Hepatitis c. diagnosis and treatment.assld guidelines.2016 .2017
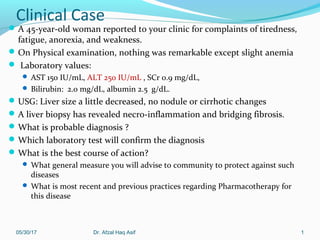
- 1. Clinical Case A 45-year-old woman reported to your clinic for complaints of tiredness, fatigue, anorexia, and weakness. On Physical examination, nothing was remarkable except slight anemia Laboratory values: AST 150 IU/mL, ALT 250 IU/mL , SCr 0.9 mg/dL, Bilirubin: 2.0 mg/dL, albumin 2.5 g/dL. USG: Liver size a little decreased, no nodule or cirrhotic changes A liver biopsy has revealed necro-inflammation and bridging fibrosis. What is probable diagnosis ? Which laboratory test will confirm the diagnosis What is the best course of action? What general measure you will advise to community to protect against such diseases What is most recent and previous practices regarding Pharmacotherapy for this disease 05/30/17 1Dr. Afzal Haq Asif
- 2. Dr. Afzal Haq Asif Associate Professor Applied Therapeutics College of Clinical Pharmacy King Faisal University, Al-Ahsa AASLD/IDSA recommendations-2016 Pharmacotherapy Principles and Practice 4th ed. 2016
- 3. ILO’s At the end of the session, the attendee will be able to Define the acute and chronic viral hepatitis C Diagnose based upon clinical and lab data Design therapeutic objectives Design therapeutic and follow up evaluation plan for patient Resolve drug related problems of patient Educate the patient to improve therapeutic outcome 05/30/17 3Dr. Afzal Haq Asif
- 4. Introduction In 60’s only A & B In 70’s, it was found that neither agent is found responsible for post trans fusion Hepatitis, So Hepatitis caused by NANB was introduce The major cause of parenterally transmitted NANB hepatitis. In 1989, the genome was cloned from the serum of an infected chimpanzee. 05/30/17 4Dr. Afzal Haq Asif
- 5. Introduction: fact sheet An estimated 130–170 million people are infected with hepatitis C worldwide Out of 100 people who contract the infection, 75–85% will develop chronic infection, 60–70% develop chronic liver disease, 5–20% develop cirrhosis over the course of their chronic infection, 1–5% will die of complications including hepatocellular carcinoma (HCC) 7.3 % individuals were found seropositive for Anti-HCV antibodies in a study carried out on 15323 Saudi patients 05/30/17 5Dr. Afzal Haq Asif
- 6. Figure 1. Seroprevalence of anti-HCV antibodies using chemiluminescent microparticle immunoassay. Abdel-Moneim AS, Bamaga MS, Shehab GMG, Abu-Elsaad A-ASA, et al. (2012) HCV Infection among Saudi Population: High Prevalence of Genotype 4 and Increased Viral Clearance Rate. PLoS ONE 7(1): e29781. doi:10.1371/journal.pone.0029781 http://www.plosone.org/article/info:doi/10.1371/journal.pone.0029781 The total seroprevalence among the 15323 tested individuals. B. HCV seroprevalence in males in comparison to females 05/30/17 Dr. Afzal Haq Asif 6
- 7. HCVHCV is a single stranded RNA virus Genus Hepa-civirus, (HCV) Family Flavi-viridae Characterized by a high spontaneous mutation rate 11 genotypes (90 sub-types) , (1a, 1,b, 2a, 3b etc) USA: Genotype 1 (subtypes 1a, 1b, and 1c) 70%–75%. Genotypes 2 (subtypes 2a, 2b, and 2c) and 3 (3a and 3b) are less common KSA: Genotype 4 is common Ia And Ib less common Genotype 2, 3, 5 and 6 are least common 05/30/17 7 Genotype helps determine therapy duration and likelihood of responding to therapy Dr. Afzal Haq Asif
- 8. Epidemiology Worldwide seroprevalence 3% based upon anti- HCV) up to 180 million people infected chronically. Variation in distribution 0.4% to 1.1% in North America to 9.6% to 13.6% in North Africa. A primary cause of death from liver disease The leading indication for liver transplantation in the United States Deaths as a result of liver failure or HCC) will continue to rise in the next two decades Responsible for 85% of cases associated with posttransfusional NANB hepatitis Occurs among persons of all ages, highest between 20 to 39 years, with a male predominance. Blacks have a substantially higher prevalence of chronic HCV infection than do whites. 05/30/17 8Dr. Afzal Haq Asif
- 9. Transmission Mainly blood-borne (transfusion, intravenous drug abuse) High risk: Transfusion, intravenous drug abuse Low risk: Hemodialysis continuous Snorting cocaine or other drugs Occupational exposure needle stick , health workers Body piercing and acupuncture with unsterilized needle Tattooing From pregnant mother to child Nonsexual household contacts (rare)05/30/17 9Dr. Afzal Haq Asif
- 10. Pathogenesis: replication in Liver cells 05/30/17 10Dr. Afzal Haq Asif
- 11. Pathogenesis Direct cell injury due to viral replication Genotype 1 is associated with higher viral replication, Genotype 1b associated with more progressive liver disease Immune mediated cell injury: CD8+ and CD4+ lymphocytes in portal, peri-portal, and lobular areas in patients with HCV infection 05/30/17 11Dr. Afzal Haq Asif
- 12. Clinical Presentation Acute: less than 6 months Usually asymptomatic; if Symptoms do appear, they are generally nonspecific: fatigue, weakness, anorexia, and jaundice; typically appear within 4–12 hours after exposure. Rapid progression to fulminant liver disease is infrequent. Diagnosis of acute infection is extremely rare. Chronic: more than 6 months Most chronically ill patients with HCV infection remain asymptomatic for years, presenting with symptoms during the fifth and sixth decades of life Most who present for medical attention have chronic infection; Anorexia, abdominal pain, fever, jaundice, malaise, nausea, Symptoms associated with hepatocellular carcinoma and liver cirrhosis. Extrahepatic disease (e.g., cryoglobulinemia, glomerulonephritis) may also be present. The level of virus in the serum (HCV RNA) is not highly correlated with stage of disease. 05/30/17 12Dr. Afzal Haq Asif
