TIVA practical approach and updates
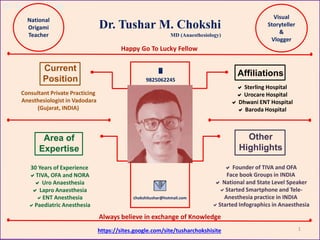
- 1. Dr. Tushar Chokshi Dr. Tushar M. Chokshi Area of Expertise Other Highlights Affiliations Current Position Consultant Private Practicing Anesthesiologist in Vadodara (Gujarat, INDIA) Sterling Hospital Urocare Hospital Dhwani ENT Hospital Baroda Hospital 30 Years of Experience TIVA, OFA and NORA Uro Anaesthesia Lapro Anaesthesia ENT Anesthesia Paediatric Anesthesia Founder of TIVA and OFA Face book Groups in INDIA National and State Level Speaker Started Smartphone and Tele- Anesthesia practice in INDIA Started Infographics in Anaesthesia 9825062245 chokshitushar@hotmail.com MD (Anaesthesiology) https://sites.google.com/site/tusharchokshisite National Origami Teacher Visual Storyteller & Vlogger Happy Go To Lucky Fellow Always believe in exchange of Knowledge 1
- 3. Dr. Tushar Chokshi 1) How many of you are giving TIVA ? 2) What is your definition of TIVA ? 3) What is your experience of TIVA ? 4) Will you give TIVA in your practice ? 3
- 4. Dr. Tushar Chokshi Lecture Outline • History – Definition • Types of TIVA – Indications • Advantages and Disadvantages – TIVA Drugs & Drug Combinations • Methods of giving TIVA – Syringe Infusion Pumps, Target Controlled Infusion(TCI) Tushar Chokshi Infusion(TCI), and Closed Loop Systems • TIVA in Different Groups of Patient – Surgical Procedures • TIVA Checklist & Monitoring – TIVA Updates & TIVA Apps • Future of TIVA 4 * Take Home message * What is your opinion
- 5. Dr. Tushar Chokshi 1656 IV injection of opium with alcohol into a dog in Oxford in leading to anaesthesia I665 Sigismund Elsholtz first attempted intravenous anaesthesia by injecting a solution of opiate in human to obtain insensibility I872 Ore, Myer, and Witzel experimented with IV chloral hydrate on animals I905 Real Intravenous anaesthesia started about when Fedorow at St. Petersburg, reported his results on 530 cases in which he used 0.75 per cent Hedonal in a normal saline solution I92I Advance in intravenous anaesthesia began with Daniel and Gabriel Bardet 1936 Pentothal changed the IV anesthesia practice of TIVA Ketamine 1962 Propofol 1977 Remifentanil 1996 Dexmedetomidine 1999 Remimazolam 2020 TIVA > 350 yrs before Inhalation > 175 yrs before 5
- 6. Dr. Tushar Chokshi 2010 2020 IV 6 In last 100 years
- 7. Dr. Tushar Chokshi It is a technique of general anesthesia Totally through Intravenous Lines Anesthesia via Intravenous agents only No Gas (Even Nitrous Oxide) or Volatile agents are used except Oxygen Given by IV boluses, in drips, by syringes or by infusion pumps Total intravenous anaesthesia (TIVA) It is a technique of general anaesthesia which uses a combination of agents given exclusively by the intravenous route without the use of inhalation agents (Gas Anaesthesia) including Nitrous Oxide, but oxygen, compressed air or helium are exception TIVA 7 ( TIVA is used in Induction as well as in Maintenance of Anaesthesia)
- 8. Dr. Tushar Chokshi 8 TIVA is Becoming Popular because
- 9. Dr. Tushar Chokshi Gives Always Side effects GAS? 9 Aerosol Droplets
- 10. Dr. Tushar Chokshi Types of TIVA 10
- 11. Dr. Tushar Chokshi With Endo Tracheal Tubes Without Endo Tracheal Tubes With Supra Glottic Airways Without Supra Glottic Airways With Nasal Airways With Oral Airways Without ETT/SGD/Nasal/Oral Airways 11
- 12. Dr. Tushar Chokshi TIVA INDICATIONS Almost in all surgical procedures Anaesthesia in non operative locations where inhalational anaesthetics are difficult Airway procedures Remote locations MH susceptible Neurosurgery & Neuro monitoring PONV risk Short procedures CT, MRI,Cardiac catheterisation Daycare Surgery Trainee teaching Patient Choice 12
- 13. Dr. Tushar Chokshi Except for a slight prick in the arm, the patient is unaware of having an anaesthetic No mask over the face No sudden concentration of gas or vapour No risk of MH Less PONV Patients wake up as it from natural sleep Very low incidence of post operative delirium Avoid distension air filled spaces in the patient’s body- so better operating conditions for surgeons Reduced stress response Better preservation of cerebral auto regulation Less chances of emergence phenomena Less operating room pollution There should be no smell of volatile agents at all in the room, and the patient is usually most grateful for not having had his system saturated with such a drug 13 TIVA
- 14. Dr. Tushar Chokshi 14 TIVA is favourable to almost all Body Systems
- 15. Dr. Tushar Chokshi Injection is irreversible Shallow respirations Possibility of not finding the vein Not having another apparatus to carry on the TIVA Incidence of awareness if not given properly Risk of bacterial contamination Environmental effect of plastic waste Disposables may be costly Caution in prolonged procedures or obese patients Pain on injection 15
- 16. Dr. Tushar Chokshi TIVA completes Anesthesia Circle 16
- 17. Dr. Tushar Chokshi TIVA Drugs 17
- 18. Dr. Tushar Chokshi TIVA drugs with their advantages • Majority of drugs used for TIVA including benzodiazepines, narcotics, propofol, ketamine, etomidate, dexmedetomidine, muscle relaxants, and other drugs are easily available in almost all the Operation theatres and outside OT • All these drugs can be given to any subset of population from paediatric to geriatric patients in easily titratable doses. 18
- 19. Dr. Tushar Chokshi 1957-1961 Dexamethasone 1886-1990 Magnesium Sulphate 1956 Paracetamol 1973-1988 Diclofenac Sodium 1961-1966 Clonidine 1980-1987 Esmolol 1920-1928 Ephedrine 1971-1985 Mephentermine 1860 Cocaine 1905 Procaine 193--1941 Tetracaine 1943-1949 Lidocaine 1950 Chloroprocaine 1960 Mepivacine 1957 Bupivacine 1980 Ropivacaine 1980 Levobupivacaine 1900 Tubocurarine Chloride 1906-1949 Suxamethonium 1947 Gallamine Triethiodide 1964 Pancuronium 1974-1983 Atracurium 1984 Vecuronium 1984 Mivacurium 1989-1995 Cisatracurium 1994 Rocuronium 1830 Chlorofom 1846 Ether 1920 Trichloroethylene 1956 Halothane 1963-1966 Enflurane 1979 Isoflurane 1970-1987 Desflurane 1971-1990 Savoflurane 1804 Morphine 1937-1943 Pethidine 1960-1968 Fentanil 1974 Sufentanil 1996 Remifentanil 1974 Carfentanyl 1961-1971 Naloxone 1930-1934 Sodium Thiopental 1962-1964-1970 Ketamine 1964-1972 Etomidate 1977-1989 Propofol 1999 Dexmedetomidine 1901 Atropine 1975 Glycopyrrolate 1964-1979 1981 Metoclopramide Ranitidine 1980-1991 Ondansetron 1959-1963 Diazepam 1963-1977 Lorazepam 1987 Flumezenil 1975-1990 Midazolam 1772 Nitrous Oxide X 1774 Oxygen 1881 Cyclopropaine X 1898 Xenon X 1996 Atipamazole 1961-1971 1982 Naloxone Doxapram 1987 Flumezenil 1931 Neostigmine 2007-2015 Sugammdex 1967 Dentrolene 2014-2020 Remimazolam Anesthesia Adjuvant IV Anesthetic Local Anesthetic Gas Opioid Premedication Inhaltion Anesthetic Benzodiazepine Muscle Relaxant Anti MH Agent Benzodiazepine Reversal Agent IV Reversal Agent Opioid Reversal Agent Relaxant Reversal Agent Opioid with Benzodiazepine I N F O G R A P H I C S A N E S T H E S I A D R U G S O F Total 66 Drugs In Use 45 Drugs Not Used In TIVA Not Used In TIVA 19 In TIVA 25 drugs
- 20. Dr. Tushar Chokshi Rapid onset of action Rapid and predictable recovery Potent and lipid-soluble Water-soluble to minimize toxicity associated with the solvent Stable in solution Chemically compatible with other drugs No perivascular sloughing if extravasated Not absorbed by plastics Does not promote bacterial growth Devoid of adverse side effects Low cost Most important it can be mixed with other anesthetic agents without any complication 20
- 21. Dr. Tushar Chokshi All Benzodiazepines Dexmedetomidine Dexamethasone Magnesium Sulphate L i d o c a i n e D i c l o f e n a c P a r a c e t a m o l TIVA DRUGS TOOLBOX C L O N I D I N E Opioids 21
- 22. Dr. Tushar Chokshi IV Anesthetic Drugs 22
- 23. Dr. Tushar Chokshi Propofol In TIVA • Prime drug in all TIVA combination • Initially TIVA dose is 2-2.5 mg/kg IV ( if use alone) • In TIVA mixture 1 mg/kg IV • In infusion 6 mg/kg/hr for maintenance • Co-administration of Propofol and Remifentanil by target-controlled infusion (TCI) is highly effective and constitutes ideal total i.v. anaesthesia Maintenance 23
