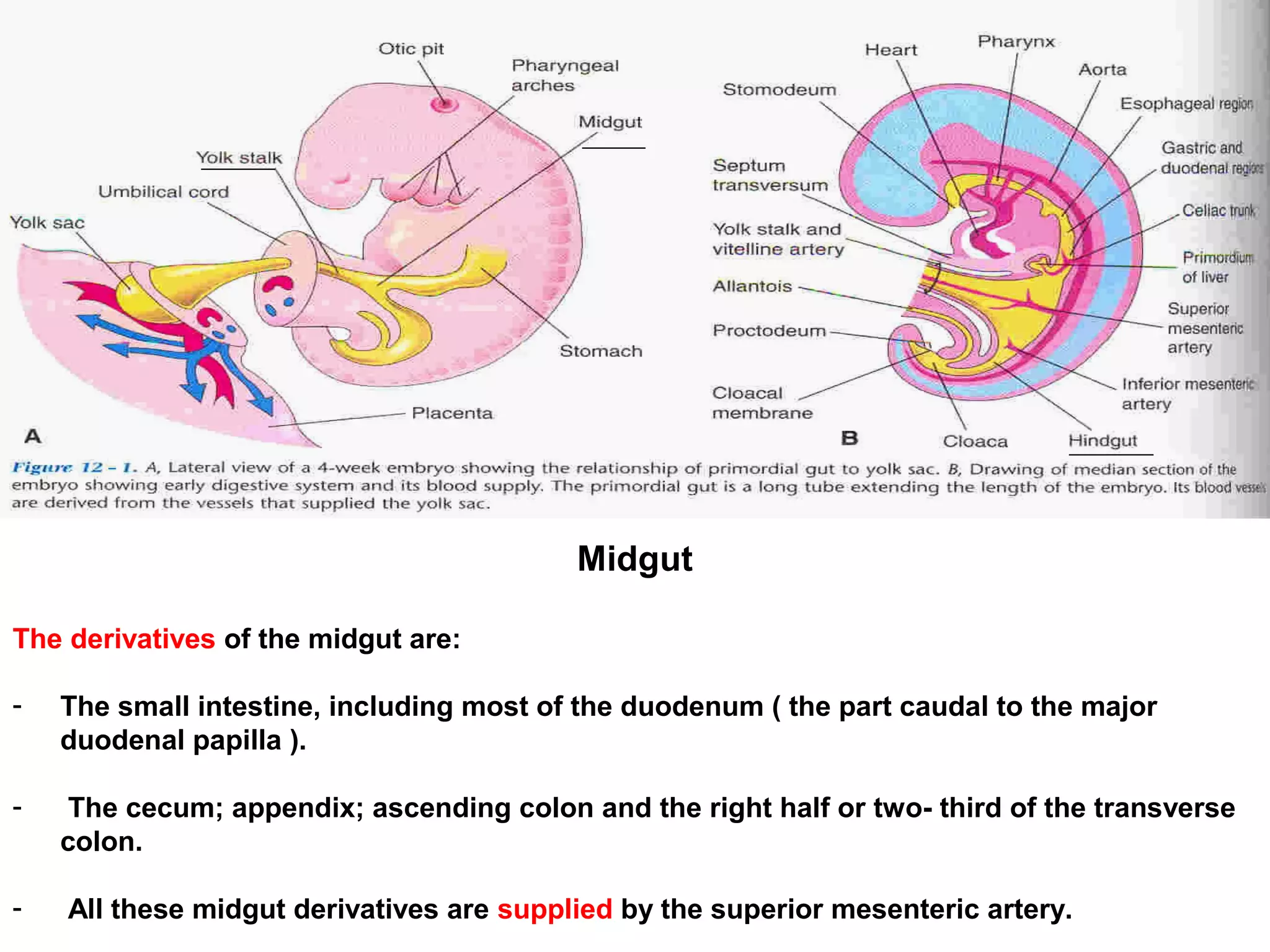
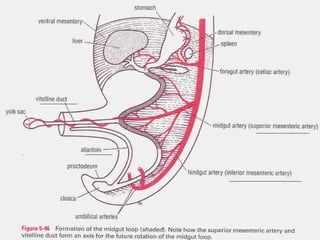
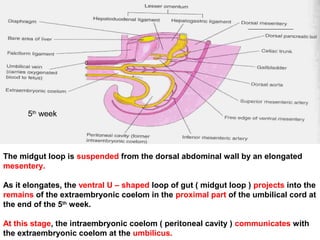
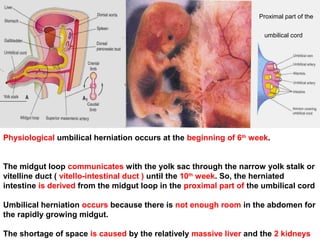
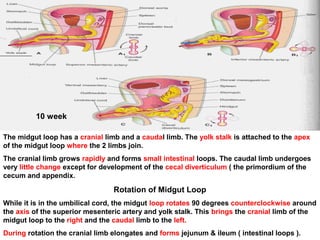
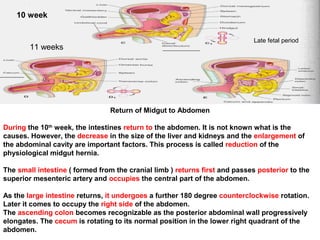
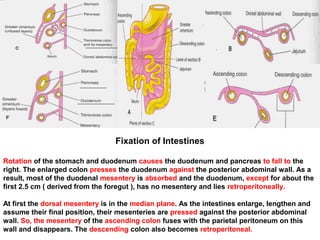
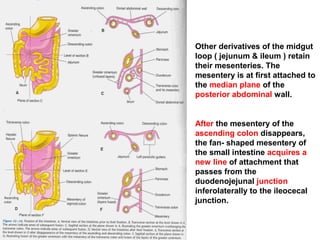
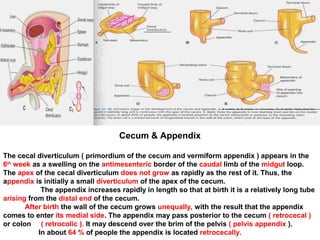
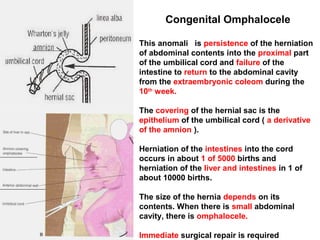
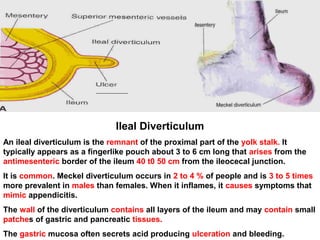
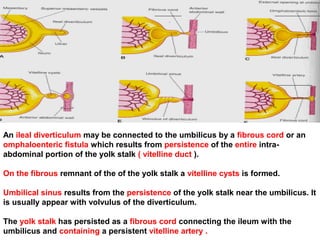
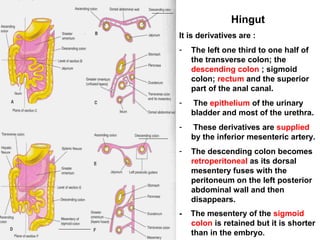
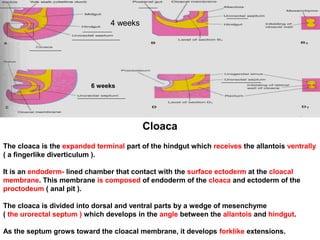
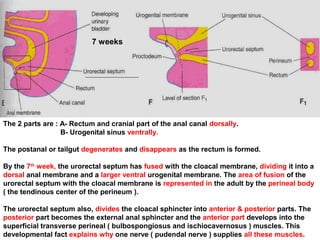
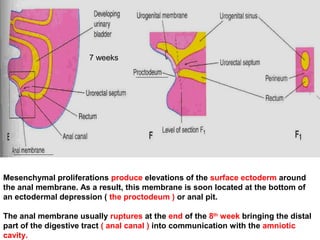
