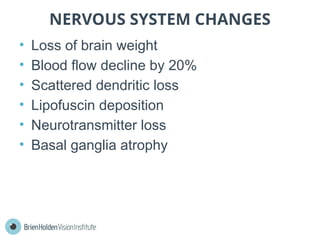
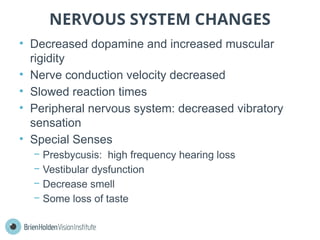
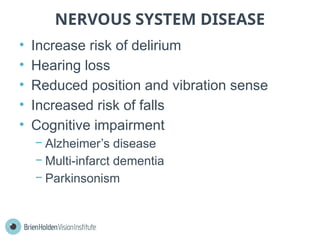
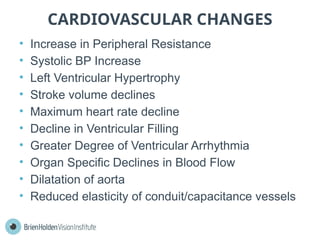
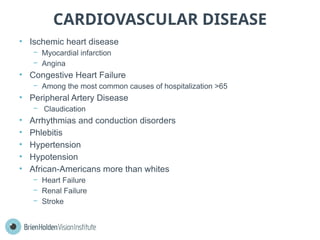
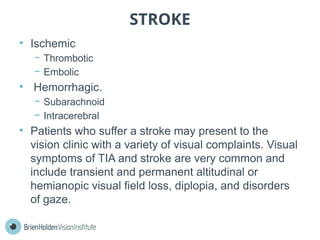
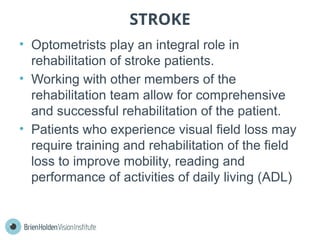
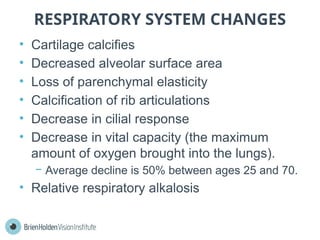
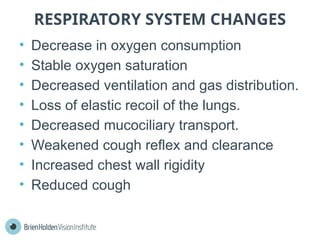
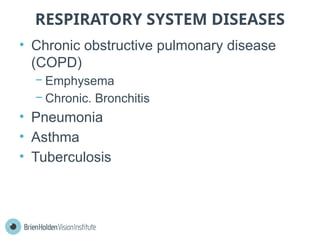
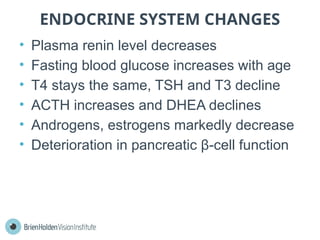
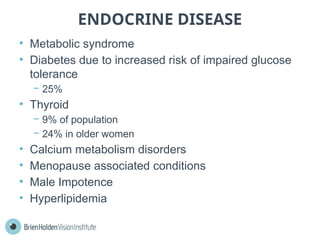
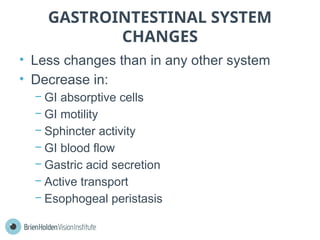
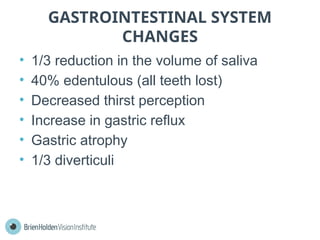
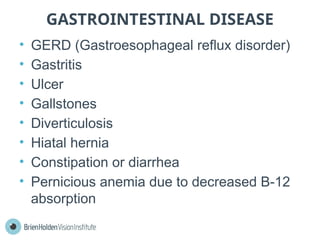
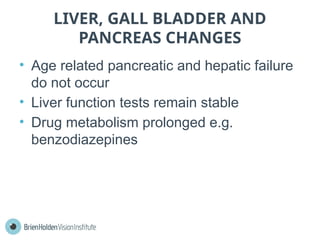
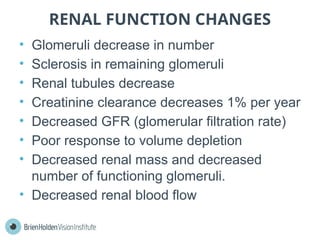
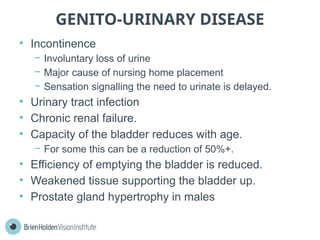
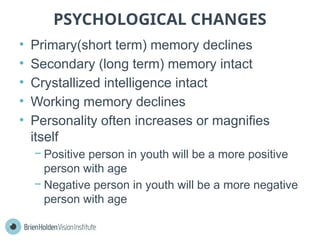
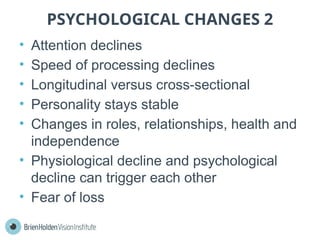
This document discusses the anatomical and physiological changes that occur with aging, detailing how various organ systems decline over time and the implications for health. It covers changes in homeostasis, skin, musculoskeletal, nervous, cardiovascular, respiratory, endocrine, gastrointestinal, renal, genito-urinary systems, and psychological aspects. Additionally, it addresses diseases associated with aging and emphasizes the role of optometrists in managing visual complaints from elderly patients.