- 13. HCV infection: course of disease Asymptomatic: 30% Moderate to severe hepatitis in 30% <20 years of age Acute: Antibodies against HCV (anti-HCV) in the blood indicate infection. About 15% to 45% of patients have acute hepatitis C that resolves without any further complication Chronic: In 70% of cases: when infection persists for more than 6 months and viral replication is confirmed by HCV RNA levels, because of Ineffective host immune system, with cytotoxic T lymphocytes unable to eradicate the HCV, Approximately 55% to 85% of chronic cases progress to mild, moderate, or severe hepatitis (Child-Pugh score) In 15% to 30% Persistent damage to hepatic cells leading to cirrhosis after several decades of infection Factors for cirrhosis: obesity, diabetes, heavy alcohol use, male sex, and coinfections with HIV or HBV. Age over 40 years at the time of infection 5-year mortality with compensated cirrhosis 9%, 5-year mortality with Decompensated cirrhosis 50% Once cirrhosis is confirmed, the risk of developing HCC is about 2% to 4% per year05/30/17 Dr. Afzal Haq Asif 13
- 14. Course of the Disease, contd; Hepatocellular Carcinoma in HCV infection 1% to 4% of patients per year during the first 5 years after cirrhosis develop hepatocellular carcinoma 7% after 5 years of cirrhosis 14% at 10 years; Higher in men Higher in older patients 05/30/17 14 NIH Consensus Program. National Institutes of Health consensus development conference panel statement: management of hepatitis C. Hepatology. 1997;26:2S-10S. Dr. Afzal Haq Asif
- 15. Spontaneous resolution Early studies 15–25% of persons who developed transfusion- associated acute hepatitis C, 14–29% HCV-infected blood donors, persons with ‘community-acquired’ infection, IV drug abusers and children with leukemia Later studies: 42 and 45%. among infected children, young women and even some persons with community-acquired hepatitis C Young age at the time of infection is an important determinant of the likelihood of spontaneous recovery. 05/30/17 15 The historyof the‘‘natural history’’of hepatitisC(1968-2009): Liver International 2009; 29(s1): 89–99 Dr. Afzal Haq Asif
- 16. Extra-hepatic manifestations Rheumatoid arthritis Glomerulonephritis Cryo-globenemia 05/30/17 16Dr. Afzal Haq Asif
- 17. Lab Testing in HCV infection Antibody to HCV (anti-HCV) Used for screening and diagnosing HCV infection. Positive result should be confirmed by HCV RNA testing. Unable to differentiate between acute, chronic, and resolved infection Testing should be done with an FDA-approved test including laboratory- based assays and point-of-care assay (i.e., OraQuick HCV Rapid Antibody Test). HCV nucleic acid test (NAT) Active disease Tests HCV RNA in blood to detect viremia, to confirm current (active) infection HCV RNA: only quantitative is uses Used to detect and/or quantify viral nucleic acid in the following individuals: Positive HCV antibody test result Negative HCV antibody test result and suspected of having liver disease Negative HCV antibody test result and who might have been exposed to HCV within the past 6 months Those who are immunocompromised All assays are 98%–99% specific. International reporting standard for HCV RNA is in international units per milliliter05/30/17 Dr. Afzal Haq Asif 17
- 18. Diagnosis Clinical Signs and symptoms: not suggestive, unless thorough history and Labs Serum anti-HCV antibodies: 99% sensitivity and specificity..indicate HCV can be detected 8–12 weeks post exposure Serum HCV RNA: can be detected 2 weeks post exposure Quantitative: used for Confirmation of Diagnosis Monitoring response to therapy Qualitative: only to confirm diagnosis 50 IU/ml: 100 copies/mL to confirm diagnosis 98% specificity Liver biopsy: for cirrhosis, prognosis ALT: Non specific Genotype: for treatment duration and response 05/30/17 18Dr. Afzal Haq Asif
- 19. Estimate Severity of liver disease 05/30/17 Dr. Afzal Haq Asif 19
- 20. AASLD, (American Association for the Study of Liver Diseases) 2016 05/30/17 20Dr. Afzal Haq Asif
- 21. Who should be screened Persons who have injected illicit drugs in the recent and remote past Persons with conditions of a high prevalence of HCV infection including: With HIV infection With hemophilia who received clotting factor prior to 1987 Who have ever been on hemodialysis With unexplained abnormal aminotransferase levels Immigrants from countries with a high prevalence of HCV infection Prior recipients of transfusions or organ transplants prior to July 1992: Persons who were notified that they had received blood from a donor who later tested positive for HCV infection Persons who received a transfusion of blood or blood products Persons who received an organ transplant Children born to HCV-infected mothers Health care, emergency medical and public safety workers after a needle stick injury or mucosal exposure to HCV-positive blood Current sexual partners of HCV-infected persons 05/30/17 21Dr. Afzal Haq Asif
- 22. Prevention No Vaccine is available Risk factor modification Intravenous drug abuse: treatment with oral methadone Sexual contact: appropriate barrier contraception Avoid blood exposure: Occupational (universal precautions) or other contact Avoid sharing toothbrushes or razors or receiving a tattoo HAV and HBV vaccine to prevent further progression of liver disease 05/30/17 22Dr. Afzal Haq Asif
- 23. Educate about the following 05/30/17 Dr. Afzal Haq Asif 23 Avoid sharing toothbrushes and dental or shaving equipment Cover any bleeding wound to prevent possibility of others coming into contacted with infected blood Counsel to avoid using illicit drugs and enter substance abuse treatment Counsel to avoid reusing or sharing syringes, needles, or any supplies for those continuing to use injectable drugs • Avoid donating blood In those coninfected with HIV, consider using barrier precautions to prevent sexual transmission Proper cleaning of contaminated surfaces with a dilution of 1 part household bleach to 9 parts water Always wear gloves when cleaning up blood spills
