Avoiding and Managing Complications During Gynaecological Surgery
- 1. Avoiding and managing complications with gynaecological surgery Joanne Morrison Alexander Swanton Ian Z MacKenzie Abstract All surgery involves a delicate balance of risk management, from the benefits and disadvantages of when a surgical option is appropriate, to the immediate post-operative care. Recognizing areas of high risk and understanding how these may be minimized, is central to the practice of safe surgery. All surgeons may encounter complications at some point, but recognizing when these occur and the most appropriate initial management is essential to prevent or minimize immediate and long-term complications. In addition, as some complications will involve areas in which the surgeon has relatively little expertise, it is important to acknowledge that limitation and enlist help from an appropriate specialist at an early stage. This review focuses on general advice on avoiding and managing complications in gynaecological surgery, excluding radical cancer surgery. Keywords bladder injuries; bowel injuries; laparoscopy complications; ureteric damage; uterine perforation; vascular damage Introduction No surgery is without risk and safe surgery aims to recognize and minimize these risks, whether due to patient or surgical factors. The previous version of this review concentrated on complica- tions encountered with specific procedures (see further reading). In this review, we will concentrate on general surgical principles, with a greater emphasis on endoscopic surgery. Factors which predispose to complications during or after surgery will be considered, followed by pre-operative strategies to identify these factors, with recommendations for reducing their occurrence. Techniques to minimize intra-operative complications will then be discussed, followed by methods for recognizing these complications during the surgery and the post- operative period. Finally strategies for managing complications will be presented. Complications may be more likely to occur with laparoscopic surgery than conventional open surgery, due to relative operator inexperience, the introduction of new instruments and more frequent use of energy sources. Electrocoagulation and laser vapourization can cause inadvertent thermal damage, which may be recognized or suspected intra-operatively, or present as delayed injuries. The incidence of complications during endo- scopic surgery is much more likely with therapeutic than diag- nostic surgery, and the complexity of the surgery significantly influences the complication rate. The likelihood of injury depends on a number of factors, and in order to minimize the chance of complications, it is important to understand which factors increase the risk and what can be done to minimize them. Pre-disposing factors Several conditions including endometriosis, cancer, disturbed coagulation, previous surgery in the operative field with subse- quent adhesion formation and obesity can complicate surgery and increase the chance of injury. Surgical competence is a major factor and complication rates decline with increasing operative practice. Appropriate training is therefore essential, but with the imposed reduction in trainees’ working hours, opportunities will diminish and inventive teaching techniques, probably using simulators, will be required to replace that void. Avoiding and preventing complications Pre-operative strategies A thorough pre-operative assessment is crucial to identify potential anaesthetic and surgical risk factors. A comprehensive history and relevant clinical examination are vital when surgery is considered. When a pre-disposing risk factor is identified, appropriate investigations should be considered (e.g. CT scan or MRI, lung function tests, ECHO cardiogram, clotting studies). Pre-operative imaging can inform counselling of the patient and planning of the procedure for the surgeon. Appropriate equip- ment and personnel can be selected in advance of the surgery. Pre- and peri-operative measures to reduce risks in susceptible cases will include intra-operative antibiotics and thrombopro- hylaxis (TEDS, low molecular weight heparin and intermittent pneumatic compression calf devices depending on level of risk). Full bowel preparation is no longer recommended although phosphate enemas will help to decompress a loaded rectum, if rectovaginal dissection is anticipated. If stoma formation is a possibility, referral to the stoma team for patient counselling and marking of potential stoma sites, is advisable. Patients with a body mass index >35 kg/m2 are at increased risk of anaes- thetic, surgical and post-operative complications and should be advised to lose weight prior to elective surgery. Serious medical co-morbidities should prompt seeking senior anaesthetic advice prior to planned surgery. Informed consent for any procedure needs to be taken care- fully by a doctor who understands the operation and the risks involved. These risks should be explained clearly to the patient, Joanne Morrison BM BCh MA MRCOG DPhil is a Macmillan Subspecialist Trainee and Clinical Lecturer in Gynaecological Oncology at the Oxford Cancer and Haematology Centre, Churchill Hospital, Oxford, UK. Conflicts of interest: none. Alexander Swanton MBBS MRCOG is a Consultant Gynaecologist at the Royal Berkshire Hospital, Reading, UK. Conflicts of interest: none. Ian Z MacKenzie FRCOG DSc is a Reader and Honorary Consultant in Obstetrics and Gynaecology at the Nuffield Department of Obstetrics and Gynaecology, John Radcliffe Hospital, Oxford, UK. Conflicts of interest: none. REVIEW OBSTETRICS, GYNAECOLOGY AND REPRODUCTIVE MEDICINE 20:3 75 Ó 2009 Elsevier Ltd. All rights reserved.
