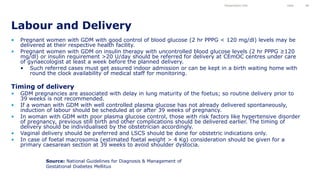
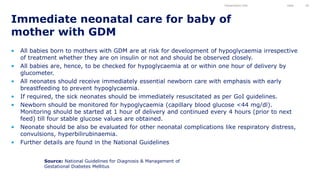
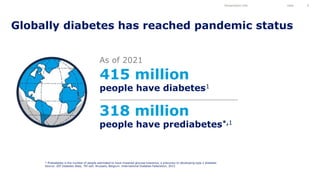
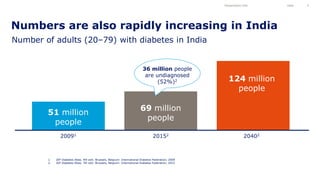
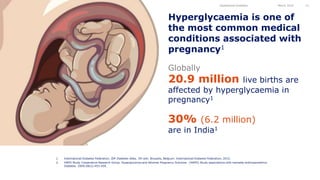
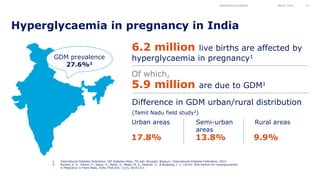
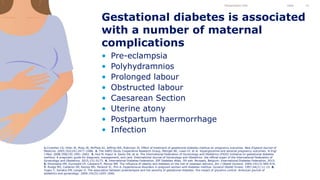
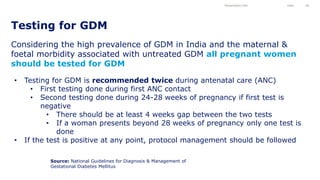
This document discusses gestational diabetes mellitus (GDM) and its diagnosis and management according to national guidelines in India. It begins with an agenda for a GDM training workshop covering diabetes as a public health crisis, the impacts of diabetes and GDM on maternal and fetal health, and national guidelines for GDM diagnosis and treatment. It then reviews globally recognized GDM risk factors and screening protocols. The document emphasizes that universal GDM screening is recommended given its high prevalence and associated maternal and fetal risks. National guidelines advise testing all pregnant women twice, with management for those testing positive.











![“In India… studies indicate that GDM may be
associated with increasing socio-economic
status, and similar trends have been found for
type 2 diabetes.”
GDM risk factors
Presentation title Date 22
Source: Nielsen, K. K., Damm, P., Kapur, A., Balaji, V., Balaji, M. S., Seshiah, V., & Bygbjerg, I. C.
(2016). Risk Factors for Hyperglycaemia in Pregnancy in Tamil Nadu, India. PloS one, 11(3), e0151311.
“…among women attending the rural health
centre a doubling in income caused an 80%
increased risk of HIP [hyperglycaemia in
pregnancy].”](https://image.slidesharecdn.com/10225385-230520193638-18629000/85/10225385-ppt-22-320.jpg)



















![Lowering episodes of hypoglycaemia with the use of
right insulin therapy
Heller et al. J Diabetes 2013; 5:482-491
Per-trial and overall analysis of all nocturnal hypoglycaemic episodes
IAsp, insulin aspart
NPH, neutral protamine Hagedorn
RHI, regular human insulin
0.1 10
Favours IAsp + NPH Favours RHI + NPH
Trial
Treatment difference
(%) [95% CI] P
1
Type 1
Type 1 and Type 2
All
Test of heterogeneity: P=0.092
Type 2
035
036
064
065
066
1634
037
1198
Fixed effects
Random effects
0.75 [0.60; 0.93] 0.01
0.69 [0.56; 0.86] <0.001
0.79 [0.59; 1.06] 0.11
0.79 [0.59; 1.06]
0.83 [0.50; 1.38]
0.12
0.97 [0.59; 1.58] 0.89
0.54 [0.24; 1.22] 0.14
0.68 [0.16; 2.85] 0.59
0.76 [0.67; 0.85] <0.001
0.76 [0.67; 0.85] <0.001
0.48
Lower rate of nocturnal hypoglycaemic episodes with insulin
aspart vs human insulin](https://image.slidesharecdn.com/10225385-230520193638-18629000/85/10225385-ppt-45-320.jpg)