- 24. AASLD, (American Association for the Study of Liver Diseases) guidelines-2016 05/30/17 24Dr. Afzal Haq Asif
- 25. Goals of Therapy Acute: Eradicate HCV infection in acute To prevents the development of chronic HCV infection Chronic: Attain Sustained Virologic Response (SVR) inChronic Undetectable HVC RNA, after therapy completion Decrease HCV associated morbidity and mortality Normalize biochemical markers Improve clinical symptoms Prevent progression to cirrhosis and HCC Prevent development of end stage liver disease 05/30/17 25 These goals are partly achieved by Pharmacotherapy Dr. Afzal Haq Asif
- 26. General recommendations To assist with making the best treatment decision for each patient each recommendation is classified as follows: Recommended – Favored for most patients Alternative – Optimal in a particular subset of patients Treatment regimens and length vary according to HCV genotype and prior treatment history. Treatment during an acute infection: Should be delayed at least 12–16 weeks to allow for spontaneous clearance before therapy initiation. HCV RNA level should be monitored during this time. 05/30/17 Dr. Afzal Haq Asif 26
- 27. Treatment of Chronic HCV infection Difficult patient population: individualized consideration Normal ALT (treatment dependent on genotype, degree of fibrosis, symptoms) Liver biopsy indicating no or mild fibrosis Advanced liver disease (fibrosis or decompensated cirrhosis) Recurrence after liver transplantation Patients younger than 18 years Co-infection with HIV or HBV Chronic Kidney Disease Non responders or relapses 05/30/17 27Dr. Afzal Haq Asif
- 28. AASLD, (American Association for the Study of Liver Diseases) guidelines-2016 05/30/17 28Dr. Afzal Haq Asif
- 29. Strength and level of Evidence 05/30/17 Dr. Afzal Haq Asif 29
- 30. New regimen: 2016: Geno 1.a Genotype 1a Treatment-naïve Patients without Cirrhosis – Rating: Class I, Level A 1. Recommended 1. Daily fixed-dose combination of elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 2. Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks 3. Daily fixed-dose combination of paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) plus twice-daily dosed dasabuvir (250 mg) with weight- based RBV for 12 weeks 4. Daily simeprevir (150 mg) plus sofosbuvir (400 mg) for 12 weeks 2. Alternative: 1. Daily fixed-dose combination of elbasvir (50 mg)/grazoprevir (100 mg) with weight-based RBV for 16 weeks Genotype 1a Treatment-naïve Patients with compensated Cirrhosis 1. Daily fixed-dose combination of elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 2. Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks05/30/17 Dr. Afzal Haq Asif 30
- 31. New regimen: 2016-Geno-1b Genotype 1b Treatment-naïve Patients without Cirrhosis – Rating: Class I, Level A 1. Recommended 1. Daily fixed-dose combination of elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 2. Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks 3. Daily fixed-dose combination of paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) plus twice-daily dosed dasabuvir (250 mg) for 12 weeks 4. Daily simeprevir (150 mg) plus sofosbuvir (400 mg) for 12 weeks Genotype 1b Treatment-naïve Patients with compensated Cirrhosis 1. Recommended 1. Daily fixed-dose combination of grazoprevir (100 mg)/elbasvir (50 mg) for 12 weeks 2. Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks 3. Daily fixed-dose combination of paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) plus twice-daily dosed dasabuvir (250 mg) for 12 weeks 2. Alternative: 1. Daily simeprevir (150 mg) plus sofosbuvir (400 mg) with or without weight-based RBV for 24 weeks 2. Daily daclatasvir (60 mg) plus sofosbuvir (400 mg) with or without weight-based RBV for 24 weeks 05/30/17 Dr. Afzal Haq Asif 31
- 32. New regimen: 2016: Geno-1 Genotype 1 Treatment-naïve Patients NOT RECOMMENDED 1. Daily sofosbuvir (400 mg) and weight-based RBV for 24 weeks. Rating: Class IIb, Level A 2. PEG-IFN/RBV with or without sofosbuvir, simeprevir, telaprevir, or boceprevir for 12 weeks to 48 weeks. Rating: Class IIb, Level A 3. Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral. Rating: Class III, Level A 05/30/17 Dr. Afzal Haq Asif 32
- 33. New regimen: 2016: Geno-2 Genotype 2 Treatment-naïve Patients without Cirrhosis –Recommended 1. Daily sofosbuvir (400 mg) and weight-based RBV for 12 weeks 1. Rating: Class I, Level A 2. Daily daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 12 weeks who are not eligible to receive RBV. Class IIa, Level B Genotype 2 Treatment-naïve Patients with compensated Cirrhosis 1. Recommended 1. Daily daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 16 weeks to 24 weeks 1. Rating: Class IIa, Level B 2. Daily sofosbuvir (400 mg) and weight-based RBV for 16 weeks to 24 weeks 1. Rating: Class IIa, Level Calternative 2. Not Recommended 1. PEG-IFN/RBV for 24 weeks Rating: Class IIb, Level A 2. Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral Rating: Class III, Level A 3. Telaprevir-, boceprevir-, or ledipasvir-containing regimens Rating: Class III, Level A 05/30/17 Dr. Afzal Haq Asif 33
- 34. New regimen: 2016: Geno-3 Genotype 3 Treatment-naïve Patients without Cirrhosis –Recommended Class I, Level A 1. Daily daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 12 weeks Rating: 2. Daily sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks who are eligible to receive PEG-IFN. 1. Genotype 3Treatment-naïve Patients with compensated Cirrhosis- Recommended 1. Daily sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks who are eligible to receive PEG-IFN. Rating: Class I, Level A 1. Daily daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 24 weeks with or without weight-based RBV Rating: Class IIa, Level B 2. Alternative: with or without cirrhosis Rating: Class I, Level A 1. Daily sofosbuvir (400 mg) and weight-based RBV for 24 weeks is an Alternative regimen for treatment-naïve patients with HCV genotype 3 infection, regardless of cirrhosis status, who are daclatasvir and IFN ineligible. 3. Not Recommended for Geno-3 1. PEG-IFN/RBV for 24 weeks to 48 weeks Rating: 2. Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral Rating: 3. Telaprevir-, boceprevir-, or simeprevir-based regimens 05/30/17 Dr. Afzal Haq Asif 34