- 2. avoiding medical jargon, with careful documentation of this discussion. Confirmation of ‘right patient, right operation’, is ultimately the responsibility of the surgeon. The concept of ‘‘site and side’’ skin marking is often not applicable to gynaecological surgery, but it can be very important when dealing with vulval lesions and ovarian or tubal pathology. Ensuring the documentation is in order and that imaging studies and all necessary equipment are available, is part of good surgical practice. These checks should be formalized as part of a pre-operative check-list, which should involve surgeons, anaesthetists and theatre staff, aimed at pre- venting complications due to communication or equipment problems. Intra-operative strategies All surgeons should be familiar with the anatomy of the relevant surgical area. Basic principles are required to avoid major complications during both open and endoscopic surgery. Specific risks for open and vaginal surgery are discussed in the previous version of this review (see further reading). Patient positioning in theatre can reduce nerve damage, back and pelvic problems and pressure sores during long procedures. Steep Trendelenberg positioning is sometimes required during complex laparoscopic procedures and shoulder supports, with padding to reduce the risk of brachial plexus injuries and close anaesthetic monitoring, may be necessary. Lithotomy poles should be avoided, since these increase the risk of peroneal nerve injury compared with cushioned foot/calf support devices. Skin preparation with antiseptic (e.g. betadine or chlorhexidine) and attention to good sterile techniques will help to reduce the risk of wound infection. Before most gynaecological procedures, the bladder should be emptied to reduce the risk of injury. Whether an in-dwelling catheter is left in place will depend on the nature and anticipated length of surgery. Gentle tissue handling and attention to haemostasis should be applied to all procedures, irrespective of route. Prophylactic ureteric stenting should be considered if a difficult dissection is anticipated, which can aid ureteric identification in addition to allowing conservative management of minor ureteric injuries. To reduce the chance of complications when introducing the pneumoperitoneum during laparoscopy, one of the more frequent occasions when complications occur, the ideal entry point is at the umbilicus where the aponeurosis is adherent to the peritoneum. This is also the ideal site to introduce the primary trocar in the majority of patients, unless significant adhesions from previous surgery are anticipated, or the patient is markedly obese or very thin. In these instances, Palmer’s point (3 cm below the left costal margin in the mid-clavicular line) should be considered or an open entry technique (Hasson) utilized. Trendelenburg position is best avoided when introducing the pneumoperitoneum and during primary trocar insertion, as this distorts the insertion angle, increasing the risk of vascular injury, and brings the bowel up out of the pelvis and towards the umbilicus. Most gynaecologists favour the closed technique with a Veress needle and rely on tactile sensation when penetrating the abdominal cavity. Insufflation carbon dioxide pressure should initially be low on initial entry into the peritoneal cavity, after which pressure may increase to 20e25 mmHg prior to inserting the primary trocar. An alternative method to enter the peritoneal cavity is an open, or Hasson technique, where the skin, rectus sheath and peritoneum are incised under direct vision and a blunt cannula inserted to achieve the pneumo- peritoneum. Although there remains controversy over which is the safer method, there is no evidence to favour one technique over the other. Recently developed visual access trocars and Veress needles may help reduce injury, but evidence at present is lacking. Once the primary trocar and laparoscope have been inserted, a full inspection of the entry site and a 360 assessment of the peritoneal cavity is made to assess pathology and identify any damage. The Trendelenburg position can then be employed, to move bowel out of the pelvis and secondary ports inserted perpendicular to the skin under direct vision, while maintaining the pneumoperitoneum at 20e25 mmHg. The intra-abdominal pressure can then be reduced to 15 mmHg to avoid anaesthetic complications. Pelvic vessels are more at risk from insertion of secondary ports, although direct visualization to control entry should reduce this happening. The inferior epigastric vessels are at risk with insertion of lateral ports; visualizing the vessels with the laparoscope and placing insertion sites lateral to the vessels is advisable. If these vessels are damaged, they may bleed during the laparoscopy and limit visualization; a sustained slow blood loss may be underestimated. Alternatively the port cannula may tamponade the vessels, so that significant bleeding occurs only after it is removed. Port sites should be inspected after gas release and instrument removal to check for delayed