Benign CR Diseases.pptx
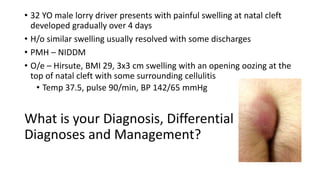
- 1. • 32 YO male lorry driver presents with painful swelling at natal cleft developed gradually over 4 days • H/o similar swelling usually resolved with some discharges • PMH – NIDDM • O/e – Hirsute, BMI 29, 3x3 cm swelling with an opening oozing at the top of natal cleft with some surrounding cellulitis • Temp 37.5, pulse 90/min, BP 142/65 mmHg What is your Diagnosis, Differential Diagnoses and Management?
- 2. The diagnosis - Pilonidal abscess • The differential diagnosis of pilonidal sinus disease • A boil. • Hidradenitis suppurativa. • Ano-rectal fistula and fissure. • Perirectal abscess. Pilonidal sinus disease is a skin disorder usually found in the midline of the natal cleft. A 'primary pit' or opening forms in the midline into which loose hairs and debris enter to create an epithelial track (sinus) which may become infected Asymptomatic, or present acutely as a Pilonidal Abscess, or become a chronically discharging Sinus/es ( midline/ lateral opening )
- 3. Pilonidal sinus disease - an acquired condition. A small midline pit develops at the site of a hair follicle. This sheds its own hair and allows keratin and debris to fill it, facilitated by the movement of the buttocks. The pit fills with debris -shed squamous epithelium and foreign material. This is driven into the depth of the pit causing a local inflammatory reaction, which further elongates the pit. A granuloma develops in the subcutaneous fat and over time, further debris, hairs, and pus are forced into the midline pit and build up under pressure to create an underlying cavity or track. An abscess may form due to moist conditions in the natal cleft that favour bacterial proliferation. A sinus (abnormal epithelialized connection with the skin surface) may develop as infection spreads, or as a result of rupture of an abscess. A sinus may have one or more secondary openings lateral to the primary pit, and if open, these may chronically discharge pus or blood.
- 4. • Occurs on average 26 / 100,000 people • Risk factors • Male gender (3–4 times more likely than in women) • Age 15–40 years • Being white (more common than in black people, due to different hair characteristics and growth patterns) • Obesity, Hirsutism • Deep natal cleft • Lifestyle or occupation which involves sitting for prolonged periods (more than 6 hours a day) • Family history of pilonidal sinus disease • Complications of pilonidal sinus disease • Abscess, Cellulitis, Sepsis • Chronic pain • Altered body image and self-esteem • Effects on personal relationships
- 5. Management • Acute pilonidal abscess • I&D ( day case under GA ) • FU in the Clinic • Meticulous perianal hygiene with regular baths or showers. • Buttock hair removal techniques, such as shaving, waxing, depilatory creams, or laser treatment • Discharging pilonidal sinus disease • Colorectal referral • Treatment of local infection/cellulitis ( Analgesia, Antibiotics, e.g., 7 days course of Flucloxacillin 500 mg qid, plus Metronidazole 400mg tds ) • wide excision of the sinus tracks, followed by primary closure or leaving the wound open to heal by secondary intention • Bascom’s Procedure • Karydakis Procedure • Limberg technique with Rhomboid transposition flap, Z-plasty
- 7. A folk tale from India that teaches intellectual awareness by illustrating how different perspectives lead to distinct points of view. • translated to the English language in the 19th century as a poem by the English writer John Godfrey Saxe. The poem illustrates how perception is based on what a person is able to see or touch Six Blind Men and The Elephant
- 8. What is your Diagnosis and Management? 31 YO male presents to A&E with anal pain, fever and unwell • 2 days h/o pain around anal area not responding to Analgesia • Noticed today a painful swelling around anal area • No previous similar history; fit, no PMH, no regular meds, smokes • O/E – Temp 37.8 C, uncomfortable • PRE – tender, swelling at 3 o’clock, mild inflammation around at the anal margin • DRE – not able to tolerate
- 9. Relevant Anatomy of the Anus/ Anal canal Puborectalis
