The study explores medical students' attitudes towards mandatory HIV testing and disclosure, highlighting mixed opinions on the obligation to disclose HIV status for both healthcare professionals and patients. Although there is a general understanding of the importance of testing, students express fear regarding the impact of positive results on their careers and emphasize the need for education to mitigate stigma. The findings aim to inform medical ethics education and provide insights into how future doctors navigate the complexities of HIV testing and disclosure.
![. By examining and identifying some of the beliefs and
attitudes surrounding such dilemmas, this information
can be of help to medical educators as they work with
medical students and their clinical preceptors to resolve
many of the social and ethical problems associated with
the stigma of HIV disclosure, while improving the
overall health of individuals and communities.
Correspondence: J. M. Aultman, Department of Behavioral and
Community Health Sciences, Northeastern Ohio Universities
College of Medicine
and Pharmacy, 4209 State Route 44, PO Box 95, Rootstown, OH
44272-0095, USA. Tel: 330-325-6113; fax: 330-325-5911;
email:
[email protected]
e50 ISSN 0142–159X print/ISSN 1466–187X online/11/010050–
7 � 2011 Informa UK Ltd.
DOI: 10.3109/0142159X.2011.530311
health departments, and clinician offices. Every state, along
with Guam, Puerto Rico, and the US Virgin Islands offers
confidential testing, where a person’s name is recorded with
test results, and 45 states including Guam and Puerto Rico,](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-5-2048.jpg)
![especially given the low probability of transmission. In 1991,
CDC recommended that infected HCWs with HIV or Hepatitis
B should not perform exposure prone procedures unless they
have ‘‘sought council from an expert review panel and [have]
been advised under what circumstances, if any, they may
continue to perform these procedures.’’ The CDC defined an
exposure-prone procedure to include ‘‘digital palpitation of a
needle tip in a body cavity or the simultaneous presence of the
health care worker’s fingers and a needle or other sharp
instrument or object in a poorly visualized anatomic site.’’ And,
even if the panels permit them to practice, it is recommended
that HCWs must still inform patients of their serologic status
(Gostin 2000). The American Medical Association’s policy on
HIV disclosure reads, ‘‘HIV infected physicians should disclose
their HIV seropositivity to a public health officer or a local
review committee, and should refrain from doing procedures
that pose a significant risk of HIV transmission, or perform
those procedures only with the consent of the patient and the](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-10-2048.jpg)
![would say mandatory. It’s just like. . .like our pap smears and
we test for that annually, and it’s not stigmatized. I don’t see
why we couldn’t do the same thing with HIV. Encourage
women and men to get their annual HIV test if they, or you
know, at least every few years. . .’’
Second-year students generally thought that so long as laws
(or guidelines) were in place to protect discrimination,
healthcare professionals and students should be mandatorily
tested. A female second-year student, echoing the same
sentiment, suggested that testing be anonymous and confi-
dential if it were to be mandatory. Another second-year
student felt that one would be more likely to pay attention [to
universal precautions] if a person’s HIV status were known.
While first- and second-year students from both medical
schools indicated the stigma would be greatly reduced with
mandatory testing, third- and fourth-year students felt that
discrimination would occur and the stigma would continue to
exist, even though ‘‘HIV is no longer a death sentence.’’](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-24-2048.jpg)
![One third-year student suggested that physicians disclose
their status in order to send the message to patients that they
too need to take precautions. Another third-year student
reported ‘‘We need to learn personal responsibility not just
with universal precautions but with whatever status we have.’’
A fourth-year student at one medical school placed himself in
the shoes of his patients and reported, ‘‘If I was a patient, I
would want to know no matter what kind of doctor [was
treating me].’’ Six students questioned why even discuss HIV
as a threat, since the threat is so slim and prophylaxis is
available. Knowing hepatitis was a greater threat, these
students could not understand why HIV is still an issue.
Three out of 10 fourth-year medical students believe the
patient has a right to know. The majority of third- and fourth-
year students believe that disclosure will not help the
healthcare professional or his or her patients, since the risk
of transmission is very slim.
