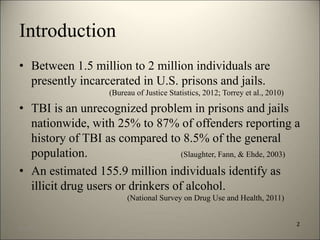
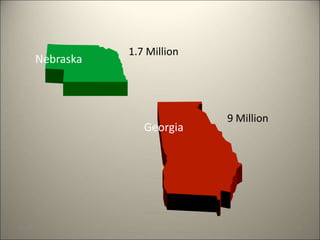
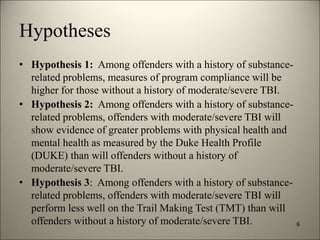
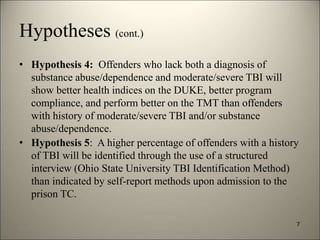
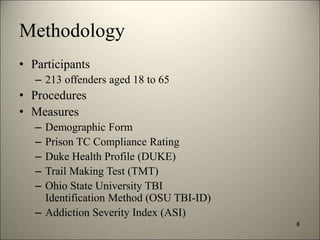
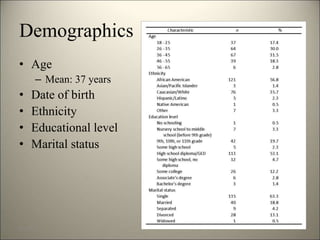
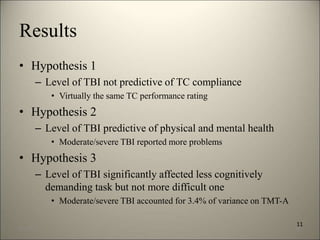
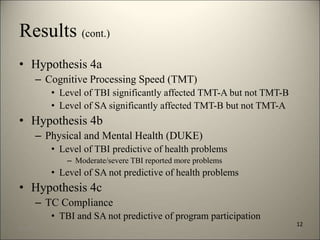
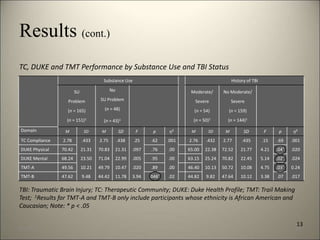
This document summarizes a study that examined the relationship between traumatic brain injury (TBI) and substance abuse among prison inmates in a therapeutic community (TC). The study hypothesized that inmates with a history of moderate or severe TBI would have poorer health, cognitive performance, and program compliance compared to inmates without TBI. It assessed 213 inmates and found that those with moderate/severe TBI reported worse physical and mental health, and performed slightly worse on a simple cognitive test, but showed similar program compliance. It also found higher rates of reported TBI using a structured interview compared to prison records. The study provides initial evidence on the interactions between TBI and substance abuse in prisoners.