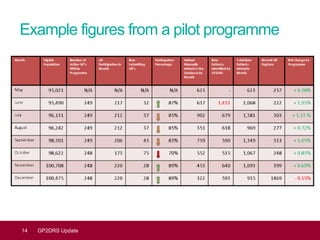
This document provides an update on GP2DRS, which is a centralized solution for sharing patient data between GP practices and local diabetes screening programs. It automates the extraction of patient lists to identify those eligible for screening more accurately and reduce workload. Benefits include reduced risk of sight loss from missed screening and more timely identification of demographic changes. Implementation may initially increase administrative workload as new patients are identified. Future improvements could include automated coding updates and potential to extract additional patient information.