Discussion](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-29-2048.jpg)
![Evaluation in the Office of Academic Affairs at the Boonshoft
School of
Medicine at Wright State University.
References
Angell M. 1991. A dual approach to the AIDS epidemic. New
Engl J Med
324:1498–1500.
Blumenreich GA. 1993 [Internet]. The law and the AIDS-
infected healthcare
worker. American Medical Association Legal Briefs. Available
from:
http://www.aana.com/Resources.aspx?ucNavMenu_TSMenuTarg
etID=54
&ucNavMenu_TSMenuTargetType=4&ucNavMenu_TSMenuID=
6&id=
2411&
Center for Disease Control 2005 [Internet]. Current Status of
HIV Infection
Surveillance, January 2005. [Accessed 2008 November 11].
Available
from: http://www.hhs.gov/asl/testify/t050623a.html
Center for Disease Control 2006 [Internet]. MMWR Reports.
55(RR14):1–17.](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-39-2048.jpg)
![[Accessed 2008 November 11]. Available from:
http://www.cdc.gov/
mmwr/preview/mmwrhtml/rr5514a1.htm?s_cid=
D’Amelio R, Tuerlings E, Perito O, Biselli R, Natalicchio S,
Kingma S. 2001.
A global review of legislation on HIV/AIDS: The issue of HIV
testing.
JAIDS 28:173–179.
Dixon-Mueller R. 2007. The sexual ethics of HIV testing and
the rights and
responsibilities of partners. Stud Fam Plann 38:284–296.
Evans JK, Bingham JS, Prat K, Carne CA. 1993. Attitudes of
medical students
to HIV and AIDS. Genitourin Med 69(5):377–380.
Fost N. 2000. Patient access to information on clinicians
infected with
blood-borne pathogens. J Am Med Assoc 284:1696–1698.
Galletly CL, Pinkerton SD, Petroll AE. 2008. CDC
recommendations for opt-
out testing and reactions to unanticipated HIV diagnoses. AIDS
Patient
Care STDS 22:189–193.](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-40-2048.jpg)
![Gerberding JL. 1996. The infected healthcare provider. New
Engl J Med
334:594–595.
Gostin LA. 2000. Proposed national policy on health care
workers living
with HIV/AIDS and other blood-borne pathogens. J Am Med
Assoc
284:1965–1970.
Gostin LA. 2002. Rights and duties of HIV infected health care
profes-
sionals. Health Care Anal 10:67–85.
Kagan I, Ovadia KL, Kaneti T. 2008. Physicians’ and nurses’
views on
infected health care workers. Nurs Ethics 15:573–585.
LeBlanc B. 2002 [Internet]. Does the duty to disclose include
personal
disclosure by professionals? Professional practice and liability
on the
net, 4(1). [Accessed 2008 November 11]. Available from: http://
www.sml-law.com/publications/newsletters-
detail.asp?DocID=2326
Li L, Wu Z, Wu S, Lee SJ, Rotheram-Borus MJ, Detels R, Jia](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-41-2048.jpg)
![M, Sun S. 2007.
Mandatory HIV testing in China: The perception of health-care
providers. Int J STD AIDS 18(7):476–481.
Perry JL, Pearson RD, Jagger J. 2006. Infected health care
workers and
patient safety: A double standard. Am J Infect Control 34:313–
319.
Shernoff M. 1996. Physicians living with HIV/AIDS. J Int
Assoc Physicians
AIDS Care 2(11). [Accessed 2008 November 13]. Available
from: http://
www.thebody.com/content/art2467.html
Tesoriero JM, Battles HB, Heavner K, Leung SY, Nemeth C,
Pulver W,
Birkhead GS. 2008. The effect of name-reporting and partner
notifica-
tion on HIV testing in New York state. Am J Public Health
98:728–735.
