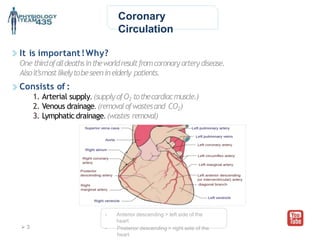
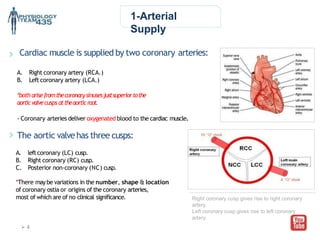
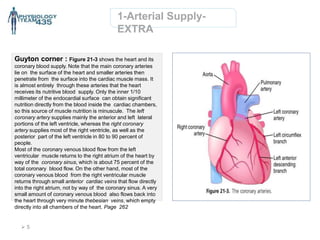
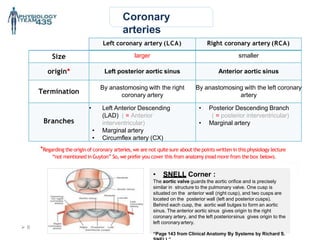
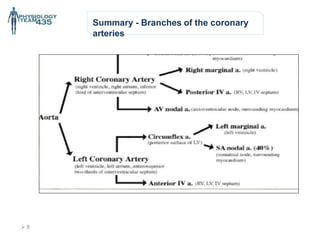
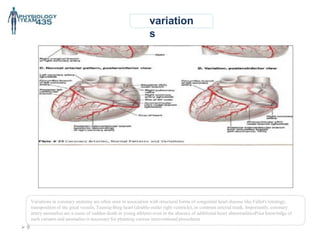
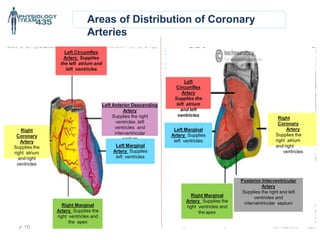
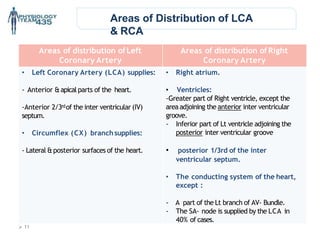
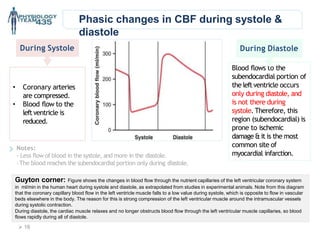
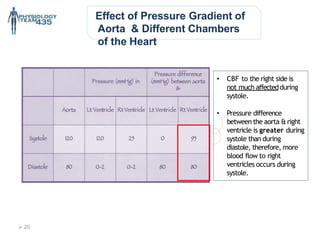
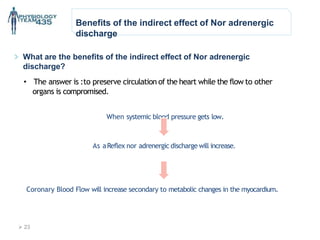
The document outlines the coronary circulation system, emphasizing the importance of coronary arteries, their branches, and their roles in supplying blood to the heart muscle. It discusses autoregulation and various factors affecting coronary blood flow, including metabolic and neural influences. Additionally, it addresses the implications of coronary artery anomalies and variations in coronary dominance related to cardiac health.