- 24. Dr. Tushar Chokshi PROPOFOL Invented in 1977 In Use 1989 Switch On & Switch Off Anaesthesia Only Hypnosis, Anaesthesia & No Analgesia Propofol 1 % (10mg/ml) Propofol 2 % (20mg/ml) Milk of Amnesia Also used in Veterinary Medicine for anaesthesia Addiction and Propofol Infusion Syndrome with long-term use Milky White Solution WHO Essential Medicine Only given by IV Route Slowly No other routes are indicated Pharmacodynamics Three compartment linear model with compartments representing Plasma, Rapidly equilibrating tissues, and Slowly equilibrating tissues Indications Initiation and maintenance of Monitored Anesthesia Care (MAC) sedation Combined sedation and regional anesthesia Induction of General Anesthesia Maintenance of General Anesthesia Intensive Care Unit (ICU) sedation of intubated, mechanically ventilated patients Lie Detector test Compatibility with other Drugs Ketamine Midazolam Dexmedetomidine Fentanyl / Remifentanil Lidocaine / Dexamethasone Compatibility with other fluids 5 % Glucose 5 % Dextrose Saline 0.9 % NaCl Ringer Lactate Paracetamol Infusion Minimum Dilution 2 mg/ml Different Doses ( IV) Induction Children – 3-3.5 mg/kg Adult – 2-2.5 mg/kg Geriatric – 1-1.5 mg/kg ASA III & IV - 1 mg/kg Maintenance Children - 0.125-0.3 mg/kg/min Adult - 0.1-0.2 mg/kg/minute Geriatric - 0.05-0.1 mg/kg/min ASA III & IV - 0.05 mg/kg/min Maximum Maintenance 6-10 mg/kg/hr(Roberts regime) ICU Patient (Maximum 10 days) 0.01-0.05 mg/kg/minute TCI Model : Marsh, Diprifusor Schinder, Kataria and Paedfusor Common Side Effects Hypotension Apnea lasting 30-60 seconds Abnormal Movement Injection site burning/pain Respiratory acidosis Hypertriglyceridemia Rash and Itching Arrhythmia and Bradycardia Cardiac Output decreased Bronchospasm / Edema Phlebitis /Allergic Reaction Pancreatitis Asystole/Cardiac Arrest Seizures Contraindications Documented Hypersensitivity Egg allergy Soybean/Soy allergy Cautions Bronchial Asthma Pt. with long term NSAIDs Severe Hypovolemia or Shock EF < 30 % with Cardiac Disease Severe hepatic dysfunction Severe renal Impairment Long term infusion GI bleeds, ulcers, perforation Pregnancy and Lactation Mechanism of Action Works by increasing GABA mediated inhibitory tone in the CNS Decreases the rate of dissociation of the GABA from the receptor, thereby increasing the duration of the GABA-activated opening of the chloride channel with resulting hyper polarization of cell membrane The endocannabinoid system may contribute significantly to propofol‘s anesthetic action and to its unique properties Causes a prominent reduction in the brain's information integration capacity Pharmacokinetics Formula : C12H18O Molar mass : 178.275 g·mol−1 Protein binding : 95–99% Metabolism : Liver glucuronidation Onset of action : 15–30 seconds Elimination half-life: 1.5–31 hr Duration of action : 5–10 min Excretion: Renal Renal clearance : 120 ml/min S H O R T A C T I N G L I P O P H I L I C I V A G E N T A L S O A V I L A B L E A S M C T - L C T Pre filled Syringes 10 ml/20 ml 10 ml/20 ml 1 % as Bulb/Ampoule 50/100 ml 1 % or 2% Bulb MCT/LCT Propofol contains Soya oil, MCT, glycerol, egg lecithin, sodium hydroxide, oleic acid and water for injections Changed Anesthesia Practice Over Dose Death Main Drug in TIVA Most widely used drug In world 24
- 25. Dr. Tushar Chokshi Ketamine NMDA antagonist - Key role and main drug in TIVA - Best analgesic, amnesic and opioid sparing effect - Dose less than 0.5 mg/kg reduces postoperative analgesic needs and especially seen in opioid-tolerant patients - It has anti-hyperalgesic and anti-tolerance effects. Most popular drug for anesthesiologist across globe since 50 years Brahmashtra for anesthesiologist in TIVA 25
- 26. Dr. Tushar Chokshi Ketamine in TIVA • Only intravenous anaesthetic with hypnotic, analgesic and amnesic properties • Produces rapid hypnosis with profound analgesia and amnesia after intravenous administration of 0.5-2.0 mg/kg • It can be mixed with all types of anaesthetic and narcotic agents in single syringe • Ketamine with Medazolam (Ketomed), Ketamine with Propofol (Ketofol) and ketamine with Dex (Ketodex/ketdex) are established TIVA mixtures • One of established drug for TIVA mixture 26
- 27. Dr. Tushar Chokshi Main Features Rapid-acting general anesthetic Produce profound analgesia Normal pharyngeal-laryngeal reflexes Slightly enhanced skeletal muscle tone Cardiovascular and respiratory stimulation Transient and minimal respiratory depression. Contraindications > Angina, Stroke and very high blood pressure Psychiatric disorders, Uncontrolled Epilepsy In raised intraocular pressure & Eye injury Acute Porphyria Age less than 3 months Traceal and Laryngeal Surgery - Bioavailability – 93 -100 % - Protein binding - 53.5% -Distribution half-life 1.95 min - Half Life - 186 minutes - Elimination - urine 91 % , 3 % in feces and 6 % unchanged - Clearance rate - 95 L/h/70kg Mechanism of action Interacts with N-methyl-D-aspartate (NMDA) receptors, opioid receptors, monoaminergic receptors, muscarinic receptors and voltage sensitive Ca ion channels Does not interact with GABA receptors Selectively depress the thalamoneocortical system before significantly obtunding the more ancient cerebral centers and pathways (reticular-activating and limbic systems) - Water and Lipid Soluble - Oral ketamine broken down by bile acids - Undergoes hepatic Metabolism - It can be mixed with any TIVA drugs - Compatible with all IV fluids Other uses > Emergency Dept. > Asthma > Seizures >Pain management > Depression > Vet Anesthesia Invented in 1962 ---- NMDA receptor antagonist with Dissociative Anesthesia ---- Approved in 1970 Most Popular Anesthetic Drug of Anesthesiologists Ketamine • I V Effect Starts -2 min Last – 25 min • IM Effect Starts – 5 min Last – 4-6 hrs • Oral – 30 min C13H16ClNO More Analgesia & Less Anesthesia M/A Main Actions Increase BP Increase Salivation Bronchodilation Hallucination Agitation Catatonia Prevent opioid induced Hyperalgesia Best agent in Post anesthetic shivering Post Ketamine Double vision & Nystagmus are very common Dose Schedules 0.1-0.3 mg/kg – Analgesia 0.2-05 mg/kg – Recreational 0.4-0.8 mg/kg -- Partially dissociated 1-2 mg/kg – Fully Dissociated 1-2 mg/kg /IV – Procedural Sedation 4-8 mg/kg/IM – Procedural Sedation 0.1-0.2 mg/kg/hr – Postop Pain Relief (Infusion maximum 3 days only) IV Bioavailability -100 % IM Bioavailability – 93 % Dose Schedules 10 mg/kg /Oral – As Sedative Premedication(Bioavailability – 20 %) 0.7-0.9 mg/kg – Intrathecal (S/A) 0.2 mg/ml – Epidural for Postop pain Intra nasal 0.5-1 mg/kg (Bio-50%) Intrarectal 0.5-1 mg/kg (Bio-30%) Sublingually 0.5 -1 mg/kg (Bio-30%) Inhalation 0.5-1 mg/kg Topical Gel – 1% ketamine with other drugs Ketamine is the only drug which Is given by all routes In body U N I Q U E D R U G S C H E D U L E D R U G •Increase HR, high BP(20 %) •Increased intracranial pressure • Transient reddening of the skin • Reduced appetite, nausea • Increased salivation, vomiting •Pain, eruptions or rashes at the injection site • Tonic-Clonic movements • Double vision , involuntary eye movements, • Increased bronchial secretions • Anaphylaxis and Dependence • Cognitive Deficits • Emergence reaction Side Effect Pharmacokinetics •Rapid onset and short duration of action • Initially distributed to highly perfused brain tissues • Crosses Blood Brain barrier • Undergoes extensive redistribution • Major metabolite are norketamine and dehydronorketamine Combination • Ket+Propofol(Ketofol) • Ketamine+Dex(Dexket) • Ketamine+Fentanyl • Ketamine+Midazolam • Ketamine+Diazepam • Ket+Prof+Dex (KPD) WHO List of Essential Medicine 27
- 28. Dr. Tushar Chokshi Dexmedetomidine • Dexmedetomidine has hypnotic, sedative, and analgesic properties and is estimated to be 7-10 times more potent than clonidine • Most ideal anesthetic agent with all the properties of anesthesia • Has got opioid sparing effect • Dexket/Ketodex combination is becoming very popular in Pediatric OFA • Patients sedated, but, arousable, alert and respond without uncomfortable • They may quickly return to sedation again • Conscious Sedation as natural sleep • This drug is becoming widely popular in all part of world in all anesthesia techniques • Dose ranges from 0.5 to 1 mcg per kg according to patient status and surgery needs • Maintenance infusion is generally initiated at 0.6μ/kg/hour and titrated to achieve desired anaesthesia effects • In pediatric TIVA dex with ketamine (Ketodex) combination is mostly preferred for Endoscopic and Radiological procedures An alpha-2 agonist 28