bleeding at the end of the procedure. The final port should be removed with the laparoscope in place, having first released the pneumo- peritoneum, to prevent a loop of bowel or omentum herniating into the wound. Recognizing and managing complications Uterine injury Trauma to the uterine cervix or body can occur with any intra- uterine surgery, but is more likely during therapeutic than diagnostic procedures. Initial cervical dilatation is usually required, but if forceful, creation of a false passage or uterine perforation can occur. This is more common with nulliparity, previous cervical surgery and in post-menopausal women. Hormonal changes during pregnancy relax smooth muscle, which also increases the risk of uterine trauma. Perforation with a blunt instrument is less likely to cause intraperitoneal visceral or vascular injury, although suspicion of injury to surrounding structures should be considered. If the patient remains haemo- dynamically stable, in-patient observation and antibiotic prophylaxis is all that is usually required. Perforation with suction, sharp curettage or an operating hysteroscope is more likely to result in visceral or vascular injury. Laparoscopy may be performed if the patient is stable, to inspect for damage and examine the bowel, adnexa and pelvic side walls. If the intra- uterine procedure cannot be abandoned, proceeding under laparoscopic vision is advisable. A laparotomy may be indicated if the patient is unstable, or the extent of the injury cannot be adequately assessed or repaired laparoscopically. Lateral perfo- rations through the cervix or into the broad ligament may be difficult to recognize, since the injury can be retroperitoneal, but should be suspected in the presence of a broad ligament hae- matoma. These can be observed directly for enlargement and REVIEW OBSTETRICS, GYNAECOLOGY AND REPRODUCTIVE MEDICINE 20:3 76 Ó 2009 Elsevier Ltd. All rights reserved.
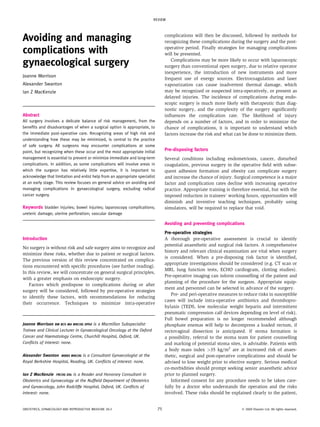
- 3. most can be managed conservatively. However, if the haema- toma does enlarge, or the patient becomes unstable, exploration, preferably by a surgeon with experience in pelvic side wall and ureteric dissection, may be required to ligate damaged vessels. During monopolar operative hysteroscopic procedures, hypotonic, electrolyte-free distension media, such as 1.5% glycine, are used. These carry an increased risk of fluid overload, leading to rare complications such as pulmonary or cardiac failure. Bipolar instruments can be used with isotonic media, and although fluid overload can still occur, the relatively high sodium content of isotonic media makes hyponatraemia and hypo- osmolality much less likely. Excessively high intra-uterine pressures (usually 60e75 mm Hg is adequate for good vision) and long procedures (90 min) should be avoided. Recognition of fluid overload is paramount and careful monitoring in theatre of fluid deficit is vital. A fluid deficit of 1000 ml should be a guide to terminate the procedure and/or expedite the end of an operation. Fluid overload is a complication which can rarely result in permanent cerebral injury due to hypo-osmolality. Post-operative symptoms of hyponatraemia include headache, nausea, vomiting, restlessness, muscle cramps and agitation. The management of hyponatraemia is multidisciplinary, involving critical care and anaesthetic staff. Treatment is generally supportive, by decreasing fluid overload and normalizing the serum sodium level. A slow increase back to normal is optimal, as a too rapid increase has been associated with complications including central pontine myelinolysis. If the sodium level is 120 mmol/L, intensive care support may be indicated. Air embolism during hysteroscopic surgery is extremely unlikely, but can be fatal. It can occur when air is introduced into the cavity, for example with repeated removal and replacement of the hys- teroscope during an operative procedure. Air can then be compressed into small venous channels that are disrupted during the procedure. Urinary tract injuries Although bladder injuries are more common than ureteric injuries during gynaecological surgery, the latter are usually more serious, especially if not recognized at the time of surgery. Because of this, assistance from a urologist should be considered when dealing with ureteric injuries. Bladder injury: Full-thickness damage to the bladder wall should be recognized at the time of surgery. If there is a suspicion of damage during laparotomy or laparoscopy, a 100e200 ml solution of diluted methylene blue can be instilled into the bladder, using a urethral catheter, to identify the site of damage. Small extra-peritoneal defects will usually heal spontane- ously, if the bladder is drained with a catheter for 7e10 days. If the defect requires suturing, the ureters should be identified to avoid damage during the bladder repair. If in doubt, the bladder can be opened, ureteric orifices identified and stents placed under direct vision. Partial thickness defects are usually closed as a single layer with 2/0 absorbable interrupted or continuous