- 10. • Internal sphincter is composed of circular, non-striated involuntary smooth muscle supplied by Autonomic Nerves System • External sphincter is composed of striated voluntary muscle supplied by Pudendal nerve • Extension from longitudinal muscle layer support the sphincter complex • The space bet sphincters – Intersphincteric plane • Superior part of external sphincter fuses with Puborectalis muscle – maintaining anorectal angle necessary for continence • Lower part of the anal canal is lined by sensitive squamous epithelium • BS – Superior, Middle and Inferior rectal (haemorrhoidal) vessels • Lymphatic drainage - Inguinal and inf mesenteric chain/para-aortic nodes • Anal glands in the submucosa and intersphincteric space at Dentate line are considered the potential source of anal sepsis
- 11. A) Pelvi-rectal supra-levator space B) Ischiorectal space C) Perianal or superficial ischiorectal space D) Marginal or mucocutaneous space E) Submucous space F) Anorectal intermuscular (intersphincteric) space 1) Pelv-irectal supra-levator abscess 2) Submucous abscess 3) Ischiorectal abscess 4) Marginal abscess 5) Perianal abscess 6) Inter-sphincteric abscess
- 12. How should the patient be assessed? • Full clinical history and Examination Duration Present of sepsis Associated GI symptoms; PRB, discharge (prev fistula), change of bowel habit GI history; diarrhoea, and pain, wt loss, F/H of IBD PMH; s/a DM, Malignancy, HIV, chemotherapy, prev organ transplant, recent pelvic surgery Drug history; any immunosuppressant , steroids • Examination – usually in left lateral position Swelling/abscess at anal verge, or minimal finding if deep sepsis DRE if possible; normally too much pain to tolerate • Investigations FBC, U & E, CRP, Clotting
- 13. How should Anorectal sepsis be treated • EUA, I(ncision) & D(rainage) • Perianal and ischiorectal sepsis - drain externally throu’ perianal skin • Intersphincteric and suprasphincteric abscesses s/b drained internally • Management of associated fistulae ( e.g., loose draining seton insertion) • Continued antibiotics if there is cellulitis/ immunocompromised patients (broad- spectrum with anaerobic and G-ve cover) • Consultation with Gastroenterologist in cases of IBD/Crohn’s for treatment • Usually FU 6-8 weeks - A cruciate incision is made into abscess cavity with excision of cruciate skin edges to deroof it - Pus swab for M C&S - Debridement of the abscess cavity, irrigated and packed with Sorbsan/Aquacel ?
- 14. What is your Diagnosis and Management? 29 YO male referred to CR Clinic with 3 months h/o intermittent discharge per rectum • H/o a perianal abscess discharged spontaneously/ did not seek medical advice • Yellowish coloured discharged sometimes blood staining of his underwear • Otherwise well/ no change of bowel function, no PMH, Smoker • O/E – G/C - NAD • PRE – a small opening at 7 o’clock position with a palpable tract • Proctoscopy reveals an internal opening in post midline, 4 cm from anal verge
- 16. • A fistula – an abnormal communication between two epithelialized surfaces • Perianal fistula – an inflammatory tract lined by granulation tissues between anorectal canal and perianal skin Types of Anal fistula (Park’s classification) 1. Intersphincteric 2. Trans-sphincteric 3. Suprasphincteric 4. Extrasphincteric Idiopathic aetiology/ Cryptoglandular hypothesis – infection begins at anal gland passing into Intersphincteric space, spread via least resistant pathway – the resulting anorectal abscess, then later a fistula develops Other conditions; Crohn’s disease, TB, hidradenitis suppurativa, HIV, foreign bodies, previous radiotherapy, trauma Goodsall’s Rule Internal opening at Dentate line
- 17. Investigation • Proctosigmoidoscopy • MRI - Gold standard – ability to demonstrate secondary extensions Coronal MRI (STIR Sequence) Primary tract running up right Ischiorectal space (short arrow) – crosses the sphincters to open into anal canal Blind Secondary tract (long arrow) at contralateral side in the roof of left ischiorectal fossa
- 18. • Eliminate the fistula • Prevent recurrence • Preserve sphincter function Procedures • Laying-open ( Fistulotomy ) • Seton insertion (loose, cutting, snug) • Fibrin glue, plug • LIFT ( Ligation of Intersphincteric Fistula Tract ) • Advancement flaps • VAAFT ( Video assisted anal fistula treatment ) • FiLaC (Fistula tract laser closure) • Defunctioning stomas Treatment