- 29. Dr. Tushar Chokshi Sedation Anxiolysis DEXMEDETOMIDINE Analgesic Anaesthetic FDA December 1999 Market August 2000 Agonist of α2-adrenergic receptors Most ideal anesthetic agent available M/A Induces sedation by decreasing activity of noradrenergic neurons in the locus ceruleus in the brain stem, thereby increasing the activity of inhibitory gamma- aminobutyric acid (GABA) neurons in the ventrolateral preoptic nucleus Popular in pediatric TIVA with ketamine Patients sedated, but arousable, alert and respond without uncomfortable like conscious sedation No effect on Respiratory System Transient Hypertension followed by Hypotension No Direct effect on Myocardium IOP Insulin Release Overdose may cause 1st or 2nd degree AV Block - Nasal - ~ 84 % bioavailability Indications Pre Anaesthetic sedation (IM/IV) As Induction Agent In maintenance of Anaesthesia As adjuvant in TIVA Intra thecal with Regional Ane. In Post Operative Analgesia As ICU sedation(only for 24 hrs) Relative Contraindication Infusion over 24 hours In pre existing severe bradycardia Brady dysrhythemia Patient with < 30% EF Partial or Complete AV block In patients more than 65 y of age, a higher incidence of bradycardia and hypotension Compatibility - 0.9% sodium chloride in water - 5% dextrose in water - 20% mannitol - Lactated Ringer's solution - 100 mg/ml MgSo4 solution - 0.3% potassium chloride solution - With other Anesthetic agents e.g. Propofol, Ketamine, Etomidate Available as Ampoules or Bulb 50 mcg / 0.5ml 100 mcg / 1 ml 200 mcg / 2ml Sileo Gel for Dogs (Dexmedetomidine Oromucosal Gel) 0.09 mg/ml, 3 ml syringe (BIPHASIC BLOOD PRESSURE RESPONSE) (BRADYCARDIA IS BECAUSE OF DOUBLE EFFECT) (DECREASE OPIOID REQUIREMENT BY 50 %) (BETTER THAN CLONIDINE IN ALL ASPECTS) 29
- 31. Dr. Tushar Chokshi Etomidate • Excellent Cardio stable drug • Use mainly in Hemodynemically compromise patient as TIVA induction agent • For Sedation : 0.1 mg/kg up to three doses • For TIVA : 0.3 to 0.4 mg/kg IV over 30-60 seconds • In ICU : As continuous infusion 0.04 to 0.05 mg/kg/hr with continuous monitoring • In Cushing Syndrome or law Cortisol level patient 0.2 mg/kg • In Geriatric patients : 0.2 mg/kg 31
- 32. Dr. Tushar Chokshi Etomidate decrease in level of circulating cortisol IV 100 to 200 mg hydrocortisone is given before etomidate Pharmacokinetics Onset of Action : within 30 to 60 seconds Peak Effect : In 1 minute Duration : 3 to 5 minute and terminated by redistribution Protein Binding : 76 % Metabolism : Hepatic & Plasma Esterase Half-Life Distribution : 3 Minutes ( Anesthesia ) Half-Life Redistribution : 30 Minutes ( Sedation ) Half-Life Elimination : 3 hours ( Drowsiness ) Etomidate + Ketamine Mixture Most suitable mixture for short procedure Best combination for RSI in trauma and sepsis patients Good alternative in pediatric patients compare to ketofol and ketodex Both counter act each other adverse effects like myoclonus, nystagmus, injection site pain Dose is 0.1mg/kg etomidate + 1 mg/kg ketamine Mechanism of Action • Carboxylated Imidazole agent • Imidazole agent in IV anesthetic drugs • R-1-(1-ethylphenyl)imidazole-5-ethyl ester • Acts directly on the (GABA) receptor complex blocking neuroexcitation producing sedation/hypnosis/ anesthesia without analgesia • Acidic pH - 6.9, pKa – 4.2, • poorly water soluble • soluble in 35 % propylene glycol History - Janssen Pharma in 1964 at Belgium First introduced as Anti-Fungal agent - Introduced as IV Anesthetic agent (due to potent sedative properties ) - In Europe 1972 - In USA 1983 - In India 2013 Doses in different situations • For Sedation : 0.1 mg/kg up to three doses • For G/A 0.3 to 0.4 mg/kg IV over 30-60 seconds • In ICU : As continuous infusion 0.04 to 0.05 mg/kg/hr with continuous monitoring • In Cushing Syndrome or law cortisol level patients 0.2 mg/kg • In Geriatric patients : 0.2 mg/kg • In Pregnancy : 0.2 mg/kg • In Pediatric Patients : 0.1-0.3 mg/kg Available as Milky White and Clear Solution in 2 mg/kg 10 ml Bulb or MCT/LCT preparation Etomidate is most preferred drug in Hemodynamically unstable patients then any other anesthetic agents for induction of anesthesia Indications • As Sedation • As Conscious Sedation • As Hypnotic Agent • Etomidate Interview in Lie Detector Test • As Anesthetic Agent ( preferred in cardiac patients) • In Rapid Sequence Intubation (RSI) • In Cardio version as Premedication • In ICU as infusion in ventilated or nonventilated patient • As eSAM ( Etomidate Speech And Memory Test) Contra-Indications • Proven sepsis with unstable hemodynamic patients • Abnormally Low Blood Pressure even with Rx • Decreased Function of the Adrenal Gland • Hypersensitivity of Etomidate • Pediatric Patients less than 10 years age (but people have started using etomidate up to 2 years age with risk-benefit profile) • In Pregnancy try to avoid as induction agent if other anesthetic agents are available • In Geriatric Patients with caution Adverse effects • Transient Injection site pain up to 80 % patients • Skeletal Muscle movements mainly myoclonic ( peripheral limb movements ) up to 30 % patients • Opsoclonus ( uncontrolled eye movements ) • Adrenal Suppression up to 10 % patients • Hiccups • Apnea up to 90 seconds • Less frequently nausea vomiting laryngospasm, snoring, arrhythmia & increase in PaCO2 CNS – Decrease ICP, Cerebral Blood flow and Cerebral Metabolism But cerebral perfusion pressure maintained CVS -- No or Minimal changes in Heart Rate, Blood Pressure and Cardiac Output No hemodynamic changes in response to pain No effect on Sympathetic tone RS – Minimal changes in Respiratory Rate and Tidal Volume Slight elevation in arterial carbon dioxide tension (PaCO2) Transient apnea up to 90 seconds - No histamine release - Very rare allergic reactions - Hepatic and Renal blood flow decreased Administration of Drug • Never dilute Etomidate with DW in same Syringe • Preferably Large Vein for IV administration • Pre administration of lidocaine if possible (2 ml) • First dose to be completed within one arm-brain circulation (60-90 seconds ) • All muscle relaxants, benzodiazepines, narcotics and ketamine are compatible with etomidate in same syringe except vecuronium and Vit-C Different Effects ETOMIDATE In Pregnancy with Heart Dz. etomidate is drug of choice 32
- 34. Dr. Tushar Chokshi Fentanyl in TIVA • Bolus 3 μg/kg over 30 sec • Followed by 2 μg/kg/hr for 30 min • 1.5 μg/kg/hr from 31-150 min • 1 μg/kg/hr until 30 min before skin closure Remifentanyl in TIVA * 1mg/vial, 2mg/vial, 5mg/vial * Initial dose of 1 mcg/kg * TIVA Maintenance 0.25-0.5 mcg/kg/min IV * Post-Op Period 0.025-0.2 mcg/kg/min IV 34
- 35. Dr. Tushar Chokshi - FENTANYL - Bioavailability 92% (transdermal) 89% (intranasal) 65% (buccal) 54% (sublingual) 100% (intramuscular) 100% (intravenous) 55% (inhaled) Protein binding : 80–85% Metabolism : Liver(CYP3A4) Onset of action : IV within 5 minutes Elimination half-life Formula C22H28N2O Intravenous Molar mass : 336.479 g·mol−1 6 mins (T1/2 α) Melting point : 87.5 °C 1 hours (T1/2 β) Crosses BBB & Placenta 16 hours (T1/2 ɣ) Intranasal : 6.5 hrs. Transdermal : 20–27 hrs. Sublingual/buccal (single dose) : 2.6–13.5 hrs. Duration of action IV : 30–60 minutes Excretion : 75% Urine, 10% feces, 10% unchanged Routes of Administration Buccal Epidural/Spinal IM IV Nasal Nebulizer Sublingual Skin patch Oral Used as Recreational drug & also in Veterinary Anesthesia Side Effects Vomiting, Constipation, Sedation, Urinary retention, Confusion, Hallucinations Injuries related to poor coordination Symptoms of Overdose Respiratory depression, Somnolence, Stupor, Coma, Skeletal muscle flaccidity, Cold and clammy skin, Pupillary constriction, Pulmonary edema, Bradycardia, Hypotension, Airway obstruction, Atypical snoring, and Death A potent OPIOID agonist 100 times more stronger than Morphine Fentanyl invented by Paul Janssen in 1960 and approved for medical use in 1968 Most widely used synthetic opioid Hyperalgesia is common with Fentanyl Fentanyl patches for cancer pain is WHO List of Essential Medicines Mechanism of Action Fentanyl binds to opioid receptors, especially the mu opioid receptor, which are coupled to G-proteins. Activation of opioid receptors causes GTP to be exchanged for GDP on the G- proteins which in turn down regulates adenylate cyclase, reducing concentrations of cAMP. Reduced cAMP decreases cAMP dependant influx of calcium ions into the cell. The exchange of GTP for GDP results in hyperpolarization of the cell and inhibition of nerve activity Fentanyl Antagonist -Naloxone- -Nalmefene- -Naltrexone- Doses -Loading dose: IV 25-100 mcg or 1-2 mcg/kg -Maintenance dose: IV 25-50 mcg or 0.35-0.5 mcg/kg every 30 to 60 minutes -Continuous