ocular drug delivery
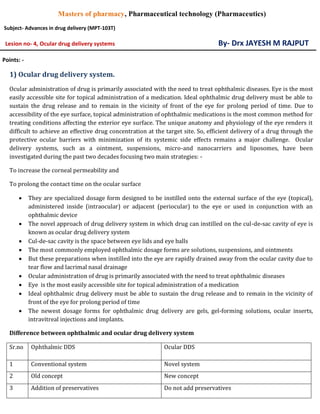
- 1. Masters of pharmacy, Pharmaceutical technology (Pharmaceutics) Subject- Advances in drug delivery (MPT-103T) Lesion no- 4, Ocular drug delivery systems By- Drx JAYESH M RAJPUT Points: - 1) Ocular drug delivery system. Ocular administration of drug is primarily associated with the need to treat ophthalmic diseases. Eye is the most easily accessible site for topical administration of a medication. Ideal ophthalmic drug delivery must be able to sustain the drug release and to remain in the vicinity of front of the eye for prolong period of time. Due to accessibility of the eye surface, topical administration of ophthalmic medications is the most common method for treating conditions affecting the exterior eye surface. The unique anatomy and physiology of the eye renders it difficult to achieve an effective drug concentration at the target site. So, efficient delivery of a drug through the protective ocular barriers with minimization of its systemic side effects remains a major challenge. Ocular delivery systems, such as a ointment, suspensions, micro-and nanocarriers and liposomes, have been investigated during the past two decades focusing two main strategies: - To increase the corneal permeability and To prolong the contact time on the ocular surface They are specialized dosage form designed to be instilled onto the external surface of the eye (topical), administered inside (intraocular) or adjacent (periocular) to the eye or used in conjunction with an ophthalmic device The novel approach of drug delivery system in which drug can instilled on the cul-de-sac cavity of eye is known as ocular drug delivery system Cul-de-sac cavity is the space between eye lids and eye balls The most commonly employed ophthalmic dosage forms are solutions, suspensions, and ointments But these preparations when instilled into the eye are rapidly drained away from the ocular cavity due to tear flow and lacrimal nasal drainage Ocular administration of drug is primarily associated with the need to treat ophthalmic diseases Eye is the most easily accessible site for topical administration of a medication Ideal ophthalmic drug delivery must be able to sustain the drug release and to remain in the vicinity of front of the eye for prolong period of time The newest dosage forms for ophthalmic drug delivery are gels, gel-forming solutions, ocular inserts, intravitreal injections and implants. Difference between ophthalmic and ocular drug delivery system Sr.no Ophthalmic DDS Ocular DDS 1 Conventional system Novel system 2 Old concept New concept 3 Addition of preservatives Do not add preservatives
- 2. 4 High dosing frequency Low dosing frequency 5 Minimum release rate of drug Maximum release rate of drug 6 Limited flexibility Extreme flexibility 7 Minimum absorption rate Maximum absorption rate 8 Minimum bioavailability Maximum bioavailability Major classes of drugs used are Miotics- e.g. Pilocarpine HCL Mydriatics- e.g. Atropine Cycloplegics- e.g. Atropine Anti-inflammatory- e.g. Corticosteroids Anti-infective (antibiotics, antiviral and antibacterial) Anti-glaucoma drugs- e.g. Pilocarpine HCL Surgical adjuncts- e.g. Irrigating solutions Diagnostic drugs-e.g. Sodium fluorescin Anesthetics- e.g. Tetracaine Composition of eye Water- 98% Solid-1.8% Organic elements Protein-0.67% Sugar-0.65% NaCL-0.66% Other mineral element- sodium, potassium and ammonia- 0.79% Artificial tear- the solution intended to rewet hard lenses in situ are referred has rewetting solutions or artificial tear. Lacrimal nasal drainage
- 3. Anatomy of the human eye Mechanism of ocular drug absorption Topically applied drug can be absorbed from, two routes: - Corneal absorption The outermost layer, the epithelium is the rate-limiting barrier Transcellular transport is the major mechanism of ocular absorption for lipophilic drugs Small ionic and hydrophilic molecules appear to gain access to the anterior chamber through paracellular pathway. Non-corneal absorption It involves penetration across the sclera and conjunctiva into the intraocular tissues This mechanism of absorption is usually non-productive, as drug penetrating is taken up by the local capillary beds and removed to the general circulation Significant