- 19. What is your Diagnosis and Management? 33 YO male referred to CR Clinic with 8 weeks h/o bright red rectal bleeding with bowel movement associated with pain and “stinging” sensation for about an hour/few hours after • H/o long-term constipation, otherwise fit and well, no change of bowel function, no PMH • GP consultation - ? Painful haemorrhoids; prescribed local agents • O/E – G/C – NAD; Abd ex - NAD • PRE – with difficulty – small posterior anal wound/ulcer noted • DRE or Anoscopy NOT possible
- 20. Anal Fissure • A tear in the lining of the mucosa of the anal canal • 90% located in posterior midline – typically result from trauma from the hard stool, also occurs from persistent diarrhoea; underlying hypertonicity (high resting pressure) of Internal sphincter • 10% anterior – birth trauma • Sentinel pile – a skin tag develops at the distal fissure margin (painful haemorrhoid) • Spasm of Internal sphincter With bowel movement - Causing pain and reduced Blood flow in the area causing Poor wound healing Chronic Anal fissure > 8weeks
- 21. Management • Normally no further investigation • Conservative measures alone heals Anal fissure up to 80% ( +6 weeks) • High-fibre diet with increased fluid intake • Sitz baths • Laxatives • Medical treatment: Topical agent – GTN (Rectogesic 0.4%), Diltiazem 2% • Facilitating local vasodilatation, relaxing sphincter, reducing anal pressure and increasing BF; Twice daily up to 8 weeks, SE – significant headache (20-30%) • BOTOX (Botulinum Toxin A) injection • relaxes sphincter, and reducing resting anal tone • Lasts for 2-3 months • Heals chronic anal fissures up to 60 – 80 % • Treatment can be repeated
- 22. Surgical operation for Anal fissure Lateral internal sphincterotomy • Open or close method – an incision over Intersphincteric Groove at 3 or 9 o’clock, internal sphincter divided for the length of fissure, not > ½ length of sphincter • High success rate >90%; Low recurrence rate • Important complication of Incontinence; variable nature and severity up to 30% Fissurectomy Anal advancement flap Anal dilatation (Lord’s procedure) Nowadays no longer perform due to high complication of anal incontinence
- 23. What is your Management? 47 YO male referred to CR Clinic with 3 months h/o intermittent bright red rectal bleeding with bowel movement which is more regular • Also notice something coming in/out with defecation, and occasionally needs manual reduction • H/o piles and had been treated with various topical and suppositories with limited success until now • Non-smoker, self-employed, fit and healthy • O/E – G/C – NAD; Abd ex - NAD • PRE – NAD • Proctoscopy – 2nd and 3rd degree Haemorrhoids
- 24. Haemorrhoids • Haemorrhoids are symptomatic Anal cushions • Anal cushions – submucosal arterio-venous vascular plexuses maintaining anal continence in Homo Sapiens Erectus • Mainly at 3, 7 and 11 o’clock position • Caused by (Exact cause is unknown) • Increased abd pressure ( excessive straining, Obesity, Pregnancy, childbirth, chronic cough) • Constipation • Genetics/ family tendency • Ageing
- 25. Symptoms • Bright-red painless bleeding • Prolapse • Mucous discharge • Itchiness (pruritus ani) • Pain (with complications/ external thrombosed haemorrhoid) Classification • First degree/Grade – bleed only • Second degree – prolapse but reduce spontaneously • Third degree – prolapse and have to manually reduce • Fourth degree – prolapsed, irreducible
- 27. Management • No further investigation unless haemorrhoids are a result of another d/s process, or rectal bleeding may be attributable to other causes ( Red Flag Signs ) – Typically this involves a flexible sigmoidoscopy or Colonoscopy • Conservative • Increase intake of fluid and fibres • Avoid constipation and straining • Stool softeners/ Laxatives • Rubber Band Ligations ( treatment of choice for 2nd degree Haemorrhoids _ • Injection of Sclerosant ( Sclerotherapy – Phenol 5% in Almond oil ) • Surgical Operations • Open (Milligan-Morgan)/ Closed (Furguson) Haemorrhoidectomy ( Ligation and Excision ) • Stapled Haemorrhoidopexy • HALO ( Haemorrhoidal Artery Ligation Operation ) or THD ( Transanal Haemorrhoidal De-arterilization ) with suture mucopexy