infusion: 50-200 mcg/hour (Ane.) -TIVA : 0.5 to 2 mcg/kg -NORA : 0.5 to 1 mcg/kg -Rapid sequence intubation : 1 to 3 mcg/kg -Continuous infusion : 50-100 mcg/hour (ICU) -Epidural : 0.5-1 mcg/kg/hr -Never exceed single doses of 3 mcg/kg (IM : 1-2 mcg/kg) Uses of Fentanyl 1) As analgesic with other anaesthetic drugs 2) For maintenance in all anesthesia technique (TIVA, NORA, Volatile, Regional) 3) In post operative pain relief 4) Management of chronic pain e.g. cancer 5) In Palliative Care 6) In ICU for mechanically ventilated patient 7) In Breakthrough pain 8) In Combat medicine in Military 9) Suppression of the cough reflex Available Strengths of Fentanyl (schedule II drug) IV injection : 0.05 mg(50 mcg)/ml 2ml, 10ml and 50 ml vials Transdermal Patch 12.5,25,37.5,50,62.5,75,100 mcg/hr Fentanyl Buccal Tablet : 100 mcg Intranasal Spray : 100mcg, 300mcg, 400mcg/100mcL spray Given from Neonates to Geriatric patients Extra Shots -Dose reduction is 50 % in acute renal and hepatic impairment -Do not abruptly discontinue fentanyl in patient -It can be mixed with propofol, ketamine, lidocaine, etomidate and midazolam -It also can be mixed in 5% dextrose, RL and 0.9 % normal saline for continuous infusion -No histamine release, thus preferred narcotic for asthmatic patients Extra Shots -Fentanyl is contraindicated in patients who are on MAO-Inhibitors -Rapid administration cause muscle rigidity, so always give IV injection slowly -Fentaketacaine (Fentanyl + Ketamine + Lidocaine) drip is used for postoperative analgesia -Fentanyl is also used in Neuroleptanalgesia -Recently fentanyl use extend in treatment of epilepsy -Narcotic delirium is common with fentanyl Opioid epidemic with fentanyl is very common Fentanyl is high potential for addiction
- 36. Dr. Tushar Chokshi REMIMAZOLAM New TIVA Drug Benzodiazepine with Opioid Property History 1990 – Glaxo Discovered 2008 – Payon (Japan) Acquired drug 2020 – Japan approved named Anerem 2020 – USA approved named Byfavo 2020 – China approved named Ruima 2020 – Europe/Canada/ S. Korea under approval named Aptimyda Types of Drug * Ester based Ultra Short Acting * Soft Drug * Properties of Midazolam and Renifentanyl * Sedative Anaesthetic Mechanism of Action *Acts on GABA receptors *Potentiate effect of GABA receptor which allows passage of chloride ions *And suppress and control the pain Water Soluble product Weight Average: 439.313 Monoisotopic: 438.069139 Chemical Formula C21H19BrN4O2 Protein bound: >91% (primarily to albumin) Pharmacodynamics *Enhance the effects of GABA *Sedation within 3-3.5 m *Ultra Short Acting *Not a Schedule drug *Careful in hepatic impairment *Caution in Patients of abuse or dependence Pharmacokinetics * Half Life – 37 to 53 min * Distribution Half-Life 0.5 to 2 Min Clearance - 54 to 75 L/Hr * Excretion – 80 % as inactive metabolites In renal failure no change in drug pharmacokinetics * Age, Sex, Race, weight has no effect on drug Strength * Single-patient-use vial for IV * Each glass, injection contains 20 mg white to off-white lyophilized powder, equivalent to 27.2 mg Remimazolam Besylate ready for reconstitution * Storage 20°C to 25°C * Reconstituted Remimazolam can be stored in the vial for up to 8 hours under controlled room temperature at 20°C to 25°C * Protect vials from light * Discard unused portion. * Contains 2.5 mg/ml after adding 8.2 ml of NaCl Compatible with * 0.9% NaCl Inj * 5% Dextrose Inj * 20% Dextrose Inj * 5% & 0.45% DNS * Ringer’s Solution * Do not mix with other drugs or fluids Preparation of Drug * Strict aseptic technique * Not contain preservative * Prepared immediately before use * To reconstitute, add 8.2 mL sterile 0.9% NaCl Injection which contains 2.5 mg/ml of drug Indication * Single dose for premedication * Bolus dose followed by Supplemental dose for Sedation * Intravenous anesthetic with opioids as a part of TIVA • Intensive care unit sedation • In short procedure < 30 min Contraindication * Remimazolam contains dextran 40 can cause hypersensitivity reactions * History of severe hypersensitivity reaction to dextran 40 * Avoid in clinically notable hypoxia, bradycardia, and hypotension * Oral Bioavailability is zero Overdose ( Rx - Flumazenil ) * CNS depression with drowsiness * Confusion and lethargy * Progression to ataxia * Respiratory depression * Hypotension * Abuse and Dependence Adverse Reactions * Hypotension (33-58%) * Hypertension (20-42%) *Diastolic HT(10-25%) Systolic HT(6-22%) * Hypoxia (22%), Bradycardia (3-11%) * Respiratory Acidosis (19%) * Increased RR(14%), Nausea, Headache Dose * Induction 5 mg IV over 1 min * Maintenance 2.5 mg over 15 seconds * Half dose in ASA 3 & 4 * Ideal Dose 0.075 mg/kg * Intra Nasal 0.075 mg/kg Specific Populations of Patient * Pregnancy cross the placenta and may produce respiratory depression and sedation in neonates * Lactation: discard breast milk for 5 hours after treatment with Remimazolam to avoid Neonatal Sedation: * Pediatric : Remimazolam should not be used in patients less than 18 years of age * Geriatric Use: may cause confusion and over-sedation in the elderly; elderly patients generally should be observed closely * Severe Hepatic Impairment: carefully titrated and reduced doses indicated * Renal Impairment: Not altered renal failure Pharma Co. Produced * Acacia Pharma (USA) * Mundipharma (Japan) * Hana Pharm (S. Korea and Southeast Asia * R Pharma (Russia, North Africa and Turkey) *Humanwel Pharma(China) Price of Remimazolam (20 mg one bulb) 25 Dollars in USA 1800 Rs in India Advantages Over Midazolam * Faster acting * Shorter lasting * Faster recovery * Predictable recovery * Conscious sedation * Remimazolam TCI pumps are under development stage * Called as “Soft-Drug” because of self metabolizing and organ independent properties Most Ideal Sedative Drug 36
- 37. Dr. Tushar Chokshi Adjuvant TIVA Drugs 37
- 38. Dr. Tushar Chokshi Midazolam • 0.05 mg/kg • Co-administration of midazolam in TIVA reduce the induction dose and the total dose of any other anaesthetic drug • Total dose: < 10 mg 38
- 39. Dr. Tushar Chokshi MIDAZOLAM Pharmacokinetics Bioavailability : By IV 100% , mouth 40%, IM 90%, Nasal 78% and Buccal 90% Protein binding : 97% Onset of action : Within 5 min (IV), 15 min (IM), 20 min (oral), 10 min (Bucal) Elimination half-life : 1.5 – 2.5 hours Duration of action : 1 to 6 hrs Excretion : Kidney Metabolism : Hepatic Hydroxylation by (CYP) 3A4 enzyme system Mechanism of Action Midazolam binds to the GABA receptor but does not displace GABA; rather, it enhances the affinity of GABA for its receptor site on the same receptor complex. The pharmacodynamic consequences of benzodiazepine agonist actions include antianxiety effects, sedation, and reduction of seizure activity Patented in 1974 medical use in 1982 Benzodiazepine class of drug Chemical name is C18H13ClFN3 Available as a generic medication Most commonly used benzodiazepine in anesthetic medicine It is shorter lasting, more potent, and causes less pain at the injection site In 2018 Midazolam approved as a "truth serum“ "Medication Side Effects Apnea / Bradypnea / Myoclonic jerks Variable blood pressure readings Drowsiness/Headache/Hiccups Nausea/Vomiting/Confusion Overdose It is medical Emergency Cautious with elderly patients Increase with CNS depressants, alcohol, opioids, or tricyclic antidepressants Antidote is Flumazenil (0.01 mg/kg IV) Indications For preoperative sedation/anxiolysis/amnesia In Non Operating Room Anesthesia (NORA) procedure An adjuvant to TIVA and OFA IV for induction of general anesthesia Continuous IV infusion for sedation of intubated and mechanically ventilated patients in ICU As oral/nasal/rectal premedication in pediatric patients For the acute management of seizures and schizophrenia In palliative care Caution to use In Geriatric and Paediatric patients During pregnancy and lactation In alcohol- or other drug-dependent individuals Those with comorbid psychiatric disorders In critically ill patients In hepatic and renal impairment Hypersensitivity Dose Schedules Available as injection, Syrup, Tablet & Buccal form IV/IM inj available as 1 mg/ml, 5 mg/ml & Syrup 2 mg/ml Oral pediatric dose : 0.25 to 0.5 mg/kg For Sedation : 0.01 to 0.05 mg/kg IV IM: 0.02 to 0.05 mg/kg IM,Rectal o.4 mg/kg Maintenance dose: 0.05 to 0.1 mg/kg via IV infusion per hour For GA : 0.25 to 0.35 mg/kg IV Nasal : 5 mg (1 spray) in 1 nostril Geriatric : 0.01 to 0.02 mg/kg IV ICU patients : 0.03 mg/kh/hr As a versatile drug, it is used for the management of palliative sedation and terminal restlessness in Ca It is more potent and has a shorter duration of action than diazepam, and replaced the diazepam Midazolam nasal spray is the first and only FDA- approved nasal option for treating seizure clusters Midazolam is also commonly used as a pre- anesthetic agent to provide sedation and muscle relaxation in Veterinary Anaesthesia Given by Oral, IV, IM, Nasal, Buccal and Rectal route Midazolam, at a concentration of 0.5 mg/mL, is compatible with 5% dextrose in water and 0.9% sodium chloride for up to 24 hours and with lactated Ringer's solution for up to 4 hours Compatible with Propofol, Ketamine, Etomidate, Dexmedetomidine, Fentanyl and Remifentanyl Midazolam provides no pain relief 39