- 35. New regimen: 2016: Geno-4 Genotype 4 Treatment-naïve Patients without Cirrhosis –Recommended 1. Daily fixed-dose combination of paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) and weight-based RBV for 12 weeks Rating: Class I, Level A 2. Daily fixed-dose combination of elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks Rating: Class IIa, Level B 3. Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks Rating: Class IIa, Level B 1. Genotype 4 Treatment-naïve Patients with compensated Cirrhosis 2. Recommended 1. Daily fixed-dose combination of paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) and weight-based RBV for 12 weeks Rating: Class I, Level B 2. Daily fixed-dose combination of elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks Rating: Class IIa, Level B 3. Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks Rating: Class IIa, Level B 3. Alternative: regardless of cirrhosis status. 1. Daily sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks who are IFN eligible, Rating: Class II, Level B 05/30/17 Dr. Afzal Haq Asif 35
- 36. New regimen: 2016: Geno-4: Not recommended Not Recommended for Treatment Naïve : PEG-IFN/RBV with or without simeprevir for 24 weeks to 48 weeks Rating: Class IIb, Level A Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral Rating: Class III, Level A Telaprevir- or boceprevir-based regimens Rating: Class III, Level A 05/30/17 Dr. Afzal Haq Asif 36
- 37. New regimen: 2016: Geno-5/6 Genotype 5/6 Treatment-naïve Patients with or without Cirrhosis –Recommended 1. Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks is a Recommended regimen for treatment-naïve patients with HCV genotype 5 or 6 infection, regardless of cirrhosis status. 1. Rating: Class IIa, Level B 1. Alternative: regardless of cirrhosis status. 1. Daily sofosbuvir (400 mg) and weight-based RBV plus weekly PEG- IFN for 12 weeks who are IFN eligible, regardless of cirrhosis status. 1. Rating: Class IIa, Level B 2. Not Recommended for Geno-5/6 1. PEG-IFN/RBV with or without simeprevir for 24 weeks to 48 weeks Rating: Class IIb, Level A 2. Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral Rating: Class III, Level A 3. Telaprevir- or boceprevir-based regimens Rating: Class III, Level A 05/30/17 Dr. Afzal Haq Asif 37
- 38. Geno-1 & 4 with Decompensated Cirrhosis Moderate to severe Decompensated Cirrhosis Child Turcotte Pugh [CTP] class B or C May or May Not be Candidates for Liver Transplantation, Including Those with Hepatocellular Carcinoma Should be referred to a medical practitioner with expertise in that condition (ideally in a liver transplant center). Rating: Class I, Level C Pharmacotherapy options:Class I, Level A Daily fixed-dose combination ledipasvir (90 mg)/sofosbuvir (400 mg) with low initial dose of RBV (600 mg, increased as tolerated) for 12 weeks Rating: Daily daclatasvir (60 mg*) plus sofosbuvir (400 mg) with low initial dose of RBV (600 mg, increased as tolerated) for 12 weeks For RBV Ineligible. Class II, Level C Daily daclatasvir (60 mg) plus sofosbuvir (400 mg) for 24 weeks Daily fixed dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) for 24 weeks If Prior Sofosbuvir-based Treatment has Failed: Daily fixed-dose combination of ledipasvir (90 mg)/sofosbuvir (400 mg) with low initial dose of RBV (600 mg, increased as tolerated) for 24 weeks Paritaprevir, ombitasvir, and dasabuvir may cause rapid onset of direct hyperbilirubinemia within 1-to-4 weeks of starting treatment without ALT elevations that can lead to rapidly progressive liver failure and death 05/30/17 Dr. Afzal Haq Asif 38 The dose of daclatasvir may need to increase or decrease when used concomitantly with cytochrome P450 3A/4 inducers and inhibitors, respectively
- 39. Geno-2 & 3 with Decompensated Cirrhosis Moderate to severe Decompensated Cirrhosis Child Turcotte Pugh [CTP] class B or C May or May Not be Candidates for Liver Transplantation, Including Those with Hepatocellular Carcinoma Should be referred to a medical practitioner with expertise in that condition (ideally in a liver transplant center). Rating: Class I, Level C Pharmacotherapy options: Class II, Level B Daily daclatasvir (60 mg*) plus sofosbuvir (400 mg) with low initial dose of RBV (600 mg, increased as tolerated) for 12 weeks 05/30/17 Dr. Afzal Haq Asif 39 The dose of daclatasvir may need to increase or decrease when used concomitantly with cytochrome P450 3A/4 inducers and inhibitors, respectively
- 40. Things Not recommended in Decompensated Cirrhosis Any IFN-based therapy Rating: Class III, Level A Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral Rating: Class III, Level A Telaprevir-, boceprevir-, or simeprevir-based regimens Paritaprevir-, ombitasvir-, or dasabuvir-based regimens Rating: Class III, Level B Grazoprevir- or elbasvir-based regimens Rating: Class III, Level C 05/30/17 Dr. Afzal Haq Asif 40
- 41. 05/30/17 Dr. Afzal Haq Asif 41
- 42. 05/30/17 Dr. Afzal Haq Asif 42
- 43. 05/30/17 Dr. Afzal Haq Asif 43
- 44. Reading Assignment: Page 381 Pharmacotherapy: Principles and Practice 4th ed. 2016 1. Paritaprevir, ritonavir, ombitasvir, elbasvir, grazoprevir MoA Drug Interactions Contraindications Adverse effects Monitoring 05/30/17 Dr. Afzal Haq Asif 44
