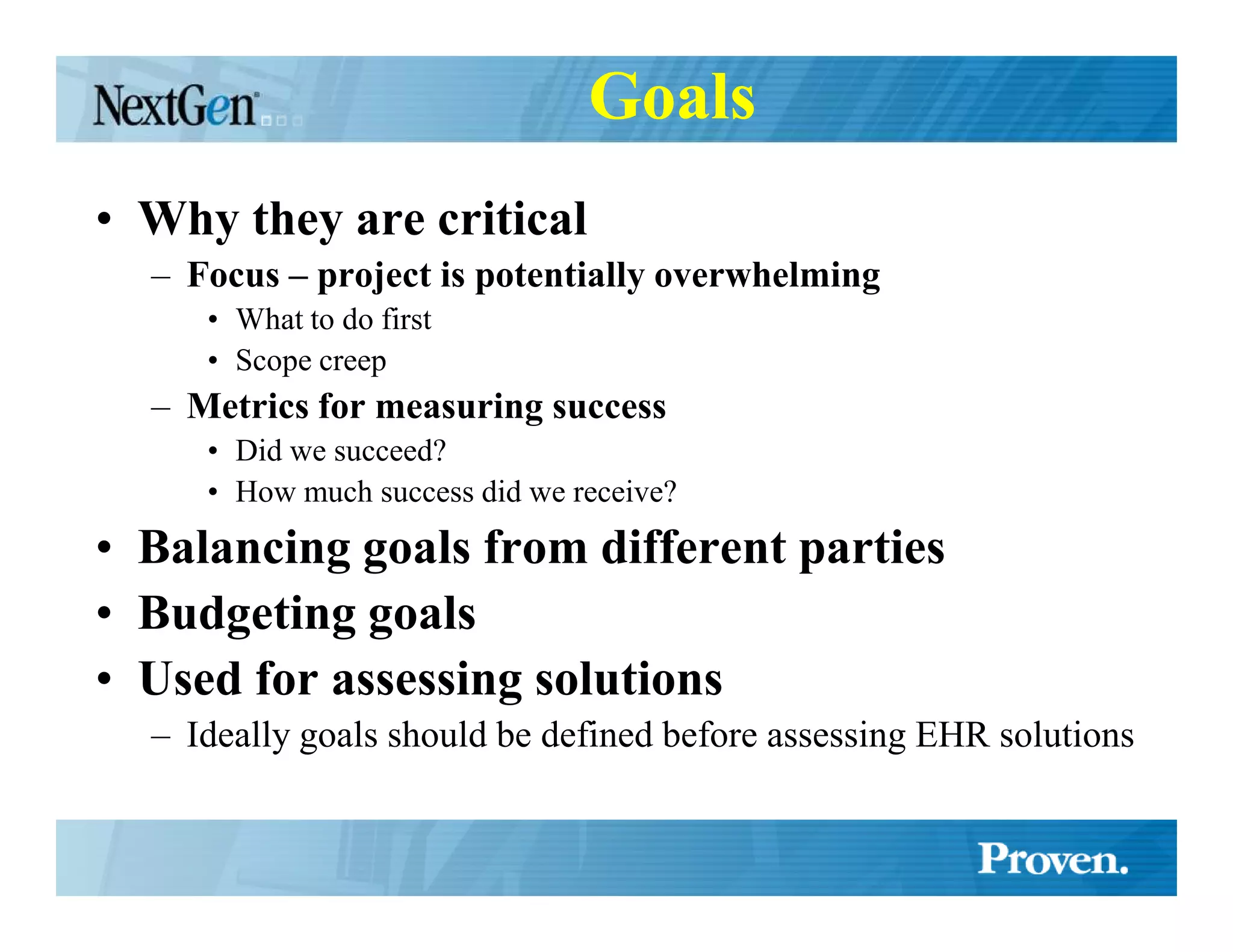
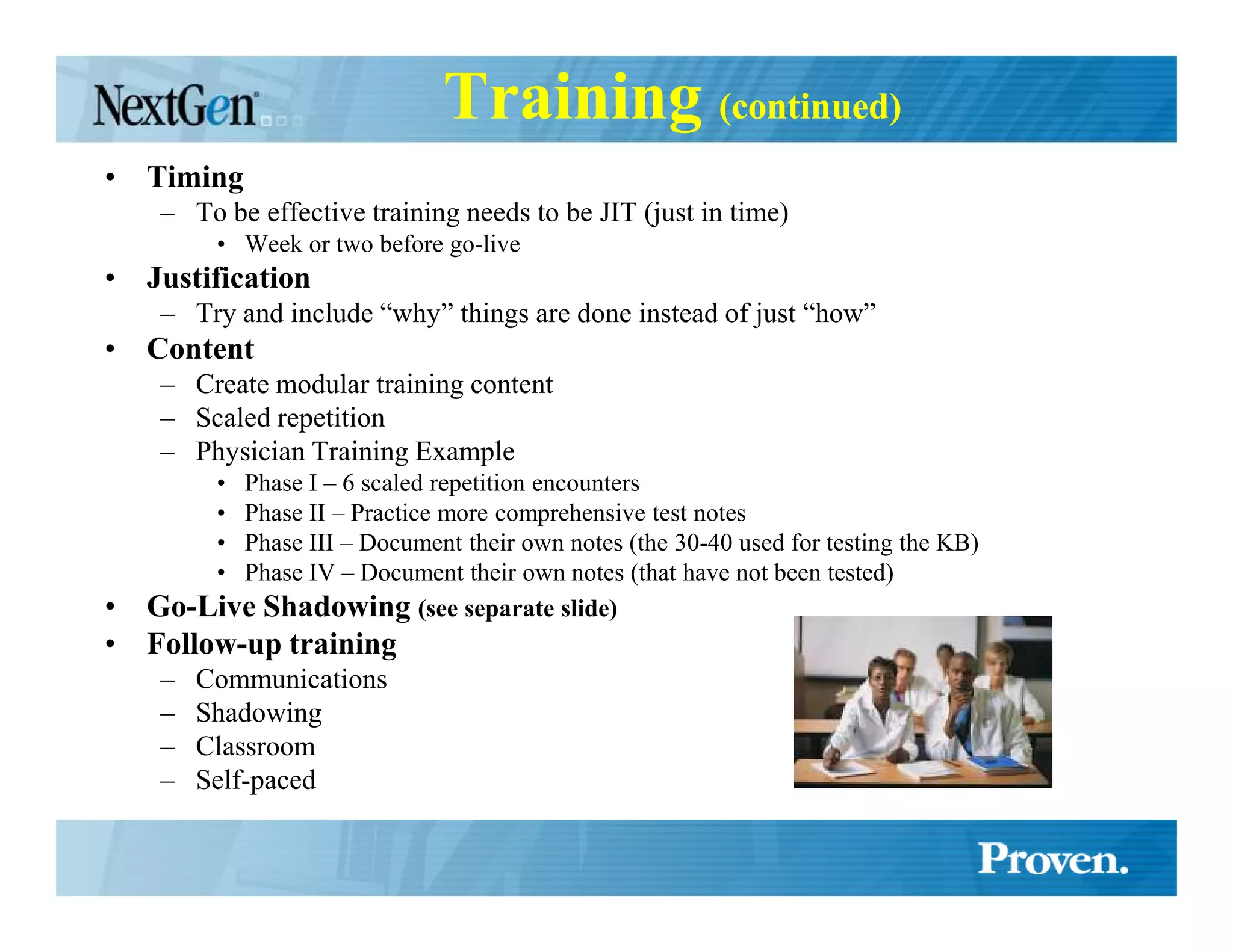
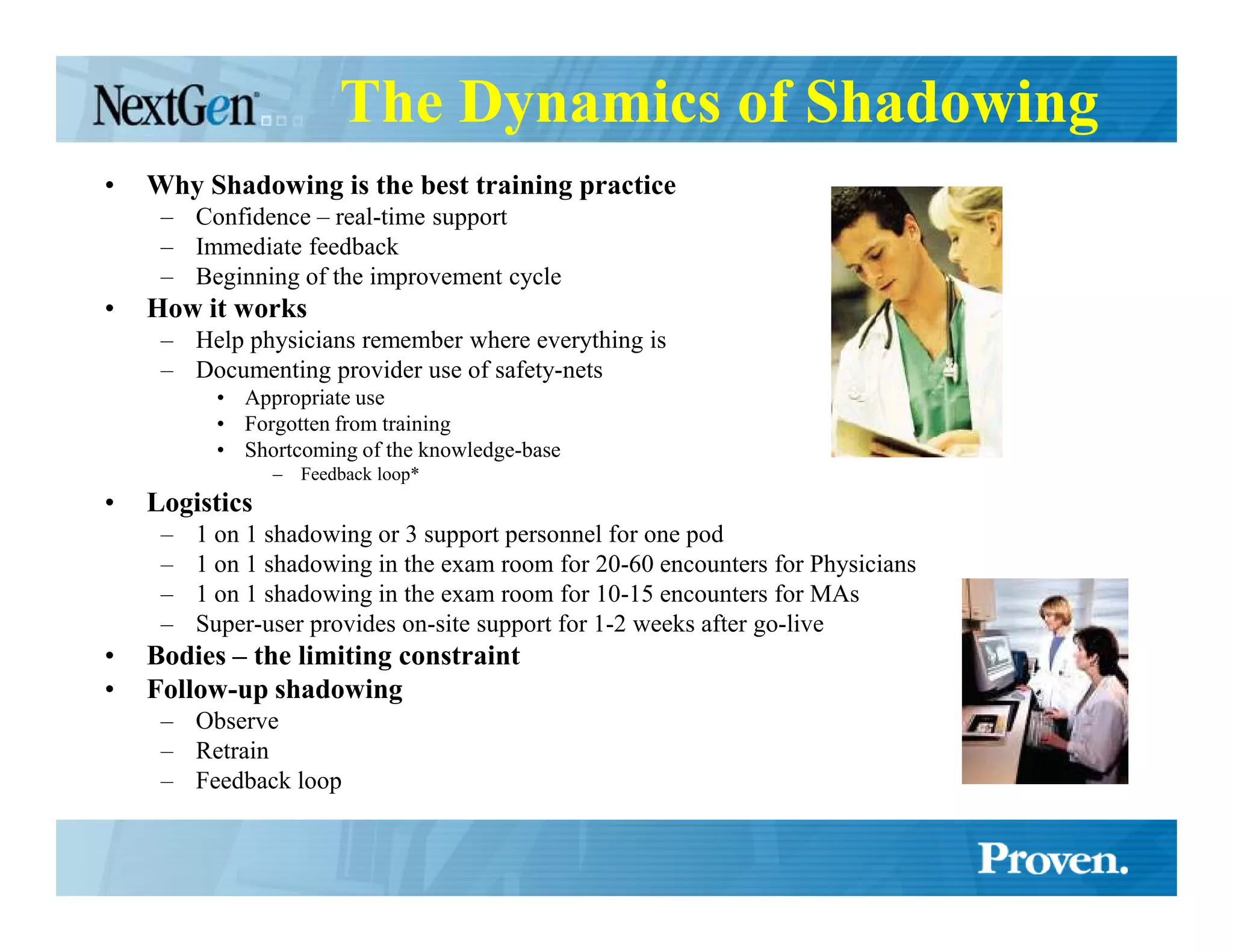
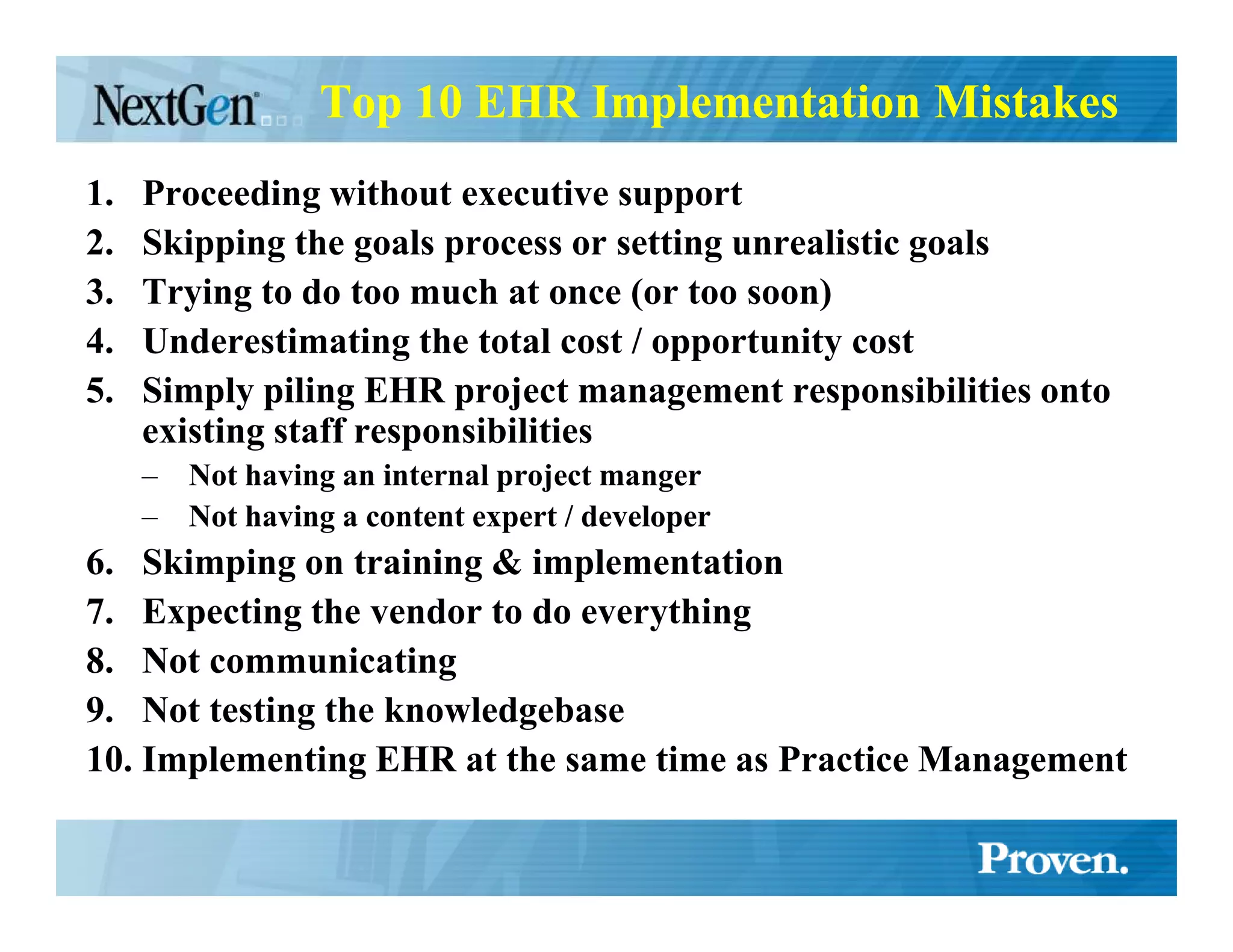
Implementing an EHR is a complex project that requires extensive planning and involvement from all stakeholders. Key steps include defining goals and metrics, analyzing workflows, selecting an appropriate vendor, and providing comprehensive training for end users. A successful implementation follows best practices such as establishing executive support, implementing in