sutures through the muscle and serosal layers. Full-thickness injuries are usually closed in two layers, the first involving the mucosa and muscle and the second the muscle and serosa, burying the first layer. The bladder should be left catheterized for 7e10 days to allow healing, with a check cystography to confirm integrity before catheter removal. Larger defects may also need an intra-abdominal drain for 2e3 days and supra-pubic cathe- terization, in addition to a urethral catheter. A cystogram should be performed at about 10 days, via the urethral catheter, to check bladder integrity before removal of the urethral catheter. The supra-pubic catheter can then be clamped intermittently to check voiding function. If a penetrating injury of the bladder is sus- pected during a trans-vaginal (TVT) or trans-obturator (TOT) tension-free tape procedure, the bladder should be inspected by cystoscopy with the needles still in-situ (Figure 1). If confirmed, these needles create a small hole and can be managed conser- vatively by withdrawing the needles and draining the bladder with an in-dwelling catheter over-night. If bladder injury goes unrecognized at the time of surgery, or the mechanism of injury means that there is delayed perforation, the patient may present with anuria, urinary incontinence, metabolic disturbance due to urinary ascites (hyperkalaemia, hyper- natraemia, uraemia, metabolic acidosis), a distended, tender abdomen, paralytic ileus or haematuria. In the post-operative setting, the best investigation is a cystogram, when a radio-opaque solution is instilled into the bladder via a urinary catheter. This should demonstrate if there is urinary leakage, unless the bladder is insufficiently distended, when overlying bowel may occlude a small defect. If a urethral injury is suspected, a cystogram should not be performed via a urethral catheter, since the catheter may pass through the defect and cause further injury. If a urethral injury is suspected (rare unless radical cancer surgery is performed) then a retrograde urethrogram should be performed. Ureteric injury: Injury to the ureter includes: obstruction by inadvertent ligation (most commonly in the ureteric canal); obstruction due to distortion of the ureter by an adjacently positioned suture; direct surgical incision of the ureteric wall; inadvertent crushing with a clamp; or ischaemic damage with subsequent necrosis secondary to diathermy or laser damage. If the damage is unrecognized, it may lead to chronic ureteral obstruction or fistula formation. Delayed repair of injury is more likely to result in long-term sequelae and so recognition of damage at the time of surgery is essential and requires a good Figure 1 TVT needle perforating the bladder at cystoscopy. Image courtesy of Miss N Price and Mr S Jackson. REVIEW OBSTETRICS, GYNAECOLOGY AND REPRODUCTIVE MEDICINE 20:3 77 Ó 2009 Elsevier Ltd. All rights reserved.
- 4. understanding of the anatomical course of the ureter with systematic checking of ureteric function (peristalsis) and integ- rity at the time of surgery. If a misplaced suture or clamp is noted at the time of surgery, this should be removed immediately. If ureteric peristalsis is preserved, no further management is required. However, if there are concerns about ureteric function or possible ischaemia, or if there is a partial ureteric transaction, a ureteric stent can be inserted. This will allow drainage of the kidney into the bladder and also help to prevent stricture formation. Stents are normally inserted cystoscopically with fluoroscopic guidance and should be removed 6e12 weeks following insertion. If damage to the ureteric wall is suspected at the time of surgery, retrograde ureteropyelography is performed by cystos- copy: a ureteric catheter is placed through the ureteral orifice and contrast injected with fluoroscopic screening, to identify any obstruction or defect in the wall. Alternatively diluted methylene blue dye can be injected proximally into the ureter and directly observed for extravasation of dye. If the ureter is intact, then management can either be conservative, or a ureteric stent can be placed, depending on the nature of injury. For more extensive ureteric damage (for example, transection, loss of a segment or significant thermal injury), treatment depends on the location of injury. Above the pelvic brim, a short segment of ureter (2 cm) can be resected to healthy tissue and joined as an end-to-end ureteroureterostomy. The cut ends of the ureter are spatulated and sutured with a 4/0 absorbable suture over a ureteric catheter, to maintain patency. The anastomosis should be water-tight, but not so tight as to cause ischaemic necrosis, and a drain should be inserted adjacent to the anasto- mosis for 3e4 days. More extensive damage will require implantation of the damaged ureter into the contra-lateral normal ureter, with an end-to-side anastomosis. Below the pelvic brim the ureter can be re-implanted into the bladder: if the injury is close to the bladder (4 cm), the ureter can be carefully mobi- lized (with preservation