Tuboku-Metzger J, Chiarello L, Sinkowitz-Cochran RL, Casano-
Dickerson A,
Cardo D. 2005. Public attitudes and opinions toward physicians
and
dentists infected with bloodborne viruses: Results of a national](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-42-2048.jpg)
![stigma
Introduction
It is estimated worldwide that 2.1 million children younger than
15 years of age are living with HIV. Of these 1.8 million
children are living in Sub-Saharan Africa. The number of newly
infected children worldwide is estimated to be 430 000, with an
estimated number of 390 000 children living in the Sub-Saharan
African countries. Over 7400 new HIV infections arose on a day
in 2008. More than 97% were in low- and middle-income
countries and about 1200 cases of infections were in children
under 15 years of age. Approximately 6200 were in adults aged
15 years and older, of whom almost 48% were women and about
40% were young people aged 15-24 years of age (UNAIDS
2009).
South Africa is experiencing one of the largest HIV epidemics
in the world. In
2006 about 29.1% of pregnant women attending government
antenatal clinics were
*Email: [email protected]
ISSN 1351-1610 print/ISSN 1469-8412 online
# 2011 Interdisciplinary Centre for Comparative Research in the
Social Sciences and ICCR Foundation DOI:
10.1080/13511610.2011.553506
http://www.informaworld.com
HIV-positive (National Department of Health, South Africa
2008). Vertical transmission has resulted in a large burden of
pediatric HIV disease and the reversal of gains achieved in
reducing child mortality (Horwood et al. 2010). In South Africa,
HIV causes over 40% of child deaths (Bradshaw et al., 2003).
HIV-related illness and deaths have had a devastating effect on](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-45-2048.jpg)


![disclosure to a child. Increasing availability of therapy for HIV
across the world presses the issue of disclosure to the child.
Even so, disclosure for children who are HIV-positive due to
vertical transmission continues to be very difficult. There is a
lack of interventions that consider guidelines for healthcare
professionals, parents or persons involved with taking care of
HIV-positive children. These interventions should be designed
in an understanding manner towards the culture where they
might be implemented and be as appropriate in the view of
integrating different family structures and the child’s
development.
Keywords: HIV vertical transmission; disclosure; child; parent;
stigma
Introduction
It is estimated worldwide that 2.1 million children younger than
15 years of age are living with HIV. Of these 1.8 million
children are living in Sub-Saharan Africa. The number of newly
infected children worldwide is estimated to be 430 000, with an
estimated number of 390 000 children living in the Sub-Saharan
African countries. Over 7400 new HIV infections arose on a day
in 2008. More than 97% were in low- and middle-income
countries and about 1200 cases of infections were in children
under 15 years of age. Approximately 6200 were in adults aged
15 years and older, of whom almost 48% were women and about
40% were young people aged 15-24 years of age (UNAIDS
2009).
South Africa is experiencing one of the largest HIV epidemics
in the world. In
2006 about 29.1% of pregnant women attending government
antenatal clinics were
*Email: [email protected]
ISSN 1351-1610 print/ISSN 1469-8412 online](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-64-2048.jpg)
![Correspondence: J. M. Aultman, Department of Behavioral and
Community Health Sciences, Northeastern Ohio Universities
College of Medicine and Pharmacy, 4209 State Route 44, PO
Box 95, Rootstown, OH 44272-0095, USA. Tel: 330-325-6113;
fax: 330-325-5911; email: [email protected]
e50 ISSN 0142–159X print/ISSN 1466–187X
online/11/010050–7 © 2011 Informa UK Ltd.