- 40. Dr. Tushar Chokshi Magnesium Sulphate • As an analgesic adjunct • Useful in patients receiving total intravenous analgesia (TIVA) • Reduce propofol, Dex, atracurium and postoperative narcotic consumption • Improves the quality of postoperative analgesia during TIVA • Bolus dose is 30-50 mg/kg with other anesthetic agents and maintenance dose is 6- 10 mg/kg/hr as continuous infusion • Very cost effective for TIVA Available as 2 ml amp with 500 mg/ml and total 1 gm 40
- 42. Dr. Tushar Chokshi In spinal Anesthesia Dose : 50 -100 mg Old Wine in New Bottle Best Adjuvant in TIVA Intravenous Oxygen for Anaesthesiologist OMg OMg As Anesthesia Adjuvant Dose : 30-50 mg/kg Direct depressant on myocardial and vascular smooth muscles Anti-arrhythmic Reduces systolic blood pressure Decrease pulmonary vascular resistance Bronchodilator Reduce excitability of nerves As an Anticonvulsant Reverse the cerebral vasospasm Reduces the release of acetylcholine at NMJ Terminates muscular contraction Causing skeletal muscles relaxation (Versatile Drug) Friend Philosopher Guide For Anesthesiologist Potassium levels must be normal Extreme caution in patients with myasthenia gravis or other neuromuscular disease In renal impairment In digitalized patients Monitor renal function, blood pressure, respiratory rate, and deep tendon reflex In Local Anesthetic Block Dose : 50 – 250 mg Pre-Emptive Analgesic Analgesic effect of MgSO4 is due to inhibition of calcium channels and NMDA receptors Reduce the dose requirement for opioids, anaesthetics and muscle relaxants and part of MMA Both in hypo and hyper Magnesemia Hyperventilated patients Avoid in Geriatric and Pediatric patients as far as possible In electrolyte disturbance Avoid excessive use of volatile agents with MgSO4 (500 mg /ml) BURP Antidote for Magnesium is Calcium 42
- 43. Dr. Tushar Chokshi Dexamethasone • Dexamethasone is used widely in TIVA as an adjuvant • As anti-inflammatory agent, prevents and treats post-operative nausea and vomiting (PONV), suppress inflammation, good analgesic agent • Provides a sense of well-being • Good quality of recovery and early discharge in patients from TIVA anaesthesia • Single prophylactic dose of dexamethasone 8 mg can be given irrespective of sex, disease or ASA risk 43
- 44. Dr. Tushar Chokshi Universal Weapon For Anesthesiologist Anti-Emetic and Anti-Nauseatic Anti-Inflammatory Analgesic Effect Anti Shivering Increase Quality of Recovery No effect on sepsis and sugar in single dose 44
- 45. Dr. Tushar Chokshi DEXAMETHASONE Universal Friend Anti Nauseatic & Anti Emetic Early Discharge from Anaesthesia Anti Inflammatory Weak anti pyretic effect Anti Edema drug Anti Shivering Systemic Analgesic Effect Increase Quality of Recovery Synthetic Glucocorticoids with minimal mineralocorticoid activity Most potent anti inflammatory than Hydrocortisone and prednisolone Biological half-life is 3 hours Metabolism in liver with inactive metabolites Renal excretion upto 65% in urine within 24 hours Readily available Price is very cheap Most ideal perioperative agent Superior to ondensetron to reduce PONV Reduce opioid Consumption Decrease Analgesic effect upto 24 hours Always to be given prior to surgery Best TIVA and OFA adjuvant Great psychological effect Prevents any allergic reaction Dose Schedule PONV – 0.1 mg/kg (IV) Anti Inflammatory – 0.2 mg/kg(IV) Analgesic – 0.1 mg/kg(IV) Epidural -- 8 to 10 mg Blocks – 0.1 mg/kg S/A - 8 mg Mechanism of Actions Depletion of γ-aminobutyric acid (GABA) stores and reduction of blood brain barrier to emetogenic toxins, Inhibition of central prostaglandins and serotonin Membrane stabilizing effect on nerves and on spinal cord Dexona IN DM 4 mg is ideal dose 8 -10 mg dose Increase around 25 mg/dl glucose postop upto 24 hrs Dexona in Sepsis Does not increase any risk of wound infection with or without DM in any surgical procedure Acute Side Effect Flushing Perineal Itching Dexona Is the only adjuvant in anesthesia given irrespective of age, sex, disease or ASA status Safe in Onco Anesthesia Avoid in Psychiatric patients Be careful in Immuno compromised patients Improves Cognitive function In Elderly 8 8 8 8 8 8 8 8 45
- 46. Dr. Tushar Chokshi Best Companion of Anesthesiologist Lidocaine Analgesic & Anti Hyperalgesic Anti Inflammatory Reduced opioid analgesic consumption Anti Arrhythmic Improvements in patient’s outcomes Decrease Aerosol and Droplets during Extubation 46
- 47. Dr. Tushar Chokshi Intravenous Lidocaine (Magic Drug) Best Adjuvant in TIVA Lidocaine is metabolized in the liver and excreted by the kidneys Permanent member of Multi Model Anaesthesia & Analgesia Analgesic Anti Arrhythmic Anti Cancer drug Anti Hyperalgesic Anti Inflammatory Reduces the release of cytokines Improvements in patient’s outcomes Reduced opioid analgesic consumption Reduce Volatile anesthetic consumption Decrease Laryngospasm and Laryngeal Edema Decrease Aerosol and Droplets during Extubation Class-1b Antiarrhythmic Amide Local Anesthetic Most beneficial In painful Propofol/Etomidate Inj. Both in Acute and Chronic pain Abdominal Surgery Neuro surgery TIVA and OFA Onco surgery ENT surgery In ERAS Most ideal drug to blunt airway reflexes and sympathetic responses to laryngoscopy and tracheal intubation Mechanism of Action Blocks sodium ion channels on the cell membranes and stabilizes the membrane In neural tissues, lidocaine inhibits the generation, transmission and propagation of neural impulses At the level of the spinal reflex, it blocks the afferent and/or efferent parts of the reflex arc The pharmacological effect of IV lidocaine involves multiple pathways (peripheral and central) and mechanisms (direct and indirect) for pain relief Dose Schedule A bolus of 1–2 mg/kg followed by an infusion of 1–2 mg/kg/h with IBW From Pediatric to Geriatric Do not exceed a maximum dose of 100 mg bolus or 100 mg/h The target plasma concentration for therapeutic effect is between 2.5 and 3.5 μg/ml CNS toxicity occurs in > 5 μg/ml CVS toxicity occurs in > 10 μg/ml Post Operative IV Lidocaine Use of lidocaine for up to 24 h has significant decrease in pain Reduced analgesic requirements A faster return of GI function An overall reduction in side effects Maximum post op infusion can be given upto 3 to 5 days till the bowel function returns normal and pain is well Controlled Multi Para monitoring is must during post op IV lidocaine Practical Consideration The concomitant use of IV lidocaine with another regional anaesthesia technique (e.g., epidural, TAP block) requires careful consideration and is probably best avoided because of possible local anaesthetic toxicity IV lidocaine is a component of every laparoscopic procedure, irrespective of its duration, invasiveness and desired outcomes IV lidocaine is Useful to relieve PDPH IV lidocaine always, to ordered by Anesthesiologists In High-Risk Patients IV Lidocaine dose must be reduced Invention 1943 First Marketed 1949 47
- 48. Dr. Tushar Chokshi Paracetamol • Preemptive analgesic • Has got opioid sparing effect • Loading dose is 30 mg/kg and maximum not to exceed 2 gm • Very innocent drug in TIVA and can be repeated at every 6 to 12 hours interval in dose of 1000 mg • Excellent adjuvant in Pediatric TIVA Diclofenac Sodium • Powerful NSAID in TIVA with analgesia and anti- inflammatory action • Best is given in single dose of 1.5 mg/Kg IV slowly and maximum is 150 mg • Use aqueous solution only • Caution with renal, hepatic, pulmonary and heart failure patients Always give both drugs before surgical incision to inhibit prostaglandin receptors 48