- 28. Stapled Haemorrhoido -pexy Excision and Ligation of Haemorrhoids/ Open technique ( Milligan Morgan )
- 29. What is your Diagnosis and Management? 71 YO female presented with 4 days h/o LIF pain • It started as an ache – getting constant and worse; today feeling hot, lethargic, anorexic and unwell; passing loose stool, no urinary symptoms • H/o similar episodes over a year, self-limiting, lasting few days • PMH – hypertension, Type 2 DM on drugs • O/E – G/C – Overweight/ flush; Temp 38.0 C, Pulse 115/min, BP 102/62 mmHg • Abd – very tender LIF with mild guarding/ rest – soft with normal BS • Bloods – Marked leucocytosis (WCC 21.5) with raised CRP (180)
- 30. Acute (Sigmoid) Diverticulitis • Differential Diagnosis • Left sided colitis • Bowel cancer complication • PID • Ovarian pathology • UTI/ Pyelonephritis • Obstructive uropathy with urinary sepsis • Management • Sepsis Six • Analgesia – usually of Opiates; avoid NSAIDs • CT abd and pelvis with contrast – to confirm diagnosis
- 32. CT images of acute diverticulitis and (pericolic) diverticular abscesses • Diagnosis of Acute Sigmoid diverticulitis with perforation resulting pericolic collection • Hospital admission with continued IV Antibiotics ( Co-Amoxiclav 1.2 gm t.d.s ) • The collection ( pericolic abscess ) was drained percutaneously under radiological guidance( CT-guided drainage ) • Patient was discharged Day 4 with oral antibiotics • Review at Ambulatory Care on D7, repeated CT, resolution of the collection and removal of drain • FU Colorectal clinic 10 -12 weeks
- 33. What is Diverticular disease? • Consists of • Diverticulosis – colonic outpouching • Diverticulitis ( simple or complicated ) • Diverticular bleeding • Prevalence in left colon (95%) Around 75% of > 70 YO in Western world • Involvement of Sigmoid alone is 65%; entire colon – 7% • 75% of Diverticulosis remains asymptomatic 25% become symptomatic – pain, distension, altered bowel habit, diverticulitis and other complications Diverticula usually occur adjacent to the vasa recta, the small vessels that extend into the submucosa, the weakest areas of the colonic wall, usually occur on the mesenteric side of the colon.
- 34. • Diverticulitis is caused by mechanical obstruction of a (thin-walled) diverticulum compromising BS and render it to bacterial invasion/ infection and inflammation ( Simple Acute Diverticulitis ) • Complicated Diverticulitis - It can lead to perforation into the wall ( intramural abscess ), pericolic fat and mesentery ( pericolic abscess), or peritoneal cavity ( localised or generalised peritonitis ) • When inflammation and infection settle – fistula formation (colovesical, colovaginal, enterocolic, colocutaneous) occurs in 5% of cases • Healing and later fibrosis can cause stenosis of colon, or adhesion causing SBO • Bleeding: most common cause of Massive LGI bleeding ( 30-50% of cases ). The bleeding stops spontaneously in most cases (70 -80%)
- 35. • What causing Diverticular disease ( Aetiology )? • Refined Western diet low in dietary fibre • Altered collagen structure with aging • Disordered motility and increased luminal pressure especially in narrow sigmoid colon • The risks of diverticular complications • Red meat and high-fat diet • Smoking ( but not Caffeine and Alcohol ) • Obesity • Lack of exercise • NSAIDs – usage increase risk of perforation • Diverticular disease is rare in Africa and Asia where the diet is high in natural fibre
- 36. Management Asymptomatic diverculosis • Advise to high fibre diet containing whole grains, fruits and vegetables, increased gradually ( to minimize flatulence and bloating) and should be maintained for life • Adequate fluid intake • Most people with diverticulosis will remain asymptomatic, and no follow up or treatment is necessary Mild, uncomplicated diverticulitis can be managed at home • Prescribe broad-spectrum antibiotics to cover anaerobes and Gram-negative rods: • Suitable choices include co-amoxiclav or a combination of ciprofloxacin and metronidazole (if the person is allergic to penicillin ) for a week • Prescribe paracetamol for pain. • Recommend clear liquids only. Gradually reintroduce solid food as symptoms improve over 2–3 days. • Review within 48 hours, or sooner if symptoms deteriorate. Arrange admission if symptoms persist or deteriorate.