DOI: 10.3109/0142159X.2011.530311
J. M. Aultman & N. J. Borges
The
ethics
of
HIV
testing
and
disclosure
e
52
e
51
health departments, and clinician offices. Every state, along
with Guam, Puerto Rico, and the US Virgin Islands offers](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-86-2048.jpg)
![consensus as to whether disclosure is valuable, especially given
the low probability of transmission. In 1991, CDC
recommended that infected HCWs with HIV or Hepatitis B
should not perform exposure prone procedures unless they have
‘‘sought council from an expert review panel and [have] been
advised under what circumstances, if any, they may continue to
perform these procedures.’’ The CDC defined an exposure-
prone procedure to include ‘‘digital palpitation of a needle tip
in a body cavity or the simultaneous presence of the health care
worker’s fingers and a needle or other sharp instrument or
object in a poorly visualized anatomic site.’’ And, even if the
panels permit them to practice, it is recommended that HCWs
must still inform patients of their serologic status (Gostin
2000). The American Medical Association’s policy on HIV
disclosure reads, ‘‘HIV infected physicians should disclose
their HIV seropositivity to a public health officer or a local
review committee, and should refrain from doing procedures
that pose a significant risk of HIV transmission, or perform
those procedures only with the consent of the patient and the
permission of the local review committee.’’ Furthermore, ‘‘A
physician who has HIV disease or who is seropositive should
consult colleagues as to which activities the physician can
pursue without creating a risk to patients’’ (Blumenreich 1993).
Marcia Angell in ‘‘A Dual Approach to the AIDS Epidemic,’’
wrote that patients have a right to know whether a doctor or
nurse who performs invasive procedures is infected with HIV.
Infected HCWs should refrain from invasive procedures, or
should expect to have reasonable alternative work
(Blumenreich 1993). Nevertheless, the 1995 Clinton adminis-
tration instructed CDC to review its guidelines that arbitrarily
restrict HIV infected HCWs, which possibly lead to
discrimination.
Critics, such as American Law Professor, Gostin, have
proposed new national policies, emphasizing patient safety by
ensuring that infection control procedures are systematically
implemented in healthcare settings, which would focus on](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-89-2048.jpg)

![reported, ‘‘I think I would lean towards HIV testing be
voluntary instead of mandatory. I really value having individ-
ual rights.’’ However, another first-year student stated, ‘‘I
would say mandatory. It’s just like.. .like our pap smears and
we test for that annually, and it’s not stigmatized. I don’t see
why we couldn’t do the same thing with HIV. Encourage women
and men to get their annual HIV test if they, or you know, at
least every few years.. .’’
Second-year students generally thought that so long as laws (or
guidelines) were in place to protect discrimination, healthcare
professionals and students should be mandatorily tested. A
female second-year student, echoing the same sentiment,
suggested that testing be anonymous and confi- dential if it
were to be mandatory. Another second-year student felt that one
would be more likely to pay attention [to universal precautions]
if a person’s HIV status were known. While first- and second-
year students from both medical schools indicated the stigma
would be greatly reduced with mandatory testing, third- and
fourth-year students felt that discrimination would occur and
the stigma would continue to exist, even though ‘‘HIV is no
longer a death sentence.’’
More than half of students (63%, or 34 out of 54 clinical and
non-clinical) interviewed at both medical schools explicitly
argued that individual rights are critical. If tests were manda-
tory, the right to privacy should be upheld to protect the
student or healthcare professional from negative conse-
quences, such as employment and insurance discrimination.
These students also indicated that mandatory testing would be a
waste of resources, since it is a common belief among students
and healthcare professionals that ‘‘we do not typically engage
in risky behaviors, such as unprotected sex, or fail to use
universal precautions’’.](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-96-2048.jpg)
![Physician disclosure
If a physician has HIV, do you think he/she should disclose this
to his/her patients? Please explain why or why not.
First-year students at one medical school felt that if there is a
risk, then the physician should disclose his or her HIV status.
First- and second-year students at both medical schools believed
that it is up to the physician to disclose. One first- year student
at another medical school exclaimed that I am ‘‘too shocked
even to imagine’’ this could happen to a physician. Another
first-year student believed that so long a physician can practice
medicine, disclosing such personal information to a patient is
acceptable. A third student believed that disclosure should
depend on the specialty of the profession. A male second-year
student at one medical
school ‘‘would feel guilty’’ if he did not disclose his HIV status
to patients.
Those first- and second-year students who believe that
physicians should not disclose their HIV status to patients
explained that ‘‘the patient is not caring for the doctor,’’ or that
it is ‘‘not professional to disclose personal things.’’ Some first-
and second-year students indicated that due to the potential
loss of clients, a physician should not disclose his or her HIV
status. A second-year student stated ‘‘if you are an HIV surgeon
you wouldn’t be making the money because you would be
limited to only surgeries that involve only HIV patients.’’