- 49. Dr. Tushar Chokshi It is an effective analgesic, especially when administered IV, useful in a broad range of clinical conditions. Also known as Acetaminophen Synthesized in 1878 by Morse, medical usage in 1883 & available without prescription since 1959 Nonsteroidal anti-inflammatory group drug Routes of administration Mouth and Buccal Rectal IV and IM Onset of action Mouth – 37 minutes Buccal – 15 minutes Rectal – 40 minutes Intravenous– 8 minutes Pharmacokinetic Protein binding : 10–25% Metabolism : Mainly liver Excretion : Urine (85–90%) Bioavailability : 63–89% Protein binding : 10–25% Elimination half life : 2–2.5 hours Formula : C8H9NO2 Molar mass : 151.165 g·mol−1 Boiling point : 420 °C Dose Schedule Infusion 10 mg/ml available 100 ml pint & 150 mg/ml amp < 10 kg : 7.5 mg/kg, maximum daily dose 1 gm 10 kg to 33 kg : 15 mg/kg, maximum daily dose 2 gm 33 kg to 50 kg : 15 mg/kg, maximum daily dose 3 gm > 50 kg without any renal/liver dz : 1 gm and maximum 4 gm > 50 kg with any renal/liver dz : 1 gm and maximum 3 gm The minimum interval between each IV administration must be at least 4 hours and no more than 4 doses to be given in 24 hours Contraindications Hypersensitivity to paracetamol In cases of severe hepatocellular insufficiency Pre-term newborn infants Indications Short term treatment mild to moderate pain Short- term treatment of fever As adjuvant in TIVA and OFA Precautions for use Chronic renal and liver disease Malnutrition Dehydration Overdose Risk of Liver injury particularly elderly subjects & young children with overdose of 7.5 g Nausea/Vomiting/Anorexia/Pallor/Abdo. Pain Storage Store below 25°C. Do not Freeze Available in 100 ml Glass Bottle and Non PVC Bag Shelf life 2 years The pharmacokinetics and the metabolism of paracetamol are not modified in elderly subjects, so, no dose adjustment is required Antidote (IV/Oral) is N-acetylcysteine (NAC) Mechanism of Action Paracetamol has a central analgesic effect that is mediated through activation of descending serotonergic pathways Its primary site of action, which may be, weak inhibition of prostaglandin (PG) synthesis or through an active metabolite influencing cannabinoid receptors Paracetamol never reduce tissue inflammation like other NSAIDs Has got opioid sparing effect Paracetamol combined with NSAIDs more effective for treating postoperative pain than either paracetamol or NSAIDs alone It is safe to use during pregnancy and when breastfeeding Paracetamol can be safely taken both with food and on an empty stomach PCM cause rare and possibly fatal skin reactions such as Stevens–Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) Extra Shots An association exists between paracetamol use and asthma so avoid in children with asthma In contrast to aspirin, paracetamol does not prevent blood from clotting (it is not an antiplatelet), thus it safely used in people who have concerns with blood coagulation Paracetamol hepatotoxicity is by far the most common cause of acute liver failure and death within days Combinations of oral paracetamol and opioid analgesics and intramuscular paracetamol would be avoided It is weak analgesic and mainly antipyretic drug Some studies have found an association between paracetamol and a slight increase in kidney cancer, but no effect on bladder cancer risk It is also available in liquid suspension and effervescent forms It is the firs t Over The Counter (OTC) drug in the world Diclofenac Sodium and Paracetamol combination is most widely used for postoperative analgesia, but thumb rule is that they should be given before any surgical incision There are no haemodynemic changes with paracetamol but repeated use causes hypertension No sedative effect Pet Name PCM During IV regional anaesthesia, adding PCM to the injected lidocaine was shown to improve the overall quality of the block & onset is sooner
- 50. Dr. Tushar Chokshi DICLOFENAC SODIUM Introduced By Ciba-Geigy in 1965 Nonsteroidal anti-inflammatory drug Available worldwide Generic Medication Available as both a sodium and a potassium salt Given by Mouth, Rectally, IM, IV injection and Topical Skin Gel/Spray Pharmacokinetic Formula C14H11Cl2NO2 Protein binding More than 99% Metabolism Liver, oxidative, primarily by CYP2C9 Onset of action Within 4 hours Topical,30 min Oral, 15 minutes IM, 5 minutes IV and 30 minutes Rectal Elimination half-life 1.2–2 hr Excretion 40% bile duct and 60% urine Molar mass 296.15 g·mol−1 Mechanism of action The primary mechanism responsible for its anti- inflammatory, antipyretic, and analgesic action is thought to be inhibition of prostaglandin synthesis by inhibition of the transiently expressed prostaglandin- endoperoxide synthase-2 (PGES-2) also known as cycloxygenase-2 (COX-2). Blockage of voltage-dependent sodium channels Blockage of acid-sensing ion channels It also appears to exhibit bacteriostatic activity by inhibiting bacterial DNA synthesis Avoid use of multidose bulb/vial Positive allosteric modulation of KCNQ- and BK-potassium channels It inhibits the lipoxygenase pathways, thus reducing formation of the leukotrienes It also may inhibit phospholipase A2 as part of its mechanism of action These additional actions may explain its high potency – it is the most potent NSAID on a broad basis Contraindications Hypersensitivity against diclofenac History of allergic reactions (COPD, bronchospasm, shock, rhinitis, urticaria) Active stomach and/or duodenal ulceration or GI bleeding Severe congestive heart failure Severe liver insufficiency Severe chronic kidney disease Pre-existing hepatic porphyria Avoid during dengue fever Patients with fluid retention In worsening of pre-existing hypertension Inflammatory bowel disease such as Crohn's disease or ulcerative colitis Serious skin adverse events e.g. exfoliative dermatitis, Stevens–Johnson syndrome, toxic epidermal necrolysis Powerful NSAID in TIVA/OFA with analgesia and anti-inflammatory action Use aqueous solution only Best is given in single dose of 1.5 mg/kg IV slowly and maximum is 150 mg It is opioid sparing drug Always give before surgical incision to inhibit prostaglandin receptors, which control the haemodynamic response to surgical stimulation Diclo should not be mixed with any drug except paracetamol in same syringe Given with any IV Infusion Always dilute diclo with DW and give slowly to avoid injection pain Dose Oral 50 mg 2 or 3 times a day Extended-release tablets 100 mg once a day Potassium immediate-release tablets 50 mg orally 2 or 3 times a day Sodium enteric-coated tablets 75 mg orally 2 times a day IV/IM 1 to 1.5 mg/kg, repeat after 8 hours Rectally 1 to 1.5 mg/kg ( Paediatric patients) Diclo is better than paracetamol to control post operative fever & pain In anaesthesia practice Diclo Is used as an adjuvant for perioperative acute pain management Diclofenac is an effective analgesic for acute pain in children as part of the analgesic regime in the peri operative period with dose range from 0.5 to 2.5 mg/kg Infusion line pain or irritation to vein is very common during IV Diclo, so better prefer large venous line Major side effects of diclo are 1) abdominal or stomach pain, cramping, or burning 2) bloody or black, tarry stools 3) bloody urine and decreased frequency or amount of urine 4) heartburn or indigestion 5) diarrhea 6) increased thirst and loss of appetite 7) vomiting of blood or material that looks like coffee grounds 7) very rare anaphylactic or anaphylactoid reaction Some time single dose or overdose of Diclo may cause acute renal failure As far as avoid diclo in geriatric age group of patients ( paracetamol is preferred )
- 51. Dr. Tushar Chokshi (Opioid sparing adjunct) (Gives central analgesia) 51