for drug molecules with poor corneal permeability 2) Barriers of drug permeation Drug loss from the ocular surface: - after instillation, the flow of lacrimal fluid removes instilled compounds from the surface of the eye. Even though the lacrimal turnover rate is only about 1µl/min the excess volume of the instilled fluid is flown to the nasolacrimal duct rapidly in a couple of minutes Lacrimal fluid-eye barriers: - corneal epithelium limits drug absorption from the lacrimal fluid into the eye. The corneal epithelial cells form tight junctions that limit the paracellular drug permeation. Therefore, lipophilic drugs have typically atleast an order of magnitude higher permeability in the cornea than the hydrophilic drugs. In general, the conjunctiva is leakier epithelium than the cornea and its surface area is also nearly 20 times greater than that of the cornea. Blood-ocular barriers: - the eye is protected from the xenobiotics in the blood stream by blood ocular barriers. These barriers have two parts: blood-aqueous barrier and blood-retina barrier. The anterior blood-eye barrier is composed of the endothelial cells in the uvea. This barrier prevents the access of plasma albumin into the aqueous humour, and also limits the access of plasma albumin into the aqueous humor. The posterior barrier between blood stream and eye is comprised of retinal pigment epithelium (RPE) and the tight walls of retinal capillaries.
- 4. Or Barriers are broadly classified as: - 1) Anatomical barriers When a dosage form is topically administered there are two routes of entry, either through the cornea or via the non-corneal route. The cornea is very tight multilayered tissue that is mainly composed of five sections Epithelium, bowman’s membrane, stroma, descent’s membrane and endothelium. Corneal cross section Out of these it is the epithelium which acts as the principal barrier. These 5-6 layers of columnar epithelial cells with very tight junctions create high Para cellular resistance of 12-16 KΩ.cm. it acts as a major barrier to hydrophilic drug transport through intercellular spaces. On the other hand stroma, which consists of multiple layers of hexagonally, arranged collagen fibers containing aqueous pores or channels allow hydrophilic drugs to easily pass through but it acts as a significant barrier for lipophilic drugs. Thus for a drug to have optimum bioavailability, it should have the right balance between lipophilicity and hydrophilicity. The remaining layers are leaky and do not act as significant barriers. Non-corneal route by passes the cornea and involves movement across conjunctiva and sclera. This route is important for large especially and hydrophilic molecules such as peptides, proteins and siRNA (small or short interfering RNA). The conjunctiva is more permeable than cornea especially for hydrophilic molecules due to much lower expression of tight junction proteins relative to corneal epithelium. High vascularity of the limbal area renders this route not suitable for drug delivery as the blood vessels remove a large fraction of absorbed dose. Only a small fration of the dose reaches the vitreous. 2) Physiological barriers o The eye’s primary line of defense is its tear film o Bioavailability of topical administered drugs is further reduced by precorneal factors such as solution drainage, tears dilution, tear turnover, and increased lacrimation. o The lacrimal fluid is an isotonic aqueous solution containing a mixture of proteins (such as lysozyme) as well as lipids o Following topical application, lacrimation is significantly increased leading to dilution of administered dose o This in turn lowers drug concentration leading to diminished drug absorption o Rapid clearance from the precorneal area by lacrimation and through nasolacrimal drainage and spillage further reduces contact time between the tissue and drug molecules o This in turn lowers the exact time for absorption leading to reduced bioavailability
