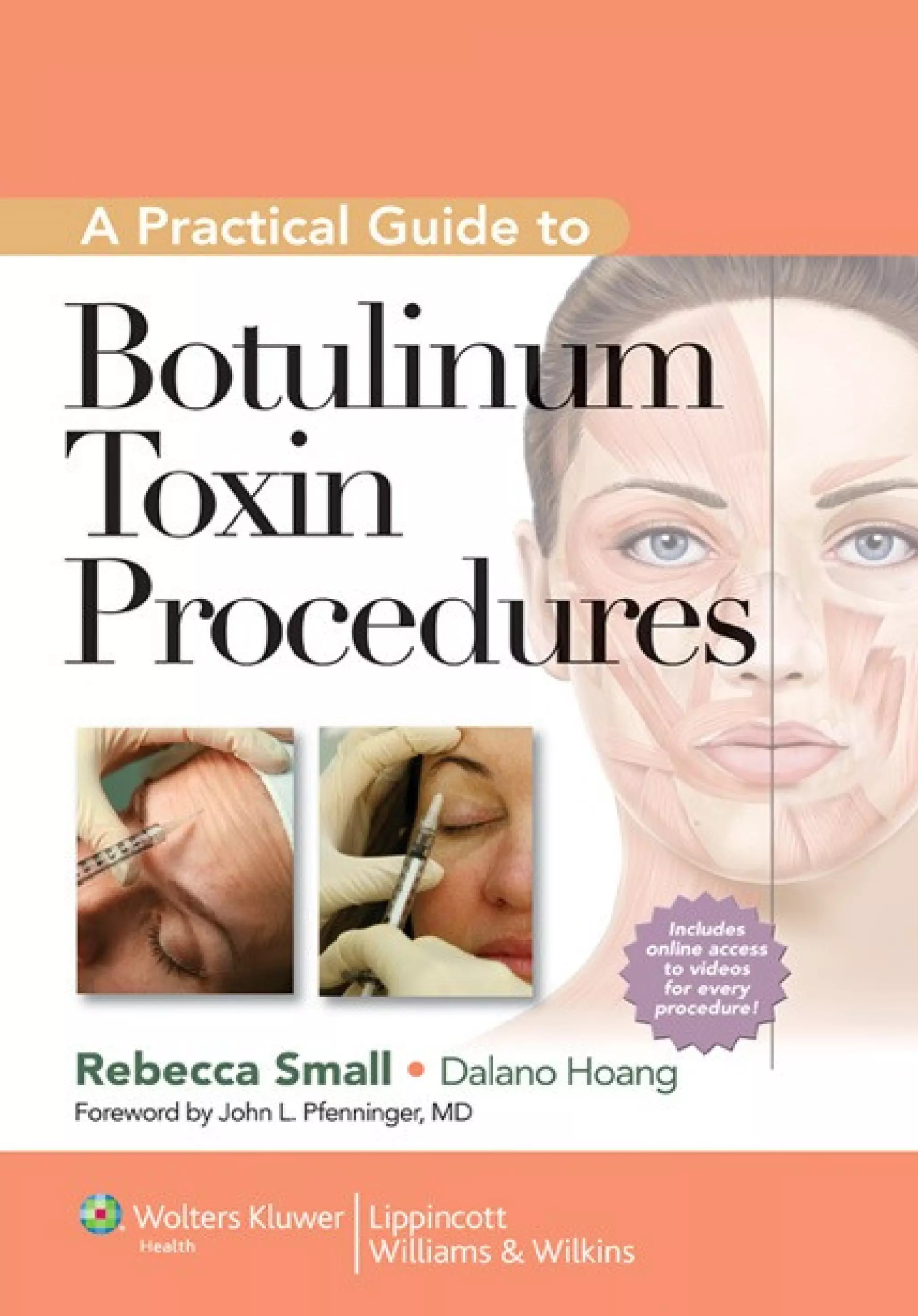
Practical Guide to Botulinum Toxin Procedures is one of four books in the new Cosmetic Procedures series. This series offers guidance to primary care practitioners who wish to expand their practice to minimally invasive cosmetic procedures. Whether the physician is just getting started or well versed in aesthetic medicine, this series can be used as a routine quick reference for current aesthetic procedures that can be readily incorporated into office practice. The series will put these cosmetic treatments into the hands of the physician the patient knows and trusts the most, and will bring primary care practitioners increased autonomy, improved patient satisfaction, and added reimbursement.