One third-year student suggested that physicians disclose their
status in order to send the message to patients that they too need
to take precautions. Another third-year student reported ‘‘We
need to learn personal responsibility not just with universal
precautions but with whatever status we have.’’ A fourth-year
student at one medical school placed himself in the shoes of his
patients and reported, ‘‘If I was a patient, I would want to know
no matter what kind of doctor [was treating me].’’ Six students
questioned why even discuss HIV as a threat, since the threat is
so slim and prophylaxis is available. Knowing hepatitis was a](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-98-2048.jpg)
![conflicting personal and professional values and interests.
Declaration of interest: The authors report no conflicts of
interest. The authors alone are responsible for the content and
writing of this article.
Note
1. Anonymous testing uses code numbers to identify your test.
Your name is never used. You use the code to get your results.
You are the only person who knows your results. With
anonymous testing, you have complete control in deciding who
to tell and when. With confidential testing, your name is
recorded and linked to your test results. Even though this
information is kept private, others may have access to this
information, including health care providers, your insurance
company, and the health department.
Notes on contributors
JULIE M. AULTMAN, PhD, is a Bioethicist and an Associate
Professor of Behavioral Sciences at Northeastern Ohio
Universities College of Medicine and Pharmacy.
NICOLE J. BORGES, PhD, is an Associate Professor in the
Department of Community Health and Assistant Dean, Medical
Education Research and Evaluation in the Office of Academic
Affairs at the Boonshoft School of Medicine at Wright State
University.
References
Angell M. 1991. A dual approach to the AIDS epidemic. New
Engl J Med 324:1498–1500.
Blumenreich GA. 1993 [Internet]. The law and the AIDS-
infected healthcare worker. American Medical Association
Legal Briefs. Available from:](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-103-2048.jpg)
![http://www.aana.com/Resources.aspx?ucNavMenu_TSMenuTarg
etID=54
&ucNavMenu_TSMenuTargetType=4&ucNavMenu_TSMenuID=
6&id= 2411&
Center for Disease Control 2005 [Internet]. Current Status of
HIV Infection Surveillance, January 2005. [Accessed 2008
November 11]. Available from:
http://www.hhs.gov/asl/testify/t050623a.html
Center for Disease Control 2006 [Internet]. MMWR Reports.
55(RR14):1–17. [Accessed 2008 November 11]. Available from:
http://www.cdc.gov/
mmwr/preview/mmwrhtml/rr5514a1.htm?s_cid=
D’Amelio R, Tuerlings E, Perito O, Biselli R, Natalicchio S,
Kingma S. 2001. A global review of legislation on HIV/AIDS:
The issue of HIV testing. JAIDS 28:173–179.
Dixon-Mueller R. 2007. The sexual ethics of HIV testing and
the rights and responsibilities of partners. Stud Fam Plann
38:284–296.
Evans JK, Bingham JS, Prat K, Carne CA. 1993. Attitudes of
medical students to HIV and AIDS. Genitourin Med 69(5):377–
380.
Fost N. 2000. Patient access to information on clinicians
infected with blood-borne pathogens. J Am Med Assoc
284:1696–1698.
Galletly CL, Pinkerton SD, Petroll AE. 2008. CDC
recommendations for opt- out testing and reactions to
unanticipated HIV diagnoses. AIDS Patient Care STDS 22:189–
193.
Gerberding JL. 1996. The infected healthcare provider. New
Engl J Med 334:594–595.
Gostin LA. 2000. Proposed national policy on health care
workers living with HIV/AIDS and other blood-borne
pathogens. J Am Med Assoc 284:1965–1970.
Gostin LA. 2002. Rights and duties of HIV infected health care
profes- sionals. Health Care Anal 10:67–85.](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-104-2048.jpg)
![Kagan I, Ovadia KL, Kaneti T. 2008. Physicians’ and nurses’
views on infected health care workers. Nurs Ethics 15:573–585.