- 45. 05/30/17 Dr. Afzal Haq Asif 45
- 46. Who Have failed with Prior PEG-IFN/RBV Therapy: Geno-1a Genotype Recommended Therapies Alternative Therapy options 1 a Without cihhosis 1. ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 2. Elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 3. daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 12 weeks 4. simeprevir (150 mg) plus sofosbuvir (400 mg) for 12 weeks 1. elbasvir (50 mg)/grazoprevir (100 mg) with weight-based RBV for 16 weeks 1a With compensate d cirrhosis 1. elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 2. ledipasvir (90 mg)/sofosbuvir (400 mg) for 24 weeks 3. ledipasvir (90 mg)/sofosbuvir (400 mg) plus weight-based RBV for 12 W’s 1. paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) plus twice- daily dosed dasabuvir (250 mg) and weight-based RBV for 24 weeks 2. elbasvir (50 mg)/grazoprevir (100 mg) with weight-based RBV for 16 weeks 3. daclatasvir (60 mg*) plus sofosbuvir (400 mg) with or without weight- based RBV for 24 weeks 4. simeprevir (150 mg) plus sofosbuvir (400 mg) with or without weight- based RBV for 24 weeks 05/30/17 46Dr. Afzal Haq Asif
- 47. Who Have failed with Prior PEG-IFN/RBV Therapy: Geno-1b Genotype Recommended Therapies Alternative Therapy options 1 b Without cirrhosis 1. ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks 2. Elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 3. daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 12 weeks 4. simeprevir (150 mg) plus sofosbuvir (400 mg) for 12 weeks 5. paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) plus twice-daily dosed dasabuvir (250 mg) for 12 weeks 1. elbasvir (50 mg)/grazoprevir (100 mg) with weight-based RBV for 16 weeks 1b With compensat ed cirrhosis 1. elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 2. ledipasvir (90 mg)/sofosbuvir (400 mg) for 24 weeks 3. ledipasvir (90 mg)/sofosbuvir (400 mg) plus weight-based RBV for 12 W’s 4. paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) plus twice-daily dosed dasabuvir (250 mg) for 12 weeks 1. daclatasvir (60 mg*) plus sofosbuvir (400 mg) with or without weight-based RBV for 24 weeks 2. simeprevir (150 mg) plus sofosbuvir (400 mg) with or without weight-based RBV for 24 weeks 05/30/17 47Dr. Afzal Haq Asif
- 48. Who Have failed with Prior PEG-IFN/RBV Therapy: Geno-2 Genotype Recommended Therapies Alternative Therapy options Geno-2 Without cihhosis 1. Sofosbuvir (400 mg) and weight-based RBV for 12 weeks 2. Daclatasvir (60 mg) plus sofosbuvir (400 mg) for 12 weeks 1. None Geno-2 With compensated cirrhosis 1. Daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 16 weeks to 24 weeks 2. Sofosbuvir (400 mg) and weight-based RBV for 16 weeks to 24 weeks 1. Sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks GENO-2 Sofosbuvir plus Ribavirin Treatment- experienced Patients 1. Daclatasvir (60 mg*) plus sofosbuvir (400 mg) with or without weight-based RBV for 24 weeks 2. Sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks Not recommended 1. PEG-IFN/RBV with or without telaprevir or boceprevir 2. Ledipasvir/sofosbuvir 3. Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral 05/30/17 48Dr. Afzal Haq Asif
- 49. Who Have failed with Prior PEG-IFN/RBV Therapy: Geno-3 Genotype Recommended Therapies Alternative Therapy options Geno-3 Without cirrhosis 1. Daclatasvir (60 mg*) plus sofosbuvir (400 mg) for 12 weeks 2. sofosbuvir (400 mg) and weight-based RBV plus weekly PEG- IFN for 12 weeks Geno-3 With compensated cirrhosis 1. Sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks 2. daclatasvir (60 mg*) plus sofosbuvir (400 mg) with weight-based RBV for 24 weeks Sofosbuvir and RBV Treatment- experienced 1. Daclatasvir (60 mg*) plus sofosbuvir (400 mg) with weight-based RBV for 24 weeks 2. Sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks Not Recommended PEG-IFN/RBV for 24 weeks to 48 weeks Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral Telaprevir-, boceprevir-, or simeprevir-based regimen 05/30/17 49Dr. Afzal Haq Asif
- 50. Who Have failed with Prior PEG-IFN/RBV Therapy: Geno-4 Genotype Recommended Therapies Alternative Therapy options 4 Without cirrhosis 1. Paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) (PrO) and weight-based RBV for 12 weeks 2. elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 3. ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks 1. Sofosbuvir (400 mg) and weight- based RBV plus weekly PEG- IFN for 12 weeks 2. Sofosbuvir (400 mg) and weight- based RBV for 24 weeks 4 With compensat ed cirrhosis 1. Paritaprevir (150 mg)/ritonavir (100 mg)/ombitasvir (25 mg) (PrO) and weight-based RBV for 12 weeks 2. Elbasvir (50 mg)/grazoprevir (100 mg) for 12 weeks 3. Ledipasvir (90 mg)/sofosbuvir (400 mg) and weight-based RBV for 12 weeks 4. Ledipasvir (90 mg)/sofosbuvir (400 mg) for 24 weeks Not Recommen ded for Geno-4 1. PEG-IFN/RBV with or without telaprevir or boceprevir 2. Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral 05/30/17 50Dr. Afzal Haq Asif
- 51. Who Have failed with Prior PEG-IFN/RBV Therapy: Geno-5,6 Genotype Recommended Therapies Alternative Therapy options Geno-5,6 with or without cirrhosis 1. ledipasvir (90 mg)/sofosbuvir (400 mg) for 12 weeks 1. sofosbuvir (400 mg) and weight-based RBV plus weekly PEG-IFN for 12 weeks Not Recomme nded 1. Monotherapy with PEG-IFN, RBV, or a direct-acting antiviral 2. Telaprevir- or boceprevir-based regimens 05/30/17 51Dr. Afzal Haq Asif