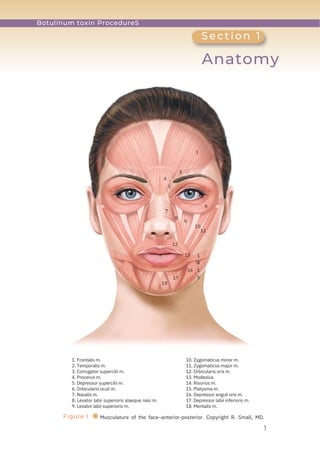
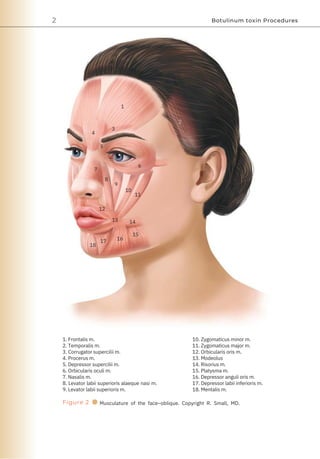
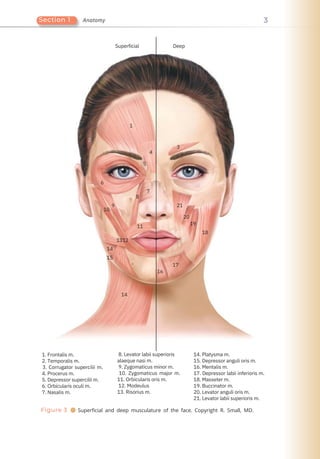
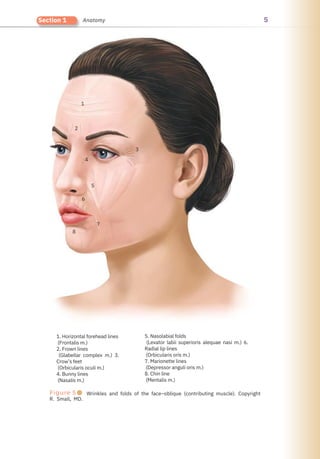
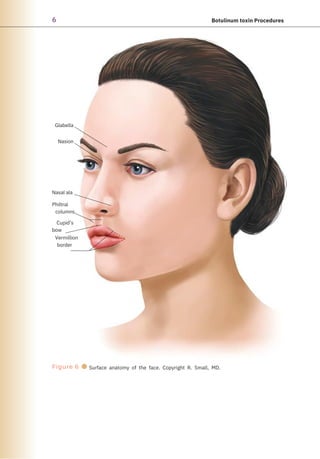
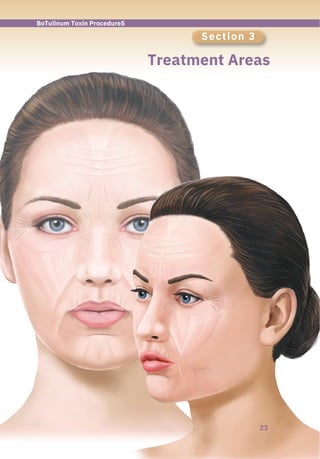
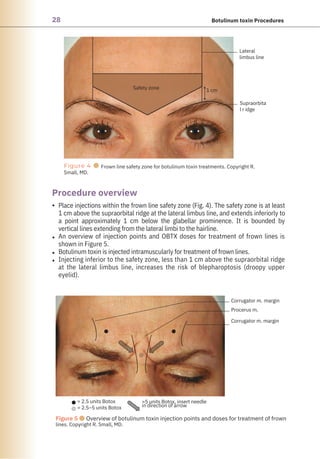
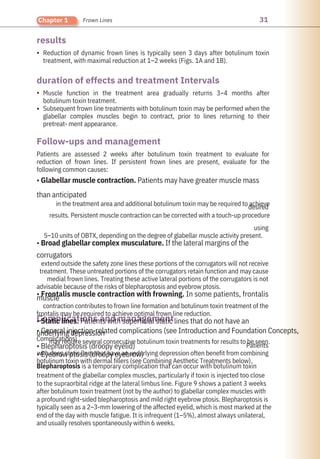
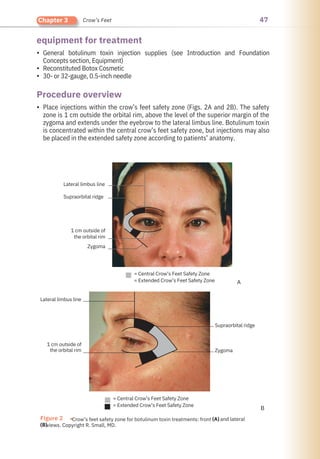
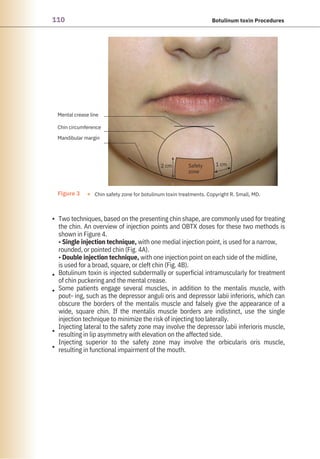
This book provides thoroughly illustrated step-by-step instructions on botulinum toxin injection procedures and advice on managing common issues seen in follow-up visits. Each chapter focuses on a single procedure and reviews all relevant anatomy, including target muscles and their functions and muscles to be avoided. Injection points and the injection Safety Zones are highlighted to help practitioners perform the procedures more effectively and minimize complication risks.