- 52. Dr. Tushar Chokshi ESMOLOL Emergency friend of Anaesthesiologist Cardioselective beta1 receptor blocker Shortest acting beta blocker Class II Antiarrhythmic Safely given in broncho- spastic and vascular dis. Gives central analgesia Opioid sparing adjuvant in OFA and TIVA Mechanism of Action Esmolol decreases the force and rate of heart contractions by blocking beta-adrenergic receptors of the sympathetic nervous system, which are found in the heart and other organs of the body Esmolol prevents the action of two naturally occurring substances: epinephrine and norepinephrine No significant intrinsic sympathomimetic or membrane stabilizing activity at therapeutic dosages Dosages forms and Strengths Infusion bags 2 g/100 ml, 2.5 g/250 ml, 5 g/500 ml Injectable solution 10 mg/ml and 20 mg/ml Compatible with all common solvents Incompatible with NaHCO3 Never infuse in small veins or by butterfly Never stop abruptly due to withdrawal effect Side Effects 10 % or more Hypotension asymptomatic ( 25%) Hypotension symptomatic (12%) Bradycardia (15 %) 1 – 10 % Injection site pain (8%) Agitation (7%) Dizziness(3%) 1 % or less Chest pain Anxiety/Depression Dry Mouth/Dyspepsia Redness of the face and neck Headache Pharmacokinetic Bioavailability 90 % Protein binding 55-60% Metabolism Erythrocytic (in blood by hydrolysis of its methyl ester) Elimination half-life 9 minutes Distribution half life 2 minutes Duration of action 10-30 minutes Excretion Kidney (73-78%) Vd 3.4 liter/kg Storage at room temperature Safely given in pediatric Patients ( > 2 Years) Careful in Pregnancy Uses To terminate supra- ventricular tachycardia In episodic atrial fibrillation or flutter Arrhythmia during perioperative period To reduce HR and BP during and after cardiac surgery In early treatment of myocardial infarction In blunting the haemodynemic response to laryngoscopy and intubation To reduce intra and post operative hypotension Brady is less Intraoperative Tachycardia and Hypertension Immediate control 1 mg/kg over 30 sec then 0.15-0.3 mg/kg/min infusion Postoperative control 0.5 mg/kg iv for 1 min then 0.1 mg/kg/min infusion If not control then repeat bolus doses For supraventricular tachycardia 0.5 mg/kg over 1 min then 0.05 mg/kg/min infusion Hypo Is more PONV is less Best adjuvant in Ane Contraindication Sinus bradycardia, Sick sinus syndrome AV heart block, Heart failure Pulmonary hypertension Hypersensitivity
- 53. Dr. Tushar Chokshi TIVA Drug Combinations 53
- 54. Dr. Tushar Chokshi 54 What to understand before mixing any drugs for anesthesia
- 55. Dr. Tushar Chokshi Anesthesia Triangle The concept of the anesthesia triangle works with Hypnosis, Analgesia, Relaxation – and their interactions Any medications entering this prism may result in different interactions: Pharmaceutical, Pharmacokinetics, Pharmacodynamics, and Thermodynamics by combo A larger number of incoming drugs leads to increased complexity and more interactions So, the rule is not mix more than three drugs at time 55 Anesthesia Triangle • Hypnosis • Analgesia • Relaxation Hypnosis Analgesia Relaxation Anesthesia Triangle
- 56. Dr. Tushar Chokshi Red Not compatible Green Compatible Yellow Non-conclusive The hidden world of drug interactions in anesthesia Colombian Journal of Anesthesiology Volume 45, Issue 3, July–September 2017, Pages 216-223 Alberto Tafur Betancourt Conclusion Drug interactions are the corner stone of the anesthesia triangle and being aware of those interactions may contribute to safe anesthesia White Not tested
- 57. Dr. Tushar Chokshi TIVA KINGDOM Anaesthesiologist Fentanyl Remifentanyl MgSO4 King Commanders Oxygen Soldier Here King will decide their military in battle of anesthesia whom to send in combination Prince is most common warrior and goes in every battle of anesthesia Prince with one or two supreme commander are the best military of King In absence of prince two supreme commanders go to win small battles
- 59. Dr. Tushar Chokshi Ketofol • First established TIVA combination in 1990 • Physically compatible chemically stable 1:1 mixture in capped syringe 3 hrs at room temperature with exposure to light • No significant change in pH up to 3 hrs • No separation, cracking, color change, gas formation • Widely used by all anesthesiologist across globe Ketodex/Dexket • Ketamine 1mg/kg and Dex 1 mcg /kg • Useful in Pediatric patients Ketomed • Ketamine 1mg/kg and Midazolam 0.1 mcg /kg • Useful in outside OT procedures 59
- 60. Dr. Tushar Chokshi KPD TIVA (Ketamine, Propofol and Dex) Mixture in 1:1:1 Dose for TIVA Combination of all these drugs permit lower dose of each individual agent for TIVA and reducing their adverse hemodynamic and respiratory effects which is very safe and important for patient and anesthesiologist The advantage is low dose of each agent as compared to full dose Excellent analgesia and anesthesia dose of individual agents airway complications Stable haemodynamics Rapid recovery 60 Used as Bolus, Maintenance and Short case < 30 minutes
- 61. Dr. Tushar Chokshi PROPOFOL & FENTANYL Combination of Propofol (1% & 2%) with Fentanyl (10 & 50 mcg/ml) showed no significant degradation of emulsion within 20 hrs Propofol dose reduction by 50% 61
- 62. Dr. Tushar Chokshi RP TIVA (Remifentanyl and Propofol) Can be mixed in polypropylene syringes and used for up to 36 hours- remifentanil concentration is 50 mcg/ml (1mg in 20 ml propofol) Color and clarity good with pH stable at 3.9 - 4 Very short acting Adequate analgesia, satisfactory hemodynamic, rapid recovery, shorter PACU stay, excellent patient acceptance Ideal agents for TCI model Synergism- Propofol dose reduction by 50% Most widely used TIVA combination with TCI in the world 62
- 64. Dr. Tushar Chokshi give TIVA • Either with a single drug or with a combination of drugs • By Single Syringe Technique with mixture of drugs or with only one drug • Continuous IV infusion through drips • With Syringe infusion pumps • With TCI ( Target Controlled Infusions) machines • Automated drug delivery through Closed Loop Systems 64
- 65. Dr. Tushar Chokshi Single Syringe TIVA (SS TIVA) 1) No additional investment for TCI or Closed Loop Systems and no need for expertise in it. 2) Simple syringe or pump can be made use of. 3) Only one syringe is used, with the advantage of dose titration at a single level & fixed dose mixtures 4) Short procedures can be managed with intermittent boluses, without a syringe pump. 5) It can be practiced in low dependent set ups, and outside the operating rooms Explores the feasibility and conduct of combining intravenous agents in a single syringe technique to provide balanced anesthesia 65
- 66. Dr. Tushar Chokshi Manually Controlled Infusion (MCI) Manual dosing of anaesthetic agents during TIVA With fixed infusion rate With syringes or with IV drips 66
- 68. Dr. Tushar Chokshi Target Controlled Infusion (TCI) A target controlled infusion is an infusion controlled to achieve a pre set drug concentration in the plasma or the effect site Key components of a TCI infusion User interface to enter details and target blood concentration Software with pharmacokinetic model, validated for specific drug to control infusion rate Communication between ‘control unit’ and pump hardware 68
- 69. Dr. Tushar Chokshi Single Syringe TCI Double Syringe TCI Three Syringe TCI 69
- 70. Dr. Tushar Chokshi John Baird Iain Glen He is Father of Modern TIVA Technique He has developed first established TCI system ‘Diprifusor’ for Propofol TIVA First time in 1996 70
- 71. Dr. Tushar Chokshi Clinical benefits of TCI ( >2000 publications) * More predictable onset of anaesthetic effect * Higher stability during maintenance * More predictable offset of anaesthetic effect * Short time to recovery * Low incidence of PONV * Short time to discharge Economic benefits * Saves nursing time in the recovery room * Limits the need for anti-emetic therapy * Allows patients an early return to work 71
- 72. Dr. Tushar Chokshi TCI Models Overview 72
- 73. Dr. Tushar Chokshi 73 Tushar Chokshi Infusion (TCI) Three Styles 1) KPD Infusion ( Ketamine + Propofol + Dexmedetomidine ) 0.5 mg : 0.5 mg : 0.5 mcg / kg/ hr ( In 500 ml RL ) 2) Dexmedetomidine Infusion ( In 500 ml RL ) 1 mg/ kg / hr 3) Propofol Infusion ( In 100 ml NS) 6 mg / kg / hr (As maintenance infusion during TIVA) Without TCI Machine
- 74. Dr. Tushar Chokshi Closed Loop Anaesthesia Delivery Systems or Automated Total Intra Venous Anaesthesia A closed-loop system is the ideal means of automated drug delivery • The Input – Drug delivery (etc. Propofol, Opioids) • The Output – Evoked Potential, Bispectral Index (BIS), Blood Pressure, Pulse Rate. ATIVA/CLADS 74
- 75. Dr. Tushar Chokshi D Input Output 75 Computer Drugs Delivery Vital Signs
- 76. Dr. Tushar Chokshi Closed Loop Anaesthesia Models 76