- 52. Liver Transplant Recipients: HCV Genotype Recommendedb (duration in weeks) Alternativec (duration in weeks) Genotype 1 (treatment naïve and experiencedd ± compensated cirrhosise ) LED/SOF (12) + RBV (12) LED (24) + SOF (24) SOF (12) + SIM (12) ± RBV (12) PAR/RIT/OMB (24) + DAS (24) + RBV (24) Genotype 2 (treatment naïve and experiencedd ± compensated cirrhosise ) SOF (24) + RBV (24) ----- Genotype 4 (treatment naïve and experiencedd ± compensated cirrhosise ) LED/SOF (12) + RBV (12) LED (24) + SOF (24) Genotype 1, 3, or 4 (treatment naïve and experiencedd + decompensated cirrhosisf ) LED/SOF (12) + RBVg (12) ----- Genotype 2 (treatment naïve or experiencedd + decompensated cirrhosisf ) SOF (24) + RBVc (24) 05/30/17 Dr. Afzal Haq Asif 52
- 53. Dose adjustment with Renal Failure Renal Impairme nt eGFR/ CrCl, mL/ minute LED DAS PAR OMB SOF SIM RBV Interferon Peg- IFNα2a Peg- IFNα2 b Mild 50−80 Standa rd Standa rd Standa rd Standa rd Standa rd Standa rd Standard Standard Standard Moderate 30−50 Standa rd Standa rd Standa rd Standa rd Standa rd Standa rd Alternate doses of 200 mg/day and 400 mg/day every other day Standard ↓ dose by 25% Severe <30 * * * * * * 200 mg/day 135 mcg/ week ↓ dose by 50% End-stage renal disease or hemodialysis * * * * * * 200 mg/day 135 mcg/ week 1 mcg/kg / week 05/30/17 Dr. Afzal Haq Asif 53 * = data unavailable DAS = dasabuvir; eGFR/CrCl = estimated glomerular filtration rate/creatinine clearance; HCV = hepatitis C virus; LED = ledipasvir; OMB = ombitasvir; PAR = paritaprevir; Peg-IFN = pegylated interferon; RBV = weight-based ribavirin; RIT = ritonavir; SIM = simeprevir; SOF = sofosbuvir
- 54. Cost of therapy Price for sofosbuvir in the United States is $1000 per day, or $84,000 to $168,000 for a 12- or 24-week treatment regimen, excluding the cost of other coadministered medications. The cost for a 28-day supply of simeprevir is $22,120, excluding other drugs given concomitantly. If the combination of simeprevir and sofosbuvir is prescribed, the cost is well over $150,000 for a 12-week course. The combination tablet Harvoni (sofosbuvir/ledipasvir) has a wholesale price of about $94,500 for a 12-week treatment course. The Viekira Pak containing ombitasvir, paritaprevir, ritonavir, and dasabuvir has a wholesale acquisition cost of $83,320 to $167,640 for 12 or 24 weeks of treatment, respectively05/30/17 Dr. Afzal Haq Asif 54
- 55. 05/30/17 Dr. Afzal Haq Asif 55
- 56. Before Therapy Before initiating HCV therapy Assess potential for drug-drug interactions. The following laboratory tests are recommended within 12 weeks of therapy initiation: CBC, INR, hepatic function panel, TSH (if regimen contains PegINF), calculated GFR. The following laboratory tests are recommended any time before therapy initiation: HCV genotype and subtype, quantitative HCV viral load (if quantification will influence therapy duration may need to obtain laboratory measurment within a few weeks of therapy initiation). 05/30/17 Dr. Afzal Haq Asif 56
- 57. During Therapy Assessment of medication adherence, monitoring of adverse effects, and potential for drug-drug interactions should occur through clinic visits or telephone contact as clinically indicated. The following laboratory tests are recommended within 4 weeks of initiation therapy: CBC, creatinine concentration, calculated GFR, hepatic function panel. Consider increasing the frequency if regimen contains medications with increased likelihood for drug-related toxicities, such as ribavirin (may need to obtain CBC more often for example). If regimen contains PegINF: TSH every 12 weeks HCV quantitative viral load After 4 weeks of therapy and 12 weeks after therapy is completed. At the end of treatment and 24 weeks after therapy is completed. 05/30/17 Dr. Afzal Haq Asif 57
- 58. Monitoring during therapy Monitor WBC, ANC, and platelets either weekly or biweekly during the first month of therapy and monthly thereafter if stable while on pegylated interferon. Monitor hemoglobin levels weekly or biweekly during the first month and monthly thereafter if stable while on ribavirin. Monitor for fatigue, shortness of breath, and chest pain and dermatological complications while on ribavirin; if significant complaints, discontinue treatment. . Monitor TSH and fasting lipid panel every 12 weeks while receiving pegylated interferon Monitor serum creatinine in patients receiving ribavirin to detect renal insufficiency that may result in ribavirin accumulation and toxicity (eg, hemolytic anemia). Monitor total bilirubin concentrations every 2 to 4 weeks while on simeprevir, and perhaps more often if the patient is cirrhotic or has decompensated liver disease. 05/30/17 Dr. Afzal Haq Asif 58
- 59. When to discontinue anti-viral therapy… Monitor HCV quantitative viral load . If HCV quantitiative viral load is detectable at week 4 of treatment, repeat test after an additional 2 weeks (i.e., treatment week 6). If threatment week 6 viral load has increased by greater than 10-fold (>1 log10 IU/mL), it is recommended to discontinue therapy. 05/30/17 Dr. Afzal Haq Asif 59
- 60. For pregnant on RBV Preganancy-related issues while receiving ribavirin Women of childbearing potential should have serum pregnancy test before initiation of therapy if regimen contains ribavirin. Contraception use and possible pregnancy should be assessed during therapy at appropriate intervals and for 6 months after the completion of treatment for women of childbearing potential and for female partners of men who receive ribavirin. 05/30/17 Dr. Afzal Haq Asif 60
- 61. Not applicable or required for exam…just for the sake of comparison 05/30/17 61Dr. Afzal Haq Asif
- 62. Treatment (Old) First-line treatment for acute HCV includes pegylated interferon plus ribavirin. once-weekly PEG-IFN and a daily oral dose of ribavirin in two divided doses 05/30/17 62 Genotype Pegylated-IFN Dose weight Ribavirin Dose Duration 1 Peginterferon α2a 180 mcg/wk Less than 75 Kg 1000 mg 48 weeks Peginterferon α2b 1.5 mcg/wk More than 75 kg 1200 mg 2,3 Peginterferon á2a 180 mcg/wk 800 mg 24 weeks Peginterferon α2b 1.5 mcg/wk At week 1, 2, 4 and then interval of 4-8 weeks monitor: •Symptom of Disease •Side Effects of therapy •Blood count •Aminotransferases Dr. Afzal Haq Asif
