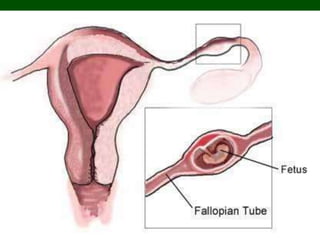
Ectopic pregnancy occurs when a fertilized egg implants outside of the uterus, usually in the fallopian tubes. Risk factors include previous pelvic inflammatory disease, pelvic surgery, IUD use, tumors, and smoking. Symptoms include vaginal bleeding and pelvic pain. Diagnosis is made through beta-hCG levels, transvaginal ultrasound showing no intrauterine pregnancy, and sometimes laparoscopy. Treatment involves surgical removal of the ectopic pregnancy through laparoscopy or laparotomy, or non-surgical options like methotrexate injections.