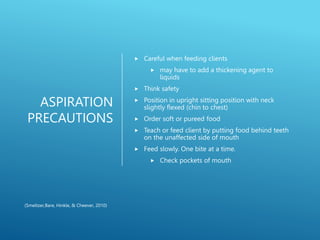
This document discusses strokes, including types like ischemic and hemorrhagic strokes. It notes that strokes are the 5th leading cause of death in the US, with 795,000 people suffering strokes annually. Risk factors include hypertension, smoking, heart disease, and diabetes. Nursing interventions focus on monitoring vital signs, administering tPA if indicated, preventing complications like aspiration, and providing rehabilitation through physical, occupational and speech therapies to address deficits in mobility, communication and cognition.