- 63. Treatment: Genotype 4 (old) A meta-analysis leads to recommendations for patients with genotype 4: Combination therapy with Peg IFN plus ribavirin for 48 weeks. Combination of Peg IFN-α2b plus a fixed dose of ribavirin (10.6mg/kg/day) for 36weeks may also result in a sufficient EVR. genotype 6: with Peg IFN-α plus ribavirin for 48 weeks was more effective than treatment for 24 weeks. 05/30/17 63Dr. Afzal Haq Asif
- 64. Follow up 05/30/17 64Dr. Afzal Haq Asif
- 65. 05/30/17 Dr. Afzal Haq Asif 65
- 66. Sofosbuvir (Sovaldi) NS5B polymerase inhibitor Indications: HCV genotypes 1, 2, 3, and 4, including those with: Hepatocellular carcinoma HCV/HIV coi-nfections Dosing: 400-mg tablet once daily with or without food No dosing recommendations for glomerular filtration rate (GFR) less than 30 mL/minute Dose of ribavirin with Sofosbuvir should be reduced when used with sofosbuvir 600 mg daily Discontinue Ribaviren if hemoglobin is less than 8.5 g/dL Reduce the ribavirin dose if there is a greater than 2-g/dL decrease in hemoglobin during any 4-week period, and Discontinue if hemoglobin is less than 12 g/dL, despite 4 weeks at reduced dose. If GFR 30–50 mL/minute, use alternating doses of 200 and 400 mg daily; If GFR less than 30 mL/minute or if end-stage renal disease/hemodialysis, reduce to 200 mg/day Adverse effects: Fatigue, headache Drug interactions: Avoid use with potent P-glycoprotein inducers. Avasimibe, carbamazepine, phenytoin, rifampin, St John’s wort,tipranavir/ritonavir Concentrations are significantly affected by anticonvulsants (carbamazepine, phenytoin, phenobarbital, and oxcarbazepine), rifabutin, rifampin, St. John’s wort, and tipranavir/ritonavir. 05/30/17 66Dr. Afzal Haq Asif
- 67. Semiprevir (Olysio) NS5B polymerase inhibitor Indications: Chronic HCV genotype 1 Dose:150 mg once daily with food for 12 weeks, combined with PEG-IFN and ribavirin. Dose recommendations cannot be made for patients of East Asian ancestry or those with moderate to severe hepatic impairment Contraindications: Pregnant women or male partners of pregnant women (category C, but must be used with ribavirin, which is category X) Screening for the NS3Q80K polymorphism. Alternative therapies should be considered in patients with genotype 1a and this polymorphism With moderate or strong inducers or inhibitors of CYP3A is not recommended. It Inhibits of OATP1B1/3 (Organic anion-transporting polypeptide) and P- glycoprotein Adverse effectes: Photosensitivity, rash; contains a sulfonamide moiety but no reports of problems with sulfa allergy 05/30/17 67Dr. Afzal Haq Asif
- 68. Substrates of OATP Atorvastatin (Lipitor®) - OATP1B1, OATP1B3 Bilirubin - OATP1B1, OATP1B3 Bosentan (Tracleer®) - OATP1B1 Digoxin (Lanoxin®) - OATP1B3 Empagliflozin (Jardiance®) - OATP1B1, OATP1B3 Ezetimibe (Zetia®) - OATP1B1 Fexofenadine (Allegra®) - OATP1B1, OATP1B3, OATP1A2, OATP2B1 Fluvastatin (Lescol®) - OATP1B1 Glyburide (DiaBeta®) - OATP1B1 Irinotecan (Camptosar®) - OATP1B1 Telmisartan (Micardis®) - OATP1B3 Valsartan (Diovan®) - OATP1B1, OATP1B3 Lovastatin (Mevacor®) - OATP1B1 Methotrexate (Rheumatrex®) - OATP1B1, OATP1B3 Olmesartan (Benicar®) - OATP1B1, OATP1B3 Paritaprevir (Viekira Pak™) - OATP1B1, OATP1B3 Pitavastatin (Livalo®) - OATP1B1, OATP1B3 Pravastatin (Pravachol®) - OATP1B1, OATP2B1 Repaglinide (Prandin®) - OATP1B1 Rifampin - OATP1B1, OATP1B3 - Rosuvastatin (Crestor®) - OATP1B1, OATP1B3 Simvastatin (Zocor®, Zetia®) - OATP1B1 Thyroxine (Synthroid®, Levoxyl®) - OATP1B1 05/30/17 68Dr. Afzal Haq Asif
- 69. Ledipasvir Ledipasvir; approved in combination with sofosbuvir (Harvoni) FDA indication (approved October 2014): Treatment of chronic HCV genotype 1 infection as a fixed dose combination with sofosbuvir. Not recommended to administer with other products containing sofosbuvir Dose and administration One tablet (90 mg of ledipasvir and 400 mg of sofosbuvir) by mouth once daily with or without food No dose adjustments required for mild or moderate renal impairment. Safety and efficacy is unknown in those with severe renal impairment (CrCl < 30 mL/ minute) or end-stage renal disease and in dialysis. No dose adjustments required for mild, moderate, or severe hepatic impairment (Child Pugh Class A, B, or C). Safety and efficacy is unknown in those with decompensated cirrhosis. Formulations: Oral; 90 mg ledipasvir and 400-mg sofosbuvir tablet Treatment duration: Depends on patient population; see Table 05/30/17 Dr. Afzal Haq Asif 69
- 70. Ledipasvir Adverse events The most notable adverse events include fatigue, headache, nausea, diarrhea, and insomnia. Safety data in prescribing guidelines are pooled from three phase 3 trials in subjects with genotype 1 with or without compensated cirrhosis. Very few subjects permanently discontinued therapy because of adverse events: 0%, <1%, and 1% who received therapy for 8, 12, or 24 weeks, respectively. Laboratory abnormalities Bilirubin elevations: Greater than 1.5 times ULN in 3%, <1%, and 2% of subjects treated for 8, 12, and 24 weeks, respectively Lipase elevations: Asymptomatic, transient, greater than 3 times ULN in <1%, 2%, and 3% of subjects treated for 8, 12, and 24 weeks, respectively Creatine kinase: Not assessed in ledipsavir/sofusbuvir treatment trials. Asymptomatic elevations (grade 3 or 4) have been previously reported with sofosbuvir therapy 05/30/17 Dr. Afzal Haq Asif 70
- 71. Ribavirin adverse effect monitoring Oral nucleoside analog Available as 200-mg tablets (Copegus) or capsules (Rebetol) Adverse Effect Hemolytic anemia: Upto 10% of patients (usually within 1–2 weeks of initiating therapy): decrease dose to 600 mg/day when hemoglobin drops to 10 g/dL or less, and discontinue when hemoglobin drops to 8.5 g/dL or less May worsen underlying cardiac disease; Monitor complete blood cell count (CBC) at baseline, 2 weeks, 4 weeks, Decrease dose to 600 mg/day if hemoglobin drops more than 2 g/dL in any 4-week period during treatment. May use epoetin or darbepoetin to stimulate red blood cell production, improve anemia (J Clin Gastroenterol 2005;39:S9-S13),05/30/17 71Dr. Afzal Haq Asif
