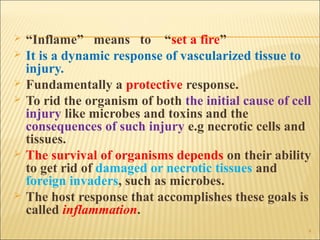
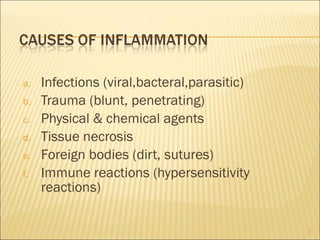
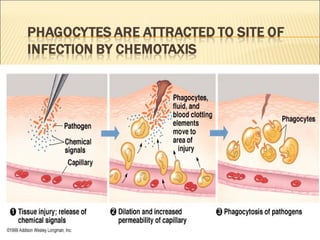
1. The document discusses inflammation, describing it as the body's protective response to injury or infection that helps rid the body of damaging stimuli and initiate repair of tissues.
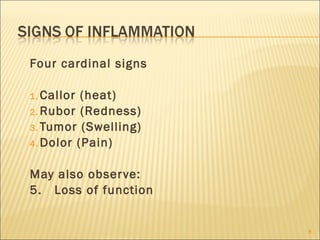
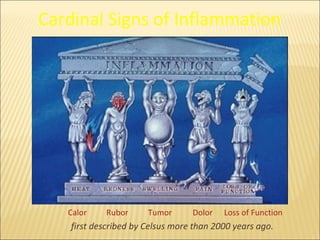
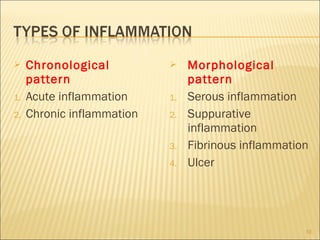
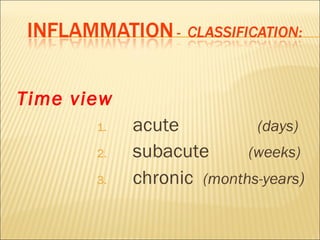
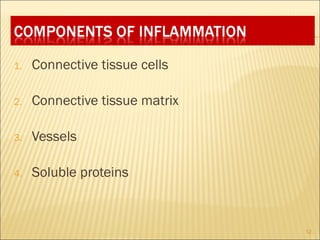
2. It notes the four cardinal signs of inflammation as heat, redness, swelling, and pain, and explains the causes, types, and components of the inflammatory response.
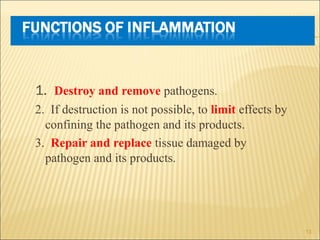
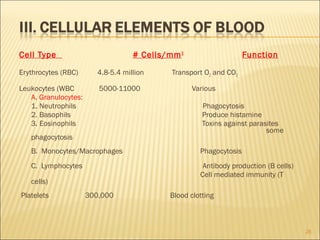
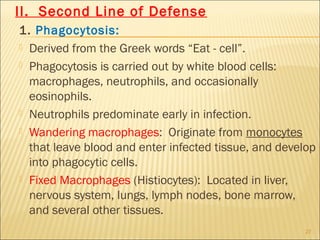
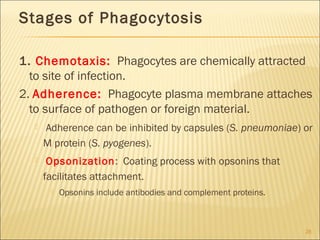
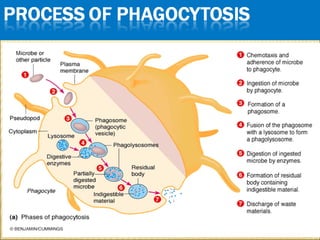
3. The summary outlines the functions of inflammation in destroying pathogens, limiting their spread, and repairing damaged tissues, as well as the roles of plasma proteins, leukocytes, and tissue phagocytes in mounting an inflammatory response.