- 77. Dr. Tushar Chokshi Clinical Benefits of Closed Loop Anesthesia • Automatic delivery of anaesthetic drugs to the patient at the time of induction of anaesthesia using IV anaesthetic agents depending upon the patient’s condition or choice of anaesthetist. • Frees the anaesthetist from the repetitive task of looking at the anaesthetic depth and altering the drug delivery manually. • Frees anaesthetists hands to allow him/her for other activities while keeping a watch on the monitor. • Anaesthetist is warned of the abnormal rates of drug delivery as well as abnormal response of the patient through visual and audio warning • Fine-tuning of the drug delivery according to the requirement of the patient as well as the surgical stimulus requirement. • Safety of patient by cutting off anaesthetic drug delivery in case of severe drop in blood pressure or heart rate. • The anaesthetist to define the safety limits of blood pressure as well as heart rate and blood gas levels for not only warning the anaesthetist but also stopping delivery of the anaesthetic agents. • The anaesthetist to define the inspired and expired concentrations of anaesthetic agent beyond which the system stops delivery of anaesthetic agent. 77
- 78. Dr. Tushar Chokshi iControl-RP (Remifentanyl-Propofol) iControl-RPR (Remifentanyl-Propofol-Relaxant) • Auto Robotic TIVA CLADS • US FDA approved • Developed in Vancouver at University of British Columbia in 2015 • By Team of Dr. Ansermino(Pediatric Anesthesiologist) & Dr. Dumont(Professor of electrical and computer engineering) 78
- 79. Dr. Tushar Chokshi TIVA in Different Groups of Patient Pediatric Geriatric Obese ASA III 79
- 80. Dr. Tushar Chokshi TIVA in Pediatric Patients • Paediatric total IV anaesthesia (TIVA) can facilitate surgery, reduce airway responsiveness, and minimize complications such as postoperative nausea and vomiting and emergence agitation • Manual infusions remain an important option in clinical practice due to variability of dose regime • Kataria and Paedfusor TCI models are used. The Kataria model used in children aged 3-16 yr and weighing 15- 61 kg, and the Paedfusor in children aged 1-16 yr and weighing 5–61 kg • Propofol, Ketamine, Remifentanil and dexmedetomidine play important role in TIVA • For obese children use the total body weight (TBW) to calculate the dose needed for infusion As far as avoid TIVA in Neonates 80
- 81. Dr. Tushar Chokshi TIVA in Geriatric Patients • Compared with inhalation anaesthesia, TIVA is more suitable as it has less observable effects on cognitive function in elderly patients after surgery • Comparing with TIVA, inhalational anaesthetics may augment complications related with reduced lung blood flow and circulatory depression. Inhalational anaesthetic agents may further reduce cardiac output and cause potentially lethal increase in alveolar concentration • Always start with a low concentration/infusion rate and slowly work upwards. Go Low, Go Slow and Always Follow • Most important is to avoid hypotension. Consider intravenous fluids and vasopressors when appropriate • Multi Para monitoring and Oxygen is must during TIVA in geriatric patients 81
- 82. Dr. Tushar Chokshi TIVA in Obese Patients • TIVA is an excellent method of administering general anaesthesia to obese patients • The recommended drug dose in obese patients always lower than non-obese patients, the actual blood concentration is higher than the calculated target dose of drugs. • The “no-relaxant” technique (for intubation) is not advisable for obese patients and Suxamethonium for intubation in TIVA is ideal choice • In Obese patient always secure airway to avoid respiratory depression with nasal or oral airways • Multi Para monitoring and Oxygen is must during TIVA in Obese patients 82
- 83. Dr. Tushar Chokshi TIVA in ASA III Patients • TIVA can be given to seriously ill patients in whom their systemic disease is not a threat to their life (ASA III) • There are no specific protocols for TIVA in ASA III patients but dose of TIVA of elderly patients can be adopted, require a lower concentration to produce anaesthesia • Multi Para monitoring and Oxygen is must during TIVA in these patients • Choose the most appropriate TIVA drugs according to the patient’s physical condition:- # Whether the patient is elderly or young # Whether the patient is obese or non-obese 83
- 84. Dr. Tushar Chokshi Surgical Procedures under TIVA in COVID Pandemic • From OT to Outside OT • From Pediatric to Geriatric patients • From any Surgical to Medical Specialty 84
- 85. Dr. Tushar Chokshi TIVA • All anesthesia drugs, Airway Equipments, Oxygen and Multipara Monitor are must before giving TIVA • Ensure no leakages from cannula and patient’s IV cannula is always visible during the surgery (if possible) • Syringes should be labelled with the drug name, date and concentration • Infusion lines should be checked every 15 minutes during surgery • The infusion set through which TIVA is delivered should have a Luer- lock connector at each end • If BIS is used, check placement before and after surgical draping • At end of case, ensure all tubing/IV cannulae which had TIVA drugs by any method are flushed to prevent inadvertent boluses in the ward 85
- 86. Dr. Tushar Chokshi TIVA Monitoring • Anesthesiologist • Loss of response to shaking and shouting • Loss of hemodynamic response or limb movement with vigorous jaw thrusting • Absence of tachycardia or even bradycardia with laryngoscopy and intubation • Multipara monitoring • Bispectral Index Monitor • Evoked Potentials • pEEG monitor is recommended when a neuromuscular blocking drug is used with TIVA Visual Machine 86
- 87. Dr. Tushar Chokshi TIVA TIVA has become more Popular, Practical and Possible due to two main reasons – First The advance knowledge of pharmacokinetic and pharmacodynamic properties of drugs such as Propofol, Ketamine, Dexmedetomidine and newer short-acting opioids, making them suitable for intravenous administration Second New concepts in pharmacokinetic modeling coupled with advances in the technology of infusion pumps which allow the use of algorithms such as Syringe Infusion Pumps, Target Controlled Infusion (TCI) & Closed Loop System Propofol with Remifentanil seems to be the dominating TIVA technique all over world, delivered either by conventional pumps or by target control systems or by close loop systems 87
- 88. Dr. Tushar Chokshi TIVA APPS 88
- 89. Dr. Tushar Chokshi Do TIVA with your Smartphone and volumetric pumps, in a pharmacokinetic manner 89
- 91. Dr. Tushar Chokshi The easiest and best drug infusion calculator for anaesthesia or anywhere else 91
- 94. Dr. Tushar Chokshi So TIVA in Fact • Patient Friendly • Surgeon Friendly • Anaesthesiologist Friendly • Economically Friendly • Environmentally Friendly • Productivity Friendly TIVA will be a norm in Future Practice This is how it is used 94
- 95. Dr. Tushar Chokshi Future Auto TIVA through Artificial Intelligence(AI) with help of TCI and BIS Dexmedetomidine TCI model Hannivoort and Dyck will be launched in 2021 Like Vaporizers, the Syringe Pumps and TCI systems will be integrated into the Anesthesia Work Station TIVA will be a Norm and New Normal TIVA will rule in all anaesthesia techniques by 2030 95
- 96. Dr. Tushar Chokshi ALL-IN-ONE TCI and CLA 96
- 97. Dr. Tushar Chokshi Secret Project for long TCI TIVA Asena P&P 97
- 98. Dr. Tushar Chokshi Instead of This complex Anesthesia machines with Monitors 98
- 99. Dr. Tushar Chokshi AI Monitor In 2030 Switch On & Switch Off Anaesthesia Machine Tusha Future TIVA Anaesthesia Work Station
- 100. Dr. Tushar Chokshi Newer Drugs in TIVA • Remimazolam ( Narcotic + Benzodiazepine ) 2020 • Suggamdex ( Reversal Agent) 2015 • Hyptiva (Anesthetic + Narcotic) combines the pharmacodynamics of Propofol with the pharmacokinetics of Remifentanil • Duzitol (Anesthetic + Narcotic + Muscle Relaxant) combines hypnosis, amnesia, analgesia, muscle relaxation and aphrodisiac 100
- 101. Dr. Tushar Chokshi Take Home Message Total Intravenous anaesthesia is viable and safe alternative to the Inhaltion Anaesthesia , with lots of advantages over the latter The newer intravenous hypnotics and analgesic agents with favourable pharmacokinetic properties have made TIVA more popular in a wide array of varying clinical scenarios and anaesthetic demands Manual Controlled Infusions using regular syringe pump can be used to deliver pre- calculated doses TCI pumps and advance monitors make administration of TIVA easy and precise & STEP IN YOUR COMFORT ZONE with TIVA for Safe Anaesthesia Safe Surgery Safe patient Safe Yourself 101
- 102. Dr. Tushar Chokshi Patient wants more than Gas Anesthesia
- 103. Dr. Tushar Chokshi 103 I I won’t use TIVA I can’t use TIVA I won’t to use TIVA How do I use TIVA I will try to use TIVA I can use TIVA I will use TIVA Yes, I have used TI
- 104. Dr. Tushar Chokshi GROUP 104
- 105. Dr. Tushar Chokshi Different TIVA Societies in the World www.eurosiva.eu www.worldsiva.org https://siva.ac.uk 105