- 72. Ribavirin adverse effect monitoring Teratogenicity: Category X drug; Requires a negative pregnancy test at baseline and every month up to 6 months after treatment, Use of two forms of barrier contraception during treatment and for 6 months after treatment. Contraindicated in patients with a creatinine clearance (CrCl) less than 50 mL/minute pancreatitis, pulmonary dysfunction (dyspnea, pulmonary infiltrate, and pneumonitis), insomnia, irritability or depression (often referred to as “riba rage”), and pruritus. 05/30/17 72Dr. Afzal Haq Asif
- 73. Interferon INF α 2 b: Used for HBV and HBC infections Half life : 2-3 hours Dose: 3 MIU subcutaneous 3 times /week Geno-1: 4/48 weeks Geno2: 3/24 weeks Peg IFN α2 a: with branched peg chain Used for HBV and HVC infections Half life: 160 hours Dose: 180 mcg s/c once weekly Geno-1 4/48 Geno-2 3/24 PegIFN -α2b : linear peg chain Half life: 40 hours Dose 1.5 mcg/kg s/c once weekly IFN alfaxon-1: Used for HCV treatment Dose: naïve: 9 mcg Non responder: 15 mcg s/c 3 times a week Naïve for 24 weeks INF non responder: 48 weeks 05/30/17 73Dr. Afzal Haq Asif
- 74. Interferon: adverse effectsMost Common: influenza-like symptoms (e.g., fever, headache, myalgia, fatigue), Hematologic abnormalities: neutropenia, thrombocytopenia, Neuropsychiatric disorders (e.g., depression 40 % and anxiety), injection site reactions, diarrhea, nausea, insomnia, alopecia, pruritis, and anorexia. Less common but serious adverse severe psychiatric (i.e., suicidal ideation), cardiovascular (i.e., myocardial infarction), Endocrine (e.g., thyroid dysfunction, diabetes mellitus), immune (e.g., psoriasis, lupus), pulmonary, and ophthalmologic disorders, pancreatitis, colitis, and other serious infections. 05/30/17 74Dr. Afzal Haq Asif
- 75. Managing the adverse effects of interferon Hematological: Anemia: common reason for discontinuation and dose reduction (upto 23% of patients) Tx: Erythropoitic growth factor: Epoitin Alfa: 40-6000 units weekly Darbepoitin alfa 3 mcg every 2 weeks IFN induced neutropenia: Recombinant granulocyte colony stimulating factor (filgrastim) is safe and effective Thrombocytopenia: Eltrombopag, an orally active thrombopoietin receptor agonist that received FDA approval for chronic ITP (hepatotoxic) 05/30/17 75Dr. Afzal Haq Asif
- 76. Managing the adverse effects of interferon Neuropsychiatric: Prompt recognition and early treatment required Depression: 44% during first 3 months Tx: Close monitoring and follow up by a team of health care providers including psychiatrist Prophylactic anti-depressants are debated Uncontrolled psychiatric symptoms: contraindication for Tx 05/30/17 76Dr. Afzal Haq Asif
- 77. HIV and HCV co-infection 30% HIV patient also have HCV infection Rapid progression of liver damage SVR is lower as compared to HVC alone A threshold CD4 count of at least 350 cells/μL has been suggested for initiation of antiviral therapy; Treatment is not recommended if CD4 counts lower than 200 cells/mL. Adverse effects are more common: Anemia with Ziduvodine and Ribavirin combination Mitochondrial toxicity, pancreatitis, liver failure, and death ; more common with Didanosine and Ribavirin combination ???? Liver transplant Assignment: Please read the following and prepare for exam: http://www.hcvguidelines.org/full-report/unique-patient-populations-patients-hivhcv-coinfection 05/30/17 77Dr. Afzal Haq Asif
- 78. Liver Transplant. Is this a solution? Most common indication in US: Hepatitis C virus–related end-stage liver disease Outcome: Recurrence is essential outcome Progression of liver disease is accelerated, Within 5 years after transplantation, 20% to 40% of liver allografts progress to cirrhosis; 60% to 70% of cirrhotics experience hepatic decompensation within 3 years Response rates to pegIFN and ribavirin treatment after liver transplant are lower than for patients in the pretransplant setting, Drug toxicity remains a limiting factor. 1/3 require discontinuation 05/30/17 78Dr. Afzal Haq Asif
- 79. Outcome evaluation Disease: As discussed above SVR after 4 weeks of treatment (TW4) After 1 and 6 months of end of therapy Check ALT after every 4 weeks of therapy (TW4), After 1, 6 months of end of therapy Drugs: Please review the Pharmacology of the following: Interferon Sofosbuvir Ledipasvir 05/30/17 79Dr. Afzal Haq Asif
- 80. Patient care and education-1 Educate patient for risk factors for acquiring hepatitis Educate patient about hepatotoxic drugs Educate regarding vaccination against A & B Obtain thorough PMH regarding psychiatric, cardiac, endocrine and renal disorders Assess fro adverse effects periodically Encourage for medication compliance to increase SVR Encourage fluid intake to avoid dehydration Educate all women of child bearing age, and men who are able to father a child to use 2 forms of contraception during and 6 months after therapy 05/30/17 80Dr. Afzal Haq Asif
- 81. Patient care and education contd-2 Provide patient education: How to prevent viral hepatitis Importance of taking all medication daily at scheduled time Adverse effects of medications How to self administer pegylated interferon injection correctly Importance of appropriate disposal of used injection 05/30/17 81Dr. Afzal Haq Asif
- 82. References Pharmacotherapy Practice and Principles 4th ed 2016 AASLD Guidelines July 2016, (American Association for the Study of Liver Diseases) guidelines-2016 05/30/17 82Dr. Afzal Haq Asif
- 83. 05/30/17 83 Thank You Very Much Dr. Afzal Haq Asif
