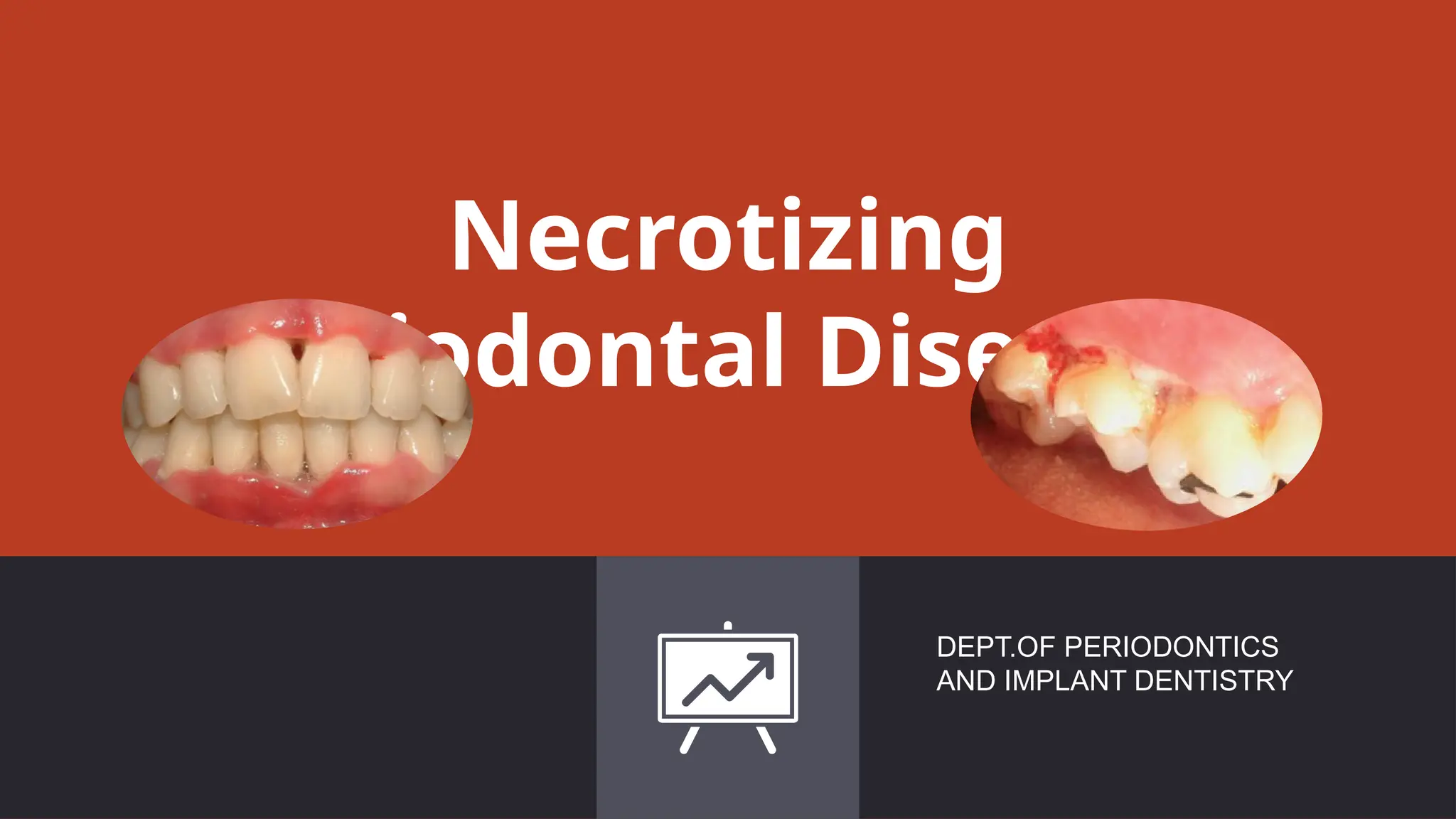
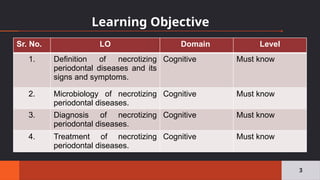
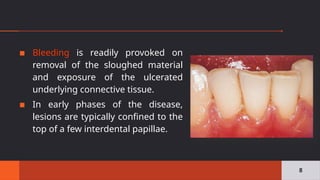
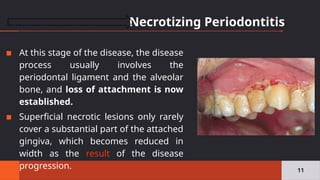
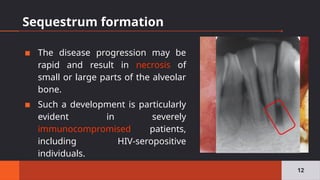
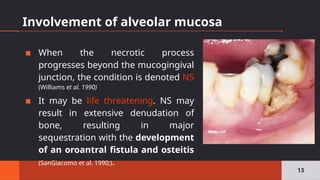
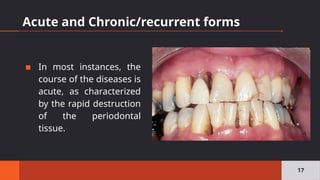
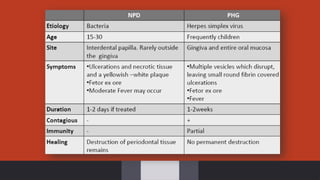
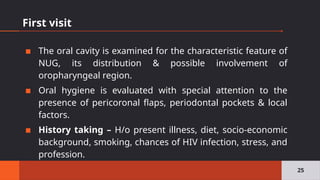
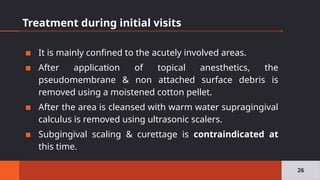
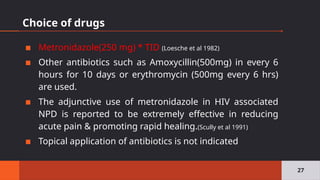
Necrotizing periodontal diseases encompass necrotizing gingivitis, periodontitis, and stomatitis, characterized by necrosis of gum tissue, bleeding, and pain, leading to rapid tissue destruction. Effective treatment is urgent and includes superficial debridement and improved oral hygiene, with surgical options considered for individual cases. The prevalence is low but the severity warrants immediate intervention to prevent further complications.