- 5. o The average tear volume is 7-9 µL with a turnover rate of 16% per minute o Thus drugs administered as eye drops need to be isotonic and non irritating to prevent significant precorneal loss 3) Blood-ocular barrier o The blood-ocular barrier normally keeps most drugs out of the eye. However inflammation breaks down this barrier allowing drugs and large molecules to penetrate into the eye 4) Blood- aqueous barrier o The ciliary epithelium and capillaries of the iris 5) Blood- retinal barrier o Non-fenestrated capillaries of the retinal circulation and the tight junctions between retinal epithelial cells preventing passage of large molecules from chorio-capillaries into the retina Drug and dosage form related factors: - The physicochemical properties of drug molecule become even more important in the case of ocular drug delivery because of the complex anatomical and physiological constrains The rate of absorption from the administered site depends highly on the physical properties of drug molecule (solubility, lipophilicity, degree of ionization and molecular weight) and ocular tissue structure Solubility: - solubility is dependent on the pKa of the drug and pH of the solution. With these parameters one can determine the ratio of ionized to unionized molecules Usually unionized molecules can readily permeate biological membranes example: - the permeability of unionized Pilocarpine is almost two fold greater than that of its ionized form.
- 6. The corneal epithelium bears a negative charge at the pH of lachrymal fluid and hence cationic species tend to penetrate at a faster ratio their anionic counterparts. Lipophilicity: - lipophilicity and corneal permeability display sigmoidal relationship This is because of the diffential permeability of the different layers of cornea towards lipophilic drugs. As previously mentioned, lipophilic drug tend to permeate easily through the epithelial layers of cornea But the hydrophilicity of the inner layer of cornea (stroma) requires higher hydrophilicity for optimal permeation Partition coefficient (Log P) value ranging from 2-4 is found to result in optimum corneal permeation. Molecular weight and size: - the weight and size of a molecules play a critical role in deciding its overall permeability through paracellular route The diameter of the tight junctions present on corneal epithelium is less than 2 nm Molecules having molecular weight less than 500 Dalton are able to permeate readily The paracellular permeability is further limited by the pore density of corneal epithelium. Molecular weight and size The conjunctiva has larger paracellular pore diameter thus allowing permeation of larger molecules such as small and medium size peptides (5000-10000 Daltons) Permeation across sclera occurs through the aqueous pores and molecular size of the solute can be the determining factor Example: - sucrose (molecular weight- 342 Daltons) permeates 16 times faster than inulin (molecular weight 5000 Daltons) Sclera permeability is approximately half of conjunctiva but much higher than cornea. 3) Methods to overcome barriers I. Viscosity enhancers Viscosity increasing polymers are usually added to ophthalmic drug solutions on the premise that an increased vehicle viscosity should correspond to a slower elimination from the preocular area, which lead to improved precorneal residence time and hence a greater transcorneal penetration of the drug into the anterior chamber The polymers used include polyvinyl alcohol (PVA), polyvinyl pyrrolidone (PVP), methylcellulose (MC), hydroxyl ethyl cellulose, hydroxyl propyl methyl cellulose (HPMC), and hydroxyl propyl cellulose. II. Penetration enhancers The transport characteristics across the cornea can be maximized by increasing the permeability of the corneal epithelial membrane So, one of the approaches used to improve ophthalmic drug bioavailability lies in increasing transiently the permeability characteristics of the cornea with appropriate substances known as penetration enhancers or absorption promoters It has disadvantages like ocular irritation and toxicity. The transport process from the cornea to the receptor site is a rate-limiting step, and permeation enhancers increase corneal uptake by modifying the integrity of the corneal epithelium E.g., cetyl pyridinium chloride, benzalkonium chloride, parabens, tween 20, saponins
