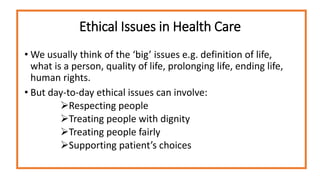
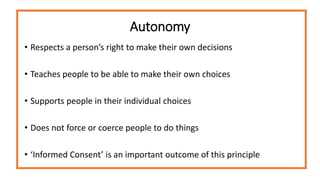
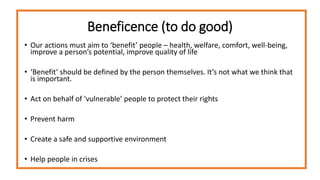
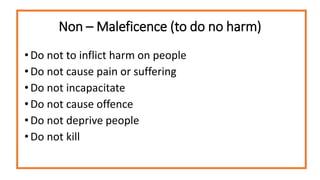
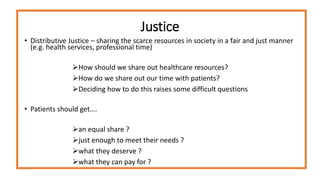
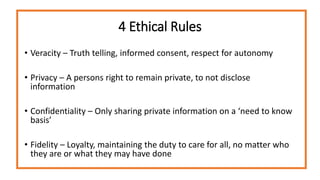
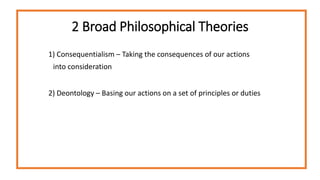
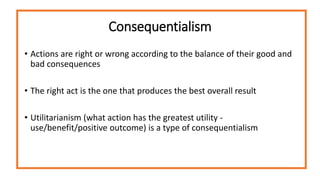
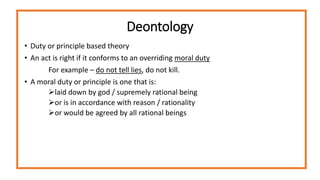
This document introduces some key concepts in medical ethics, including the four main ethical principles of autonomy, beneficence, non-maleficence, and justice. It discusses ethical issues that clinicians may face in healthcare, from big issues like determining what constitutes life to smaller interpersonal issues like treating patients with dignity and respecting their choices. The document also outlines two main philosophical approaches to ethics - consequentialism, which considers the consequences of actions, and deontology, which focuses on adhering to principles of duty. It provides examples of how these principles and theories can guide decision-making around ethical dilemmas in clinical practice.