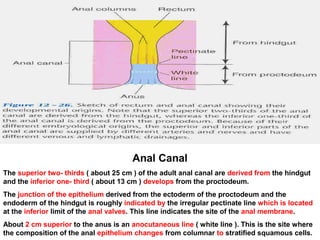
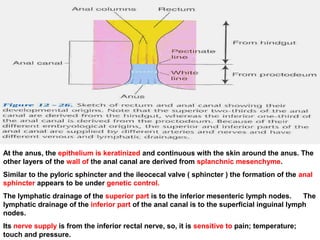
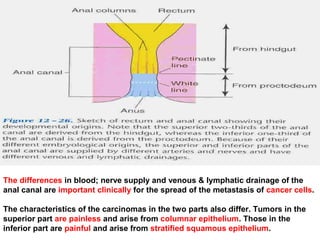
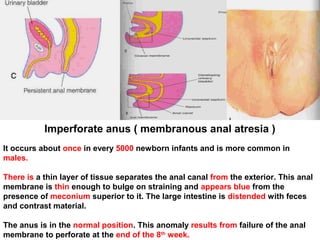
The midgut derivatives are the small intestine, cecum, appendix, ascending colon, and right half of the transverse colon. During the 5th week, the midgut loop protrudes into the umbilical cord. During the 6th week, physiological umbilical herniation occurs. Between the 10th and 11th weeks, the midgut returns to the abdomen. The hindgut derivatives are parts of the transverse colon, descending colon, sigmoid colon, rectum, and parts of the anal canal and urinary bladder. The cloaca divides into the rectum and urogenital sinus.