LeBlanc B. 2002 [Internet]. Does the duty to disclose include
personal disclosure by professionals? Professional practice and
liability on the net, 4(1). [Accessed 2008 November 11].
Available from: http:// www.sml-
law.com/publications/newsletters-detail.asp?DocID=2326
Li L, Wu Z, Wu S, Lee SJ, Rotheram-Borus MJ, Detels R, Jia
M, Sun S. 2007. Mandatory HIV testing in China: The
perception of health-care providers. Int J STD AIDS
18(7):476–481.
Perry JL, Pearson RD, Jagger J. 2006. Infected health care
workers and patient safety: A double standard. Am J Infect
Control 34:313–319.
Shernoff M. 1996. Physicians living with HIV/AIDS. J Int
Assoc Physicians AIDS Care 2(11). [Accessed 2008 November
13]. Available from: http://
www.thebody.com/content/art2467.html
Tesoriero JM, Battles HB, Heavner K, Leung SY, Nemeth C,
Pulver W, Birkhead GS. 2008. The effect of name-reporting and
partner notifica- tion on HIV testing in New York state. Am J
Public Health 98:728–735. Tuboku-Metzger J, Chiarello L,
Sinkowitz-Cochran RL, Casano-Dickerson A, Cardo D. 2005.
Public attitudes and opinions toward physicians and dentists
infected with bloodborne viruses: Results of a national survey.
Am J Infect Control 33:299–303.
Weiss ES, Makary MA, Wang T, Syin D, Pronovost PJ, Chang
D, Cornwell EE. 2005. Prevalence of blood-borne pathogens in
an urban, university- based general surgical practice. Ann Surg
241:803–319.
Copyright of Medical Teacher is the property of Taylor &
Francis Ltd and its content may not be copied or emailed to
multiple sites or posted to a listserv without the copyright
holder's express written permission. However, users may print,
download, or email articles for individual use.](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-105-2048.jpg)
![Norman, Chopra, & Kadiyala, 2007; Olley, Seedat, & Stein,
2004; Sagay et al., 2006; Skogmar et al., 2006) and some
research describes disclosure to children of the child’s own
HIV-positive status (Kouyoumdjian, Meyers, & Mtshizana,
2005; Myer, Moodley, Hendricks, & Cotton, 2006). A review of
US studies found that by age 12-13 years, 84% of HIV- positive
mothers had disclosed their own HIV status to their children
and mean ages of children disclosed to ranged from 7 to 10
years (Murphy, Steers, & Dello Stritto, 2001). A Belgian study
found that disclosure of a parent HIV-positive status among
African migrant families was lower than disclosure among
European families (5% compared to 20.5%, respectively) (Nos-
tlinger et al., 2004). However, there is little research about
disclosure of parental HIV status to their children in Africa.
In other settings, children who have been told their parents are
HIV positive have shown lower levels of
*Corresponding author. Email: [email protected]
ISSN 0954-0121 print/ISSN 1360-0451 online
# 2009 Taylor & Francis
DOI: 10.1080/09540120802270276
http://www.informaworld.com
390
S.L. Nam
et al.
