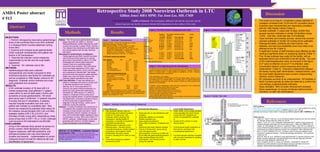
This summarizes a retrospective study of a 2008 norovirus outbreak at a long-term care facility in North Carolina. The outbreak lasted 16 days and infected 71 patients (57% attack rate) and 24 staff (20% attack rate). Risk factors for infection included being female, having diabetes, and low levels of independence. The facility implemented enhanced hygiene measures, staff self-quarantine, and restricted admissions and visitors, which may have contained the outbreak. The total estimated cost to the facility was $34,000.