- 37. Surgical Management • Indications for Emergency Surgery • Purulent or faecal peritonitis (perforation) • Uncontrolled sepsis or failure to improve with conservative management • Laparotomy and Washout • Usually Hartmann’s procedure (Sigmoid resection with formation of end colostomy and closure of rectal stump) • Resection and primary anastomosis (+ Defunctioning ileostomy) • Mortality about 15% up to 50% in Faecal Peritonitis • Laparoscopy and Washout • Elective Sigmoid Resection • Younger patients • Less perform nowadays
- 39. Toxic Megacolon ( Acute Toxic Colitis ) • Toxic colitis with segmental or generalised dilatation of colon • Acute presentation with significant morbidity and mortality form inflammatory or infectious colitis • Diagnostic criteria • Radiological evidence of acute colitis • Any 3 of following – Fever > 38.6℃ , Tachycardia >120/min, WCC > 10.5, or anaemia • Any one of following – Dehydration, Altered mental status, Electrolyte abnormality, or Hypotension • Involvement of a Multidisciplinary team ( gastroenterologist, surgeon, critical care, anaesthetist ) • Operative treatment ( perforation, massive rectal bleeding, or lack of improvement after appropriate medical therapy for 72 hours )
- 40. Case history • #1 - A 30 YO man with a history of ulcerative colitis (UC) presents with severe abdominal pain and distention. He is currently being treated for an acute colitis flare characterised by 20 bloody bowel movements daily, fevers to 38.9°C (102°F), and left upper quadrant pain. P/E reveals tachycardia and hypotension. Abd examination shows distention with signs of focal peritonitis in the left lower quadrant • #2 - A 60 YO woman presents to the A&E department with a 4-day history of watery diarrhoea, fevers, and worsening abdominal pain. Her significant PMH includes sinusitis, for which she has been taking antibiotics for the past 3 weeks. On P/E, she is tachycardic and febrile, and her abdominal examination reveals diffuse abdominal tenderness and distention
- 41. Step-by-step Diagnostic approach, initial Treatment, and Investigations • H/o ongoing episodes of colitis symptoms associated with colitis ( diarrhoea – watery/bloody, fever, chills, crampy abd pain ) • h/o IBD, recent use of Abs and other medications s/a Opiates, anticholenergics, antidepressants, chemotherapy, steroids, or antimotility agents • P/E – Vital signs ( HR, BP, Temp, GCS, Urine OP ) • Abd – distention, decreased BS, tenderness, signs of peritonitis ( focal/local or diffuse ) • Atypical presentations ( no clear h/o e.g., C.Diff colitis no recent AB use/ no diarrhoea ) • Laboratory - FBC with differential, U&E, Serum Lactate, BC, Stool samples • Imaging – CT – AP – mandatory test in assessment of severity, CXR, AXR • Sigmoidoscopy and biopsy – in selective patients – to identify e.g., pseudomembranous colitis, IDB, or identify full-thickness necrosis Contraindicated in presence of peritonitis
- 42. Test Result FBC Raised WCC with left shift (Neutropenia in immunocompromised or severe sepsis) Low Hb abd reduced Hct Serum electrolytes Hypokalaemia, Hypomagnesia, deranged Renal functions Serum Albumin, CRP Hypoalbuminaemia, elevated CRP Serum Lactate May be elevated Stool studies ( for C&S, ova and parasite assay including C. Diff - NAAT (Nucleic acid amplification test) May be positive for infectious organism CT-AP Diffuse colonic wall thickening, submucosal oedema, pericolic fat stranding, colonic dilatation, absence of normal haustral marking CXR Free air under diaphragm indicates perforation AXR Massive dilated colon ( Colonic dilatation of >6cm in presence of systemic sepsis is suspicious of Toxic megacolon ) BC ( on admission and prn ) May be positive for pathogens