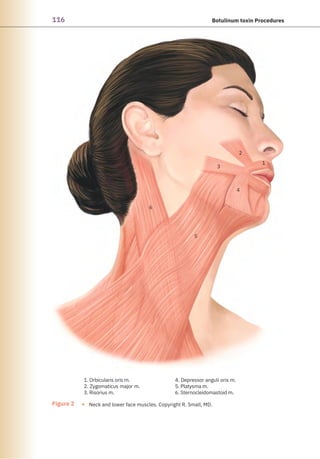
Initial chapters cover treatment in the upper third of the face for frown lines, horizontal forehead lines, and crow's feet—procedures suited for practitioners who are getting started with cosmetic botulinum toxin treatments. Subsequent chapters cover more advanced face and neck procedures and treatment of axillary hyperhidrosis.

![Acquisitions Editor: Sonya Seigafuse
Product Manager: Kerry Barrett
Production Manager: Bridgett Dougherty
Senior Manufacturing Manager: Benjamin Rivera
Marketing Manager: Kim Schonberger
Creative Director: Doug Smock
Illustrator: Liana Bauman
Production Service: Aptara, Inc.
© 2012 by LIPPINCOTT WILLIAMS & WILKINS, a WOLTERS KLUWER business
Two Commerce Square
2001 Market Street
Philadelphia, PA 19103 USA
LWW.com
All photos copyright R. Small, M.D. unless otherwise noted.
All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form by
any means, including photocopying, or utilized by any information storage and retrieval system without written
permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Mate-
rials appearing in this book prepared by individuals as part of their official duties as U.S. government employees
are not covered by the above-mentioned copyright.
Printed in China
Library of Congress Cataloging-in-Publication Data
Small, Rebecca.
A practical guide to botulinum toxin procedures / Rebecca Small ;
associate editor, Dalano Hoang.
p. cm.
Includes bibliographical references and index.
ISBN-13: 978-1-60913-147-0 (alk. paper)
ISBN-10: 1-60913-147-9 (alk. paper)
1. Botulinum toxin–Therapeutic use. 2. Injections, Intradermal.
I. Hoang, Dalano. II. Title.
[DNLM: 1. Botulinum Toxins–therapeutic use–Handbooks. 2. Cosmetic
Techniques–Handbooks. 3. Injections, Intradermal–methods–Handbooks.
QV 39]
RL120.B66S63 2012
615′.778–dc23
2011015537
Care has been taken to confirm the accuracy of the information presented and to describe generally
accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions
or for any consequences from application of the information in this book and make no warranty, expressed or
implied, with respect to the currency, completeness, or accuracy of the contents of the publication.
Application of the informa- tion in a particular situation remains the professional responsibility of the
practitioner.
The authors, editors, and publisher have exerted every effort to ensure that drug selection and dosage set
forth in this text are in accordance with current recommendations and practice at the time of publication.
However, in view of ongoing research, changes in government regulations, and the constant flow of
information relating to drug therapy and drug reactions, the reader is urged to check the package insert for
each drug for any change in indications and dosage and for added warnings and precautions. This is
particularly important when the recom- mended agent is a new or infrequently employed drug.
Some drugs and medical devices presented in the publication have Food and Drug Administration (FDA)
clearance for limited use in restricted research settings. It is the responsibility of the health care providers to
ascertain the FDA status of each drug or device planned for use in their clinical practice.
To purchase additional copies of this book, call our customer service department at (800) 638-3030 or fax orders
to (301) 223-2320. International customers should call (301) 223-2300.
Visit Lippincott Williams & Wilkins on the Internet: at LWW.com. Lippincott Williams & Wilkins customer service
representatives are available from 8:30 am to 6 pm, EST.