- 7. Classified as:- Calcium chelators, surfactants, bile acid and salts, preservative, glycoside, fatty acids III. Eye ointments The medical agent is added to the base either as a solution or as a finely micronized powder Upon instillation in the eye, ointments break up into the small droplets and remain as a depot of drug in the cul-de-sac for extended periods Ointments are therefore useful in improving drug bioavailability and in sustaining drug release Although safe and well-tolerated by the eye, ointments suffer with relatively poor patient compliance due to blurring of vision and occasional irritation. IV. Gel It has advantage like reduced systemic exposure. Despite the extremely high viscosity, gel achieves only a limited improvement in bioavailability, and the dosing frequency can be decreased to once a day at most The high viscosity, however, results in blurred vision and matted eyelids which substantially reduce patient acceptability The aqueous gel typically utilizes such polymers as PVA, polyacrylamide, poloxamer, HPMC, carbomer, poly methyl vinyl ether maleic anhydride, and hydroxyl propyl ethyl cellulose The release of a drug from these systems occurs via the transport of the solvent into the polymer matrix, leading to its swelling. The final step involves the diffusion of the solute through the swollen polymer, leading to erosion/dissolution V. Liposomes Liposomes are the microscopic vesicles composed of one or more concentric lipid bilayers, separated by water or aqueous buffer compartments Liposomes possess the ability to have an intimate contact with the corneal and conjunctival surfaces, which increases the probability of ocular drug absorption This ability is especially provides the sustained release and site specific delivery. Liposomes are difficult to manufacture in sterile preparation It has limitation like low drug load and inadequate aqueous stability and is undesirable for drugs that are poorly absorbed, the drugs with low partition coefficient. VI. Niosomes Niosomes are bilayered structural vesicles made up of non-ionic surfactant which are capable of encapsulating both lipophilic and hydrophilic compounds Niosomes reduce the systemic drainage and improve the residence time, which leads to increase ocular bioavailability They are non biodegradable and non biocompatible in nature. VII. Nanoparticles/ Nanospheres These are polymeric colloidal particles, ranging from 10 nm to 1 mm, in which the drug is dissolved, entrapped, encapsulated, or adsorbed Encapsulation of the drug leads to stabilization of the drug. They represent promising drug carriers for ophthalmic application They are further classified into nanospheres (small capsules with a central cavity surrounded by a polymeric membrane) or nanocapsules (solid matricial spheres) VIII. Microemulsion
- 8. Microemulsion is stable dispersions of water and oil, facilitated by a combination of surfactant and co- surfactant in a manner to reduce interfacial tension Microemulsion improves the ocular bioavailability of the drug and reduces frequency of the administration These systems are usually characterized by higher thermodynamic stability, small droplet size (῀100 nm), and clear appearance IX. In situ-forming gel The droppable gels are liquid upon instillation, and they undergo a phase transition in the ocular cul-de- sac to form a viscoelastic gel, and this provides a response to environmental changes It improves the patient acceptance. It prolongs the residence time and improves the ocular bioavailability of the drug Parameters that can change and trigger the phase transition of droppable gels include pH, temperature, and ionic strength Examples of potential ophthalmic droppable gels reported in the literature include gelling triggered by a change in pH- CAP latex cross linked polyacrylic acid and derivatives such as carbomers and polycarbophil, gelling triggered by temperature change- poloxamers methyl cellulose and smart hydrogel, gelling triggered by ionic strength change- gelrite and alginate. X. Ocular inserts The ocular inserts overcome this disadvantage by providing with more controlled, sustained and continuous drug delivery by maintaining an effective drug concentration in the target tissues and yet minimizing the number of applications It reduces systemic adsorption of the drug. It causes accurate dosing of the drug It has disadvantages like patient incompliance, difficulty with self-insertion, foreign body sensation, and inadvertent loss from the eye.