- 43. First choice – Vancomycin 500mg qid Second choice – Metronidazole 500 mg IVI tds + Vancomycin 500mg Enema Total colectomy with end-ileostomy • IV Ciclosporin and Infliximab have been utilised as Rescue Therapy when Corticosteroids fail to resolve severe colitis associated with IBD • Faecal microbial transplantation - a proven safe and effective treatment of recurrent or refractory Clostridium difficile colitis
- 44. A 22-year-old man presented with abdominal pain, passage of blood and mucus per rectum, abdominal distention, fever, and disorientation. Findings from sigmoidoscopy confirmed ulcerative colitis. Abdominal radiographs obtained 2 days apart show mucosal oedema and worsening of the distention in the transverse colon. The patient's clinical condition deteriorated over the next 36 hours despite steroid and antibiotic therapy, and the patient had to undergo a total colectomy and ileostomy The entire colon is distended, measuring up to 9 cm at the transverse colon and cecum with bowel wall oedema and surrounding fat stranding
- 45. What is your Diagnosis and Management? 72 YO female presented with 6-8 hrs h/o sudden onset severe, constant central abd pain which has been getting progressively worse • Feeling unwell, vomited several times • PMH – hypertension on ACEI, OA on opiates, ex- smokers 20 cigarettes/day for last 40 years • O/E – looks pale and unwell, irregular pulse 100/min, BP 104/62 mmHg, O2 Sat 94% on air, resp rate 26/min • Abd – very tender generally with no signs of guarding or peritonism, reduced BS • Bloods – Leucocytosis (WCC 16.5) , Lactate 5.5 mmol/L, Serum Amylase 267
- 46. Differential diagnosis • High index of suspicion for bowel ischaemia ( Acute mesenteric ischaemia ) • Any causes of acute abdomen – Acute pancreatitis, cholecystitis, diverticulitis, perforated viscus What are the appropriate investigations? • ECG • CT-AP with contrast – Radiological features of intestinal ischaemia ( thickened bowel wall, mural haematoma and gas, mesenteric vessel congestion, gas in the mesenteric or portal system (late signs) • Unclear diagnosis – CT Angiogram or Selective Angiography If CT imaging or angiography is not immediately available , urgent exploratory laparotomy is indicated in patients with suspected ischaemic bowel
- 47. CT –angiogram showed thromoembolus within proximal SMA - Underwent emergency laparotomy and thrombolectomy - the bowel was mostly viable, only requiring localized resection of non-viable SB with primary anastomosis.
- 48. Intestinal ischaemia can be classified into three broadly defined types: • Acute mesenteric ischaemia • Superior mesenteric artery embolus • Superior mesenteric artery thrombosis • Non-occlusive mesenteric ischaemia • Superior mesenteric vein thrombosis • Focal segmental ischaemia • Chronic mesenteric ischaemia • Colonic ischaemia • Reversible ischaemic colonopathy • Transient ulcerating ischaemic colitis • Chronic ulcerating ischaemic colitis • Colonic gangrene • Fulminant universal ischaemic colitis.
- 49. Comparison of symptoms/signs and investigations for the three types of ischaemic bowel disease
- 50. A large thrombus (blue arrow) is seen filing the right sided branches of the superior mesenteric vein. The bowel drained by these occluded branches is thick-walled and poorly enhancing (blue dotted line). Branches draining the more proximal small bowel remain patent (green arrow) and jejunal loops appear to have normal wall thickness (greed dotted line) ''Thumb-printing' is a radiologic sign indicating bowel-wall thickening due to oedema that is often a finding in patients with mesenteric ischemia
- 51. References • Bailey & Love’s Short Practice of Surgery, 27th Edition ( Norman Williams ) • Oxford Case Histories in General Surgery, 2018 • A Companion to Specialist Surgical Practice, Colorectal Surgery, Sixth Edition • Medscape (https://www.medscape.com/generalsurgery) • BMJ Best Practice (https://bestpractice.bmj.com/) • Radiopedia (https://radiopaedia.org/?lang=us) • Various Sources ( World Wide Web/ Internet )