increments, thoroughly testing the system, and providing ongoing support and feedback after going live. Shadowing providers during training and post go-live periods is critical to ensure adoption and maximize benefits of the new EHR system.





![Tips
• Use Incremental training process
• Shadow providers, observer, create feedback loop
• Test the vendors knowledge base by entering 30-40 actual charts (for each provider) before you present it to the
doctor.
• Define preference lists for providers before go-live
– Medications
– SIGs
– ICD9s
– Chief Complaints
– Etc.
• Let patients know you are transitioning to computerized patient records
– Letters
– Posters
– Brochures
– News Media
– Face to face
• Publish your practical EHR tips in a document or on your internal web site and send them out every two weeks or so
• Attend your vendors user group meetings
• Complete all training and self-paced learning
• Keep go-live groups modular [reword]
• Don’t schedule go-live during peak season
• Get computer training before training for those not as computer literate [reword]
• Have as many super-users as possible
• Celebrate small victories
• Create three EMR environments – Demo, Test & Production
• Be 100% committed
• Provide your project manager all the resources they need to succeed
• Don’t under-resource your technology
• The IT staff cannot do everything. IT is just one of the skill sets required for successful implementation](https://image.slidesharecdn.com/successfulehrimplementationstrategytips-12825261011644-phpapp02/75/Successful-EHR-Implementation-Strategy-amp-Tips-37-2048.jpg)