AIDS Care
391](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-108-2048.jpg)
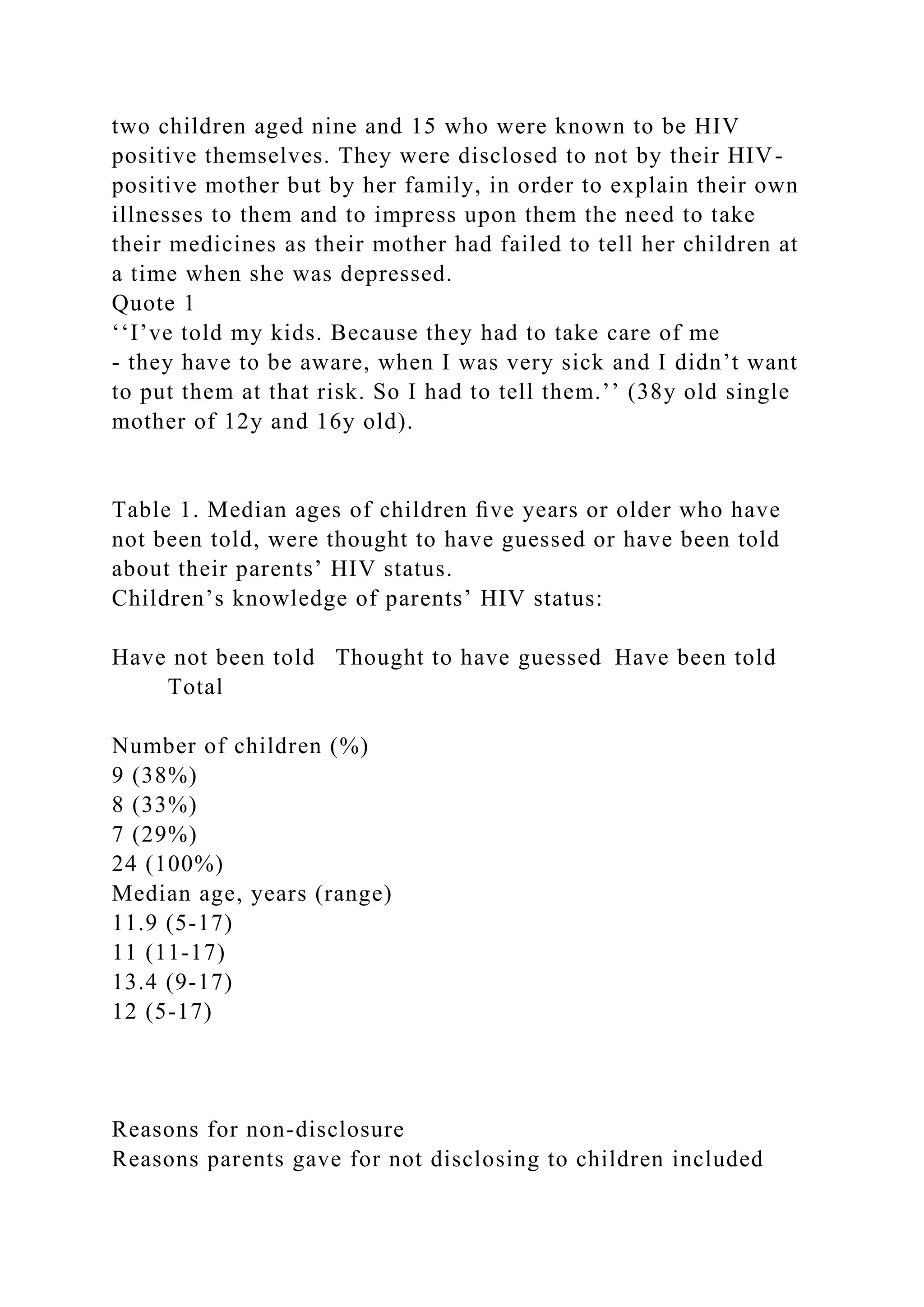
![feeling children were not old enough and not knowing how to
address the issue. Parents worried that the knowledge would be
‘‘too painful’’ for the child/ren and non-disclosure to other
people was also partly out of concern that the children might
find out from other people and face stigma as a result (Quote 2).
Quote 2
‘‘I love my kids so much - they are still at school, and I
wouldn’t like for them to be hearing that ‘your mum is
positive’, and what, what, what. All these kind of things.’’ (38y
old single mother of 14y and 16y old).
Parents who had not disclosed their status ex- pressed vague
plans to talk to their children in the future, but at the time of the
interview preferred to leave it to chance. Four parents said that
their children saw them taking the antiretrovirals and had
probably guessed what they were for, but had not discussed HIV
(Quote 3).
Quote 3
‘‘I guess the boy might know, but they [the children] don’t ever
ask me about it.’’ (48y old single mother of a 17y old son and
carer of 14y old niece).