- 9. XI. Implants The goal of the intraocular implant design is to provide prolonged activity with controlled drug release from the polymeric implant material Intraocular administration of the implants always requires minor surgery. In general, they are placed intravitrally, at the pars plana of the eye (posterior to the lens and anterior to the retina) Although this is an invasive technique, the implants have the benefit of: - By-passing the blood-ocular barriers to deliver constant therapeutic levels of drug directly to the site of action Avoidance of the side effects associated with frequent systemic and intravitreal injections, and Smaller quantity of drug needed during the treatment The ocular implants are classified as non biodegradable devices. Non-biodegradable implants can provide more accurate control of drug release and longer release periods that the biodegradable polymers do, but the non biodegradable systems require surgical implant removal with the associated risks XII. Iontophoresis Ocular Iontophoresis has gained significant interest recently due to its non invasive nature of delivery to both anterior and posterior segment Iontophoresis is a non invasive method of transferring ionized drugs through membranes with low electrical current The drugs are moved across the membranes by two mechanisms: migration and electro-osmosis, ocular Iontophoresis is classified into transcorneal, corneosceral, or trans-scleral Iontophoresis It has ability to modulate dosages (less risk of toxicity), a broad applicability to deliver a broad range of drugs or genes to treat several ophthalmic diseases in the posterior segment of the eye, and good acceptance by patients. It may combined with other drug delivery systems It has disadvantage like no sustained half-life, requires repeated administrations, side effects include mild pain in some cases, but no risk of infections or ulcerations, risk of low patient compliance because the frequent administrations that may be needed Ocuphor™ system has been designed with an applicator, dispersive electrode, and a dose controller for transscleral Iontophoresis (DDT), this device releases the active drug into retina-choroid as well A similar device has been designed called visulex ™ to allow selective transport of ionized molecules through sclera Examples of antibiotics successfully employed are gentamicin, tobramycin, and ciprofloxacin, but not vancomycin because of its high molecular weight
- 10. Approaches for the enhancement of ocular bioavailability Based on the use of the drug delivery system, which provide the controlled and continuous delivery of opthalmic drugs. Based on maximizing corneal drug absorption and minimizing precorneal drug loss, these are summarized as: - Approach Advantages Limitations Penetration enhancers Ease of formulation due to compatibility with wide range of excipients Accumulation in cornea affecting clear Vision. Alteration of permeability of Blood vessels in the uveal tract. Irritation of eye and nasal mucosa. Suspension Retention in lower cul-de-sac for prolonged period Non-uniformity of dosing formulation Of non-dispersible cake. Polymorphic Changes of drug. Ointments Retention in lower cul-de-sac for prolonged period, slower diffusion of drug Blurred vision Non esthetic Gels Retention in lower cul-de-sac for prolonged period, slower diffusion of drug Difficulty in administration Blurred vision Mucoadhesive dosage forms Retention in lower cul-de-sac for prolonged period Poor compliance Blurred vision Liposomes Biodegradable, non-toxic, available in more than one dosage form Limited stability, limited drug loading Capacity, expensive. Niosomes Non-toxic Available in more than one dosage Form Limited stability, limited drug loading Capacity, expensive Micro and Nanoparticles Enhance bioavailability, available in More than one dosage forms, Retention in lower cul-de-sac for Prolonged period Suitability for only small dose drugs, difficulty in formulation, expensive Micro emulsion Enhanced patient compliance, best of Drugs with slow dissolution, good Stability Rapid precorneal elimination Ocular inserts Controlled rate of release, prolonged Delivery Irritation, need of skilled personnel for Administration, abrasion of cornea, expensive Contact lenses Correction of vision, sustained Delivery of drugs Low precision of dosing, expensive Iontophoresis Fast delivery, painless and safe drug delivery system, delivery at the desired ocular tissue, increased ocular retention time Difficulty in insertion, patient non-compliance
