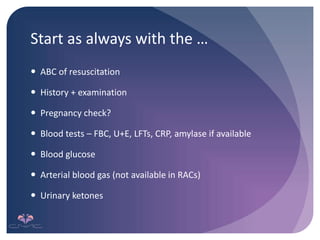
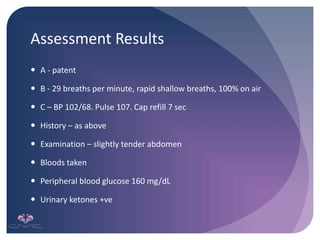
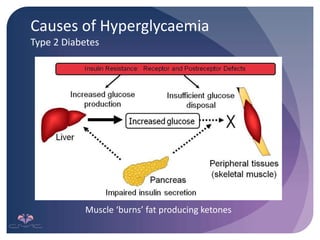
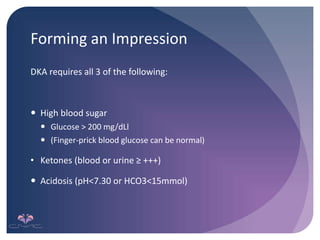
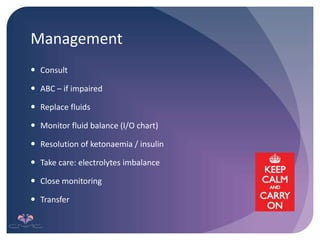
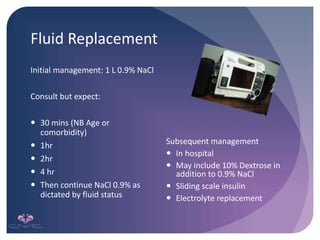
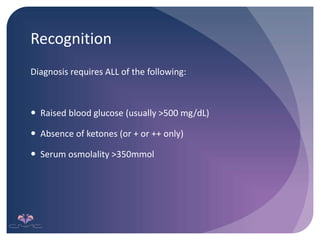
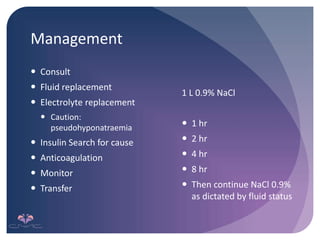
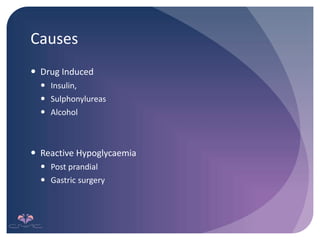
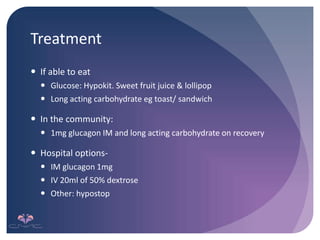
This document provides guidance on assessing and managing diabetic emergencies in remote clinics. It outlines the signs and symptoms of three potential emergencies: diabetic ketoacidosis (DKA), hyperosmolar nonketotic hyperglycemia (HONK), and hypoglycemia. For DKA and HONK, it describes the diagnostic criteria and management approach, including fluid resuscitation and monitoring. Hypoglycemia treatment focuses on oral carbohydrate intake or glucagon and dextrose injections. The document aims to equip remote nurses to initially recognize and stabilize patients until transfer to a hospital.



![References
Hariman, C. (2011) Diabetic Emergencies [Online]. Available at:
https://www.mededcoventry.com/.../Diabetes%20lecture%202011%20-%... Accessed on: 28th July 2015](https://image.slidesharecdn.com/03ediabeticemergencies-221012231811-83bf8e0e/85/03e-Diabetic-Emergencies-pptx-29-320.jpg)