Three of these parents said their children re- minded them to
take their pills, checked that they had taken them or brought
the pills to them with water, even though they had not told their
children about their status. This made parents think that these
children had guessed their status although they had not been
explicitly told and the parents appre- ciated this expression of
concern by their children (Quote 4).
Quote 4
‘‘I love it when my kids remind of the medication. Even [the
girl] she will just run to the bedroom and give me a glass of
water.’’ (38y old single mother of 14y and 16y).
Discussing sexual health
Parents described difficulties in addressing the issues of HIV
and sexual relationships with their children. Parents expressed a
preference to leave sexual and reproductive health topics for](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-116-2048.jpg)
![schools to address, although they were not clear about what was
taught at school in relation to these issues. Among those who
did discuss such topics, only one mother directly addressed
preventing pregnancy and protecting one- self from HIV or
other sexually transmitted infections (Quote 5).
Quote 5
‘‘I haven’t shared anything with her [my daughter]. Fortunately
I’ve never been sick. I always teach her how she should handle
herself. At school when some- body gets injured I told her that
she should she shouldn’t touch somebody’s blood and she
knows that
- she’s been told at school also. [I tell her] to respect people
who are positive - to like them. Those who come out, like
maybe she will meet one children at school and that one kid is
positive or her mum is positive - to love them it’s something
that could happen to anybody even to her. So, she has to take
care of herself. I started talking to her about relationships when
she was 9. The whole reason was [that] kids ask things. You
should guide your child to choose what kind of a friend [she]
should make. People think that when you talk to a child about a
relationship, you are teaching her to do that [develop sexual
relationships], but you are not. But you are teaching her [is]
that she should be careful in choosing friends.’’ (37y old single
mother of a 13y old).
Three parents felt it was not necessary to talk to their children
about protecting themselves from HIV because they were
‘‘good’’ children and such studious and well-behaved children
who were not considered to be at risk of HIV. Conversely,
parents felt they would be more likely to discuss the ‘‘dangers’’
of HIV and pregnancy if a child was considered ‘‘naughty’’ or
‘‘troublesome’’ or who spent time with friends whom parents
considered inappropriate (Quote 6). Two parents described
discussing HIV in general as an educational intervention or to
prepare the children for the uncertain future.
Quote 6](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-117-2048.jpg)
![‘‘The eldest girl who is 15, ah! She doesn’t really seem to be
interested in most of those things she’s the type of person who
gets 99% at school every time so in her I don’t see much of a
problem she’s quite well educated. She’s very disciplined. The
problem may arise form the last born [11y] - hey! That one she
needs lots of guidance she was clever at school, but she’s not
good, and, eish! some of [her friends] are older than her, you
know, so she joined those instead of learning [from] her sister
this one is going to give us problems, so we need to find
information and start guiding her now.’’ (38y old father of
three).
Discussion
This study found that HIV-positive parents taking
antiretrovirals had difficulty discussing their HIV status with
their children, as has been found among African immigrants
overseas (Myer et al., 2006). This study is limited by its small
sample size but even so, the depth of information gathered
reveals parental inhibition about discussing reproductive and
sexual
health with their children. In common with other research (Lee
& Rotheram-Borus, 2002), parents in this study disclosed their
HIV status in response to their own worsening health and
appeared more likely to disclose to older (median age 14 years),
rather than younger (median age 11 years) children. Parents also
confirmed findings from other studies for the reasons not to
disclose their HIV status. This included wanting children to
have a carefree childhood, children being too young, not
wanting to worry older children and not wanting children to be
hurt by the reaction of others (Nostlinger et al., 2004).
Research from the USA has found that adoles- cents who knew
their parents’ HIV status fared no worse in terms of emotional
distress, self-esteem or parental bonding than those who had not](https://image.slidesharecdn.com/201133e50e56webpapertheethicsofhivtestingan-221224055601-957c0173/75/2011-33-e50-e56WEB-PAPERThe-ethics-of-HIV-testing-an-docx-118-2048.jpg)