of the adventitial blood supply) and re-implanted into the bladder. Securing the cut end of the ureter with a 3/0 absorbable stay suture, the dome of the bladder is entered, ureteric orifices identified and a site for re-implantation identified near the dome of the bladder to prevent traction on the ureter. An entry is made through the bladder wall, either directly or through a sub-mucosal tunnel in the bladder wall, to prevent reflux of urine and the ureter is drawn into the bladder, using the stay suture. The ureteric end is spatulated and sutured to the inside of the bladder with four 3/0 absorbable sutures and several 3/0 absorbable sutures placed to anchor the ureter to the outside of the bladder. A psoas hitch is recommended to prevent excessive tension on the anastomosis. This is performed by mobilizing the bladder and placing several 2/0 absorbable sutures between the muscle layer of the bladder and the fascial covering over the psoas muscle. A Boari flap is often performed in such situations, to further reduce the tension on the ureteric re-implantation, especially if a portion of ureter is lost or requires resection. To do this, a psoas hitch is performed and a full- thickness flap is cut from the anterior bladder wall and the distal ureter (spatulated) is re-implanted directly (or via a sub-mucosal tunnel) into the upper end of the bladder flap using 4/0 absorb- able sutures. The edges of the flap are closed with one layer of interrupted 3/0 absorbable sutures. A ureteric catheter is left in-situ to maintain patency and the bladder drained with a urethral or supra-pubic catheter for 10 days. In more than 70% of cases ureteric injury is recognized post- operatively. A chronically occluded ureter will lead to the development of hydronephrosis and loss of renal function in the affected kidney. Hydronephrosis may be asymptomatic or present with loin pain. If pyelonephritis develops symptoms include loin pain, fever and rigours. Necrosis of a ureter may result from unrecognized ligation, crush injury or devasculari- zation from excessive stripping of the ureter from the surrounding tissues, from which it derives its blood supply. This may lead to stenosis and hydronephrosis with loss of renal function, or fistula formation and leakage of urine into the peritoneal cavity, or a uroma in the retroperitoneal space. Either urinary ascites or a uroma may become infected, presenting with signs of sepsis and urinary ascites may cause a paralytic ileus. However, if the vaginal vault has been opened at the time of surgery, urinary ascites is likely to drain out of the vagina and present with profuse watery vaginal discharge. In the case of bilateral ureteric damage, or damage to a solitary functioning kidney, the patient will present with anuria and rapidly develop uraemia, which must be urgently investigated and treated, possibly requiring percutaneous nephrostomies to preserve renal function, as a matter of considerable urgency. Investigations will depend on the presenting symptoms, but will generally include measuring serum electrolytes and creati- nine levels, blood gases (reabsorption of urine can lead to metabolic acidosis) and full blood count; C reactive protein and blood and urine cultures should be sent for microbiology, if the patient is pyrexial. If excessive drain or vaginal fluid is present, fluid should be sent for measurement of creatinine and electro- lytes and compared to serum levels; normal exudates should have levels similar to serum while raised creatinine levels would suggest urine. However, as urinary ascites will be mixed with peritoneal exudates to a variable degree, levels may not be as high as those in urine and should be interpreted with caution. Post-operative imaging will depend on the clinical presenta- tion and can assess hydronephrosis, renal function and ureteric continuity. Ultrasound will detect hydronephrosis, ascites or a pelvic mass. Retrograde ureteropylography can be performed using a flexible cystoscope, and will determine the continuity of the ureter and allow for stent placement. A CT scan in excretion phase can be used to image kidneys, ureters and bladder. It also can demonstrate renal function (a non-functioning kidney will not excrete contrast medium), hydronephrosis and presence of ascites or cystic collections, but may not be as useful as retro- grade ureteropylography or intravenous urography (IVU) for examining the continuity of the ureter or determining the level of urinary leak. Bowel injuries Bowel injury can lead to considerable morbidity and mortality and experienced surgical assistance should be sought at an early stage. Ideally, bowel injury should be noted at the time of surgery, although diathermy, laser damage and crush injuries may lead to ischaemic necrosis and breakdown of the bowel wall within a few days following surgery. Damage bowel should be isolated with betadine-soaked swabs, to avoid generalized leakage of contents into the abdominal cavity. REVIEW OBSTETRICS, GYNAECOLOGY AND REPRODUCTIVE MEDICINE 20:3 78 Ó 2009 Elsevier Ltd. All rights reserved.