- 11. Formulation considerations in ophthalmics A. Sterility Probably the most important property of ophthalmic formulations is that they must be sterile. The USP XXII-NF xvII (2003) lists five methods of achieving sterility: - Steam sterilization at 121 degree, dry-heat sterilization, gas sterilization using ethylene oxide (due to environmental concerns the use of ethylene oxide is being phased out wherever possible), sterilization using ionizing radiation e.g., radioisotope decay (gamma radiation) and electron beam radiation, sterilization by filtration. B. Preservatives The selection of a preservative for ophthalmic solutions is not an easy task, with very few candidates to choose from: - Sr no Preservatives Conc. range 1 Quaternary ammonium compounds 0.004-0.02 2 Organic mercurial’s 0.01- most common 3 Parahydroxy benzoates 0.001- 0.01 4 Chlorobutanol 0.5 The following criteria are important for selection of preservative: - Bard spectrum of activity against both gram-positive and gram-negative organisms and fungi The agent should rapidly kill virulent organisms Satisfactory chemical and physical stability over a wide range of pH and temperature Compatibility with formulation components and container materials Non-toxic and non-irritating during use C. Clarity o The official definition of ophthalmic solutions requires that they be free of particulate matter o Solution clarity is usually achieved by filtration, either with a clarifying filter or as part of a sterile filtration procedure o The degree of clarity of the finished product can be monitored by means of various instruments capable of detecting any light scattering or blockage resulting from the presence of particulate matter. Sr no Particle size (µm) Proposed limit (particles per ml) 1 ≥10 ≤50 2 ≥25 ≤5 3 ˃50 Not allowed
- 12. D. Stability The stability of the active ingredient in an ophthalmic solution depends upon the chemical nature of the active ingredient, pH manufacturing procedure, type of additives, and type of container. The maintenance of a pH that is consistent with acceptable stability is often in conflict with a pH that would provide optimum corneal penetration of the drug in question and optimum patient acceptance of the product. E. pH adjustment and buffers o the adjustment of ophthalmic solution pH by the appropriate choice of a buffer is one of the most important formulation considerations o buffers may be used in an ophthalmic solution for one or more of the following reasons; to maintain the physiologic pH of the tears upon administration of formulation in order to minimize tearing and patient discomfort, to optimize the therapeutic activity of the active ingredient by altering the corneal penetration through changes in the degree of ionization; and to optimize product stability o the tear fluid pH is reported to be vary between 6.9 and 7.5 F. Tonicity o The hypertonic solution placed in the eye tends to draw solvent (water) from its surroundings in order to dilute the instilled solution o In this case, water flows from the aqueous layer through the cornea to the eye surface o Conversely, a hypotonic solution could result in the passage of water from the site of application through the eye tissues o In this case, the epithelial permeability is increased; allowing water to flow into the cornea, the corneal tissues swells, and drug concentration on the ocular surface is temporarily increased. G. Viscosity modifiers o The viscosity of ophthalmic solutions is often increase in order to prolong the corneal contact time, decrease the drainage rate, and increase the bioavailability of the active ingredient o The polymers used to increase viscosity may also lower the frictional resistance between the cornea and the eyelid which occurs with each blink, thereby exerting a lubricating effect that may be of benefit for some patients. H. Additives o Stabilizers o The use of stabilizers is permitted in ophthalmic solutions when necessary. Epinephrine hydrochloride undergoes oxidative degradation and an oxidant such as sodium bisulphate or metabisulfite is commonly added up to a 0.3% concentration. Epinephrine borate stabilization requires special consideration, and mixtures of ascorbic acid and acetyl-cysteine or sodium bisulphite and 8-hydroxyquinoline have been used for this purpose o Surfactant o The addition of surfactants to ophthalmic solutions is permitted; even through their use is greatly restricted. The toxicity of surfactants is on the order: Anionic ˃ cationic ˃ non-ionic Non-Ionics are used in low concentration to increase the dispersion of suspended drugs, such as steroids, and thereby improve solution clarity. The ability of these compounds to bind and thereby inactivate certain preservatives coupled with their irrational potentials, limits their use to low concentrations. _______________________________________THE END_________________________________________