10 9 8 7 6 5 4 3 2 1](https://image.slidesharecdn.com/rebeccasmalldalanohoang1-apract-230614095842-17be3a76/85/A-Practical-Guide-to-Botulinum-Toxin-Procedures-5-320.jpg)






































































































































![Chin
Dysport
Neck Bands
Gummy Smile
Marionette Lines
Axillary Hyperhidrosis
Combining Aesthetic Treatments
149
Bibliography
Lowe P, Patnaik R, Lowe N. Comparison of two formulations of botulinum toxin type A for the treatment of
glabellar lines: a double-blind, randomized study. J Am Acad Dermatol. 2006;55(6):975–980.
Gassia V, Beylot C, Bechaux S, et al. Botulinum toxin injection techniques in the lower third and middle of the
face, the neck, and the decollete: the “Nefertiti lift.” [in French]. Ann Dermatol Venereol. 2009;136(suppl
4):S111–S118.
Polo M. Botulinum toxin type A (Botox) for the neuromuscular correction of excessive gingival display on smiling
(gummy smile). Am J Orthod Dentofacial Orthop. 2008;133(2):195–203.
Papel ID, Capone RB. Botulinum toxin A for mentalis muscle dysfunction. Arch Facial Plast Surg. 2001;3(4):
268–269.
Brandt FS, Boker A. Botulinum toxin for the treatment of neck lines and neck bands. Dermatol Clin. 2004;22:
159–166.
Matarasso A, Matarasso SL, Brandt FS, et al. Botulinum A exotoxin for the management of platysma bands. Plast
Reconstr Surg. 1999;103(2):645–652.
Absar MS, Onwudike M. Efficacy of botulinum toxin type A in the treatment of focal axillary hyperhidrosis.
Dermatol Surg. 2008;34(6):751–755.
Hornberger J, Grimes K, Naumann M, et al. Recognition, diagnosis, and treatment of primary focal hyperhidrosis.
J Am Acad Dermatol. 2004;51(2):274–286.
Kowalski JW, Eadie N, Daggett S. Development, validity, and reliability of the Hyperhidrosis Disease Sever-
ity Scale (HDSS). Poster Presented at: 62nd Annual Meeting of the American Academy of Dermatology;
February 6–10, 2004; Washington, DC.
Lowe NJ, Glaser DA, Eadie N, et al. Botulinum toxin type A in the treatment of primary axillary hyperhidrosis:
a 52-week multicenter double-blind, randomized, placebo-controlled study of efficacy and safety. J Am Acad
Dermatol. 2007;56(4):604–611.
Strutton DS, Kowalski JW, Glaser DA, et al. US prevalence of hyperhidrosis and impact on individuals with axillary
hyperhidrosis: results from a national survey. J Am Acad Dermatol. 2004;51(2):241–248.
Blitzer A, Binder WJ, Boyd J, et al, eds. Management of Facial Lines and Wrinkles. Philadelphia, PA. Lippincott
Williams & Wilkins. 2000.
Carruthers J, Carruthers A. A prospective, randomized, parallel group study analyzing the effect of BTX-A
(Botox) and nonanimal sourced hyaluronic acid (NASHA, Restylane) in combination compared with
NASHA (Restylane) alone in severe glabellar rhytides in adult female subjects: treatment of severe
glabellar rhytides with a hyaluronic acid derivative compared with the derivative and BTX-A. Derm Surg.
2003;29(8):802–809.
Carruthers J, Glogau RG, Blitzer A. Advances in facial rejuvenation: botulinum toxin type A, hyaluronic acid
dermal fillers, and combination therapies—consensus recommendations. Plast Reconstr Surg. 2008;121(suppl 5):
5S–30S.
Coleman KR, Carruthers J. Combination therapy with BOTOX and fillers: the new rejuvenation paradigm. Der-
matol Ther. 2006;19(3):177–188.
De Maio M. Botulinum toxin in association with other rejuvenation methods. J Cosmet Laser Ther. 2003;5(3–4):
210–212.
De Maio M. Combination Therapy—The Microlift Procedure. In: De Maio M, Rzany B, eds. Botulinum Toxin in
Aesthetic Medicine. New York, NY. Springer. 2007:127–136.
Fedok FG. Advances in minimally invasive facial rejuvenation. Curr Opin Otolaryngol Head Neck Surg.
2008;16(4):359–368.
Micheals J, Micheals B. Coupling advanced injection techniques for cosmetic enhancement. Cosmet Dermatol.
2008;21(1):31–36.](https://image.slidesharecdn.com/rebeccasmalldalanohoang1-apract-230614095842-17be3a76/85/A-Practical-Guide-to-Botulinum-Toxin-Procedures-172-320.jpg)