- 5. The bowel wall is repaired with interrupted 3/0 absorbable sutures on a non-traumatic needle and sutures are hand-tied to oppose and create an air-proof seal, but not so tight as to cause ischaemia, increasing the risk of dehiscence of the repair. Longitudinal injuries can be closed horizontally, to help avoid stricture forma- tion. Sutures should include w5 mm of serosa and muscle layers, and either sub-mucosa or 1 mm of mucosa, to invert the mucosa and reduce the risk of fistula formation (Figure 2). If the damage is superficial and the mucosa not breached, sutures should include only muscle and serosal layers with the aim of burying the defect. Occasionally, a damaged section may need to be removed because of a major laceration, or if vessels in the bowel mesen- tery have been damaged resulting in ischaemia of the bowel wall. This will require a primary anastomosis, which can be end-to- end, end-to-side, or side-to-side. There are a variety of techniques and suture materials used for bowel repairs and there is little evidence that one approach is superior to another. An interrupted suturing approach is described here, as recommended by the Royal College of Surgeons Basic Surgical Skills Course. Bowel is clamped with soft bowel clamps, to prevent escape of bowel contents. 3/0 absorbable stay sutures on an atraumatic round-bodied needle are placed at the ante-mesenteric and mesenteric borders, including w5 mm of serosa, muscle and sub- mucosa and either emerging between the mucosa and sub- mucosa or involving w1 mm of mucosa. The sub-mucosa is the strongest layer and it is essential to include this in the suture. These sutures are not tied at this stage, but the ends are left long and clipped to help stabilize and manipulate the bowel. Starting at the mesenteric border, sutures are placed (as described above) at w5 mm intervals and tied. The bowel is then turned over by passing the mesenteric stay suture through the defect in the mesentery and moving the ante-mesenteric suture to display the posterior aspect of the anastomosis and further sutures are placed at 5 mm intervals, as before. The bowel is returned to its original position, by passing the mesenteric stay suture back through the defect, before the stay sutures are tied and cut. Any defect in the mesentery should then be repaired with interrupted sutures, to prevent bowel loops becoming incarcerated. Following repair, the bowel should be checked for haemostasis, adequacy of circulation and air leaks and the abdominal cavity washed-out with warm saline. The patient will require intra- operative antibiotics according to local antibiotic policy, which may be continued post-operatively, depending on the degree of contamination of the abdominal cavity. Increasingly anasto- moses are repaired with staples and frequently a side-to-side anastomosis is created using a GIA and TA stapler (Figure 3). If bowel injury is not noted at the time of surgery or there is a subsequent leak from a primary repair, presenting symptoms include abdominal pain, vomiting, fever and rigours. There may be signs of sepsis (fever, tachycardia, hypotension), and the abdomen may be tender, with guarding and rebound tenderness; bowel sounds are normally absent, if peritonitis is present. If the leak is localized to the pelvic area, vaginal or rectal examination may be useful to feel for masses, tenderness or cervical excita- tion. General surgical assistance should be sought, since faecal peritonitis carries a high mortality rate and dehiscence of subsequent bowel repair is more common. In patients diagnosed with post-operative bowel perforation, the degree of pre-operative investigations will depend on the clinical condition of the patient with resuscitation instigated without delay. Immediate investigations should include full blood count, urea and electrolytes, blood and urine culture, following which antibiotics can be started. Liver function tests, amylase, lipase, calcium and glucose may help to rule out other causes for the acute presentation. Imaging may include an erect chest X-ray to check for sub-diaphragmatic air, supine and erect abdominal X-rays to look for dilated loops of bowel, fluid/gas levels and a visible falciform ligament (which can be seen as an oblique line in the right upper quadrant down to the umbilicus and is visible if there is significant free air in the abdomen). However, free air in the abdominal cavity is not a reliable sign in patients within 24e48 h of abdominal surgery. Ultrasound examination may detect signs of bowel perforation (localized collections of gas or free fluid). A CT scan may detect inflam- matory changes and evidence of localized perforation. Diagnostic laparoscopy may be used, although the open approach is prob- ably safer than blind entry in this situation to reduce the risk of further trauma. Surgical repair will involve a laparotomy with careful washout of the abdominal cavity and post-operative antibiotics. Following repair of a bowel injury a temporary defunctioning stoma, to reduce the risk of faecal peritonitis from anastomotic dehiscence, should be considered. In the case of a primary repair of healthy small bowel, without abdominal contamination, a covering ileostomy is not normally required. Use of a loop stoma (either ileostomy or colostomy) is a matter for debate amongst colorectal surgeons in other situations. However, a defunctioning stoma is normally recommended, if there is faecal contamination or the bowel is not healthy. Recent randomized control trial evidence suggests that a covering stoma should be used following a low anterior resection for rectal cancer since anastomotic leak rates were nearly three times higher without a covering stoma (10.3% vs. 28%), as were Figure 2 Placement of bowel sutures. 3/0 Absorbable stay sutures on an atraumatic round-bodied needle include w5 mm of serosa, muscle and sub-mucosa and either emerge between the mucosa and sub-mucosa or involve w1 mm of mucosa. The sub-mucosa is the strongest layer and it is essential to include this in the suture. Image from the Royal College of Surgeons Basic Surgical Skills Course Handbook. Copyright: The Royal College of Surgeons of England. Reproduced with permission. REVIEW OBSTETRICS, GYNAECOLOGY AND REPRODUCTIVE MEDICINE 20:3 79 Ó 2009 Elsevier Ltd. All rights reserved.
- 6. urgent re-operation rates (8.6% vs. 25.4%). These data support the use of a covering stoma following significant injury to large bowel. Vascular injury Vascular injury should be noted at the time of surgery and routine checking for haemostasis examining all pedicles or secondary port sites following removal, is recommended prior to closure or withdrawal of the laparoscope. Despite precautions to avoid injury to superior epigastric vessels at the time of secondary port insertion during laparos- copy, damage can still occur. Options for achieving haemostasis of epigastric vessels include: (a) opening the skin and fascia with direct ligation of the vessels; (b) ligation with a through-and- through suture or laparoscopically-placed suture; (c) use of laparoscopic electrocautery; (d) tamponade from an inflated Foley balloon catheter secured under traction with a clamp at the skin surface. During open surgery, vessel ends should be identified, clam- ped with non-toothed forceps and re-ligated, taking care of surrounding structures. It may be necessary to dissect out or skeletalize the vessel to identify it, especially if the end of the ovarian artery has retracted into the retroperitoneal tissues. Defects in larger vessels require expert repair by a vascular surgeon, to prevent stenosis, dissection or thrombus formation and embolization. Repair of larger vessels requires dissection to display anatomy and gain control of the up-stream and down- stream flow with vascular clamps or slings (avoiding damage to the intima) and repair the wall with prolene sutures (6e7 throws for secure knot-tying). Handling of vessels should be limited to avoid damage and the intima should never be handled. Sutures are placed from inside to out (intimaeadventitia) wherever possible, to prevent formation of a flap and dissection of the intima from the adventitia. Since not all sutures can be placed like this, down-stream sutures are placed inside-out as a priority. Transverse arteriotomies can be closed by primary closure, but longitudinal arteriotomies will require patching to prevent stenosis. Occasionally a suture may slip following surgery, leading to significant haemorrhage. This will normally happen within the first few hours following surgery. Signs may include pallor, an increased respiratory rate, which may be the first sign, reduced urine output, tachycardia and hypotension; beware, because young fit patients can lose a significant blood volume before displaying significant haemodynamic changes. Because of this, careful, frequent post-operative observations should be taken and the modified early warning score (MEWS) (Table 1) helps to highlight concerning trends; patients should be reviewed by a doctor if the MEWS is 4 or more. Nerve injury Neuropraxia is a recognized complication of prolonged surgery. Problems may arise in the lower limb, secondary to extended lithotomy position in either femoral or peroneal nerves, espe- cially if lithotomy poles are used (where rates of 20% have been reported). Problems will be noted post-operatively, when there is unexpected motor or sensory block. Most cases will resolve over time, but may require specialist neurological Figure 3 a Mesenteric vessels are identified, secured with Robert’s clamps, transected and ligated with 2/0 absorbable ties. The damaged section is cleaned of mesenteric fat and excised with a GIA stapler. b Ante-mesenteric borders are aligned and a 2/0 absorbable suture placed w10 cm away from the stapled ends between the two ante-mesenteric borders, with soft bowel clamps placed further away from the stapled ends to prevent leakage of bowel contents when the bowel is opened. Small diagonal cuts are made across the ante-mesenteric stapled ends, to allow placement of the arms of the GIA stapling device into the bowel. The device is closed, but not fired until each side has been checked to ensure that mesentery is not caught in the stapling device. c The small defect in the end closed with further staples (TA stapler), ensuring that the staple intersection is slightly off-set. The mesenteric defect is closed with interrupted sutures. Images reproduced with permission courtesy of Covidien (www.autosuture.com). REVIEW OBSTETRICS, GYNAECOLOGY AND REPRODUCTIVE MEDICINE 20:3 80 Ó 2009 Elsevier Ltd. All rights reserved.
- 7. investigation and physiotherapy to aid recovery and prevent further complications, such as contractures. Brachial plexus injuries, due to shoulder restraints to aid the Trendelenburg position, or arms abducted above the shoulders on arm boards, have been reported. These will normally resolve over time with physiotherapy, but may be very disabling in the short term. Post-traumatic neuropathy can result from damage to nerves during surgery or at injection sites. Symptoms are usually felt locally, at the site of injury and radiate to the involved nerve distribution area. Symptoms of damage include neuralgic pain (burning, shooting) and possibly hypersensitivity, numbness, tingling, and muscle weakness depending on the functions of the nerve involved. There may be changes in the sympathetic nervous system to that area (excessive sweating, temperature and colour changes) and allodynia (experiencing normal stimuli as painful). If the nerve is damaged within the skin, there may be point tenderness over the site of the injury, which will reproduce the abnormal symptoms. Investigations to consider include nerve conduction studies and cross-sectional imaging to identify sites of nerve compres- sion. Treatment will normally be in conjunction with a chronic pain service. Oral medications for neuralgic pain include tricyclic antidepressants and anti-epileptics, e.g. amitriptyline and gaba- pentin. Doses should be increased gradually to reduce side effects. Desensitization injections with dilute local anaesthetic and steroid can reduce scar hypersensitivity and nerve blocks can be used with long-acting local anaesthetic and steroid in some anatomical locations. Permanent blocks e.g. with phenol may help initially, but may cause deafferentation pain afterwards. Surgery may be appropriate to decompress a nerve, remove suture materials, or excise a neuroma, but may exacerbate symptoms in the long term. All scars are capable of causing neuralgic pain, and although the mechanism is not completely understood, may involve entrapment of nerves within scar tissue. Conclusions No surgery is without risk and complications are inevitable. However, correct training and mindful surgery, with a thorough knowledge of the anatomy will help reduce avoidable compli- cations. Appropriate pre-operative counselling of women is crucial in gynaecological surgery, as many procedures are for symptom control of non-life threatening conditions. Many complications are relatively minor and appropriate immediate management will avert long-term sequelae. It is therefore vital to be able to recognize when complications have occurred, institute ‘first-aid’, and enlist senior and experienced assistance when necessary. Last, but by no means least, the patient should be made aware of any complication as soon as possible following surgery. Thorough explanation of events and likely conse- quences is essential and follow up for further debriefing may be required depending on the circumstances. Patients accept that complications may occur and are sometimes unavoidable. However, failing to communicate adverse events and answer questions appropriately is not. A FURTHER READING http://www.autosuture.com/autosuture/pageBuilder. aspx?topicID¼31271;breadcrumbs¼0:122497. http://www.gmc-uk.org/guidance/ethical_guidance/consent_guidance/ index.asp. Morrison J, MacKenzie IZ. Avoiding and managing complications during gynaecological surgery. Obst Gyn Repro Med 2007; 17: 105e11. Preventing entry-related laparoscopic injuries (Green-top guideline 49). London: The Royal College of Obstetricians and Gynaecologists, May 2008. Thomas WEG. The Intercollegiate Basic Surgical Skills Course: Participant handbook. 3rd Edn. London: The Royal College of Surgeons of England, 2002. Modified early warning score for post-operative observations Score 3 2 1 0 1 2 3 Respiratory rate (minÀ1 ) 8 9e14 15e20 21e29 29 Heart rate (minÀ1 ) 40 41e50 51e100 101e110 111e129 129 Systolic BP (mm Hg) 70 71e80 81e100 101e199 !200 Urine output (ml/kg/h) Nil 0.5 Temperature ( C) 35 35.1e36 36.1e38 38.1e38.5 !38.6 Neurological Alert Reacting to voice Reacting to pain Unresponsive Table 1 Practice points C Pre-surgical preparation of patient, surgeon and operating team is central to avoiding complications. C Careful explanation of procedure and risks to the patient is required for consent to be valid. C Sequelae of a complication can be minimized by prompt recognition and initial management. C Prompt recourse to appropriately experienced assistance is advised. C Careful explanation and counselling of the patient following complications is essential. REVIEW OBSTETRICS, GYNAECOLOGY AND REPRODUCTIVE MEDICINE 20:3 81 Ó 2009 Elsevier Ltd. All rights reserved.
