GIT BLEEDING.pdf
- 2. GI Bleeding • Clinical Presentation • Acute Upper GI Bleed • Acute Lower GI Bleed
- 3. Core Principles in GI Bleeding Management • Assessment and stabilization of hemodynamic status • Determine the source of bleeding • Stop active bleeding • Treatment of underlying abnormality • Prevent recurrent bleeding
- 4. GI Bleeding Management Definitions Hematemesis: bloody vomitus (bright red or coffee-grounds) Melena: black, tarry, foul-smelling stool Hematochezia: bright red or maroon blood per rectum Occult: positive stool occult test Symptoms of anemia: angina, dyspnea, or lightheadedness
- 5. GI Bleeding Management Patient Assessment • Hemodynamic status • Localization of bleeding source • CBC, PT, and T & C • Risk factors – Prior h/o PUD or bleeding – Cirrhosis – Coagulopathy – ASA or NSAID’s
- 6. GI Bleeding Management Initial Patient Assessment Vital Signs Blood Loss Severity of GI Bleed Shock (resting hypotension) 20-25% Massive Postural (orthostatic hypotension) 10-20% Moderate Normal <10% Minor
- 7. GI Bleeding Management Resuscitation • 2 large bore peripheral IV’s • Normal saline or LR • Packed RBCs • Correct coagulopathy
- 8. GI Bleeding Management Location of Bleeding • Upper – Proximal to Ligament of Treitz – Melena (100-200 cc of blood) – Azotemia – Nasogastric aspirate • Lower – Distal to Ligament of Treitz – Hematochezia
- 9. Acute UGIB Demographics • Over 400,000 admissions annually • 80% self-limited • Mortality 10-14% • Continued or recurrent bleeding - mortality 30- 40% • Nonvariceal UGIB w/o complication* – Mean LOS 2.7 days, $3402 (2008 $) • Nonvariceal UGIB with complication* – Mean LOS 4.4 days, $5632 (2008 $) Adam V, Barkun A. Value Health. 2008;11:1-3.
- 12. UGIB Risk Stratification – AIMS65 • Albumin < 3.0 g/dL, • INR > 1.5, • Altered mental status, • Systolic blood pressure 90 mm Hg or lower, and • Age older > 65 years. Saltzman JR et al. Gastrointest Endosc 2011:1215-22. • Large clinical database - CareFusion • 187 US hospitals • Recursive partitioning • 2004-5 29,222 pts to derive risk score • 2006-7 32,504 pts to validate
- 13. UGIB Risk Stratification – AIMS65 Saltzman JR et al. Gastrointest Endosc 2011:1215-22.
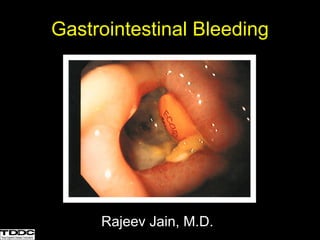
- 14. • Peptic ulcer disease – Gastric ulcer – Duodenal ulcer • Mallory-Weiss tear • Varices • Esophagitis • Dieulafoy’s lesion • Vascular anomalies • Malignancy • Post-procedural • Cameron’s lesions • Hemobilia • Hemorrhagic gastropathy • Aortoenteric fistula Acute UGIB Differential Diagnosis Major Causes Minor Causes
- 15. Peptic Ulcer Disease Forrest Class Stigmata IA Arterial spurting IB Arterial oozing IIA Visible vessel IIB Adherent clot IIC Pigmented flat spot III Clean based Forrest JA, Finlayson ND, Shearman DJ: Endoscopy in gastrointestinal bleeding. Lancet 1974; 2:394-7
- 16. Endoscopic Appearance of Ulcers Clean based ulcer Nonbleeding visible vessel
- 18. Prognostic Features at Endoscopy in Acute Ulcer Bleeding
- 19. • Thermal – Bipolar probe – Monopolar probe – Argon plasma coagulator – Heater probe • Mechanical – Hemoclips – Band ligation • Injection – Epinephrine – Alcohol – Ethanolamine – Polidocal Endoscopic Therapy of PUD
- 20. Endoscopic Therapy of PUD Laine and Peterson New Eng J Med 1994;331:717-27.
- 21. Risk of Recurrent Bleeding after Endoscopic Therapy
- 22. Effect of Proton-Pump Inhibition on Peptic Ulcer Bleeding Gralnek et al. New Eng J Med 2008;359:928-37.
- 23. Management of PUD after EGD in High Risk Pts • Proton-pump inhibitor 80 mg IV bolus dose plus continuous infusion for 72 hrs • Admit to monitored bed or ICU setting • Initiate oral intake of clear liquid diet 6 hrs after EGD in pts with hemodynamic stability • Transition to oral PPI after completing IV course • Perform testing for H. pylori infection • For selected patients, discuss need for NSAIDs and antiplatelet therapy Gralnek et al. New Eng J Med 2008;359:928-37.
- 24. Management of PUD after EGD in Low Risk Pts • Oral proton-pump inhibitor • Initiate oral intake with a regular diet 6 hrs after EGD in pts with hemodynamic stability • Perform testing for H. pylori infection • For selected patients, discuss need for NSAIDs and antiplatelet therapy • Consider early discharge in selected pts Gralnek et al. New Eng J Med 2008;359:928-37.
- 27. Management of Acute Variceal Bleeding Suspected Variceal Bleeding Endoscopy Band ligation or sclerotherapy Continue Octreotide for 5 days Early rebleeding Failure to control TIPS or surgery Octreotide 50 ug bolus, 50 ug/hr Conservative blood volume resuscitation Antibiotics
- 28. Antibiotic Prophylaxis in GI Bleeding in Cirrhotic Patients • Fluoroquinolones or amoxicillin + clavulinic acid • Meta-analysis 1 – Decrease rates of infection • SBP, bacteremia – Increased short-term survival • RCT 2 – Reduction in early rebleeding 1.Bernard et al.Hepatology. 29(6):1655-61.1999. 2.Hou et al. Hepatology. 39(3):746-53.2004.
- 30. Transjugular Intrahepatic Portosystemic Shunt (TIPS) IVC Portal Vein Splenic Vein Coronary Vein
- 31. Aortoduodenal Fistula The picture can't be displayed. The picture can't be displayed. The picture can't be displayed. The picture can't be displayed. Aorta Duodenum Graft Fistula
- 32. Acute UGIB Surgery • Recurrent bleeding despite endoscopic therapy • > 6-8 units pRBCs
- 33. Management of Ulcer Bleeding: ACG Guidelines Initial Assessment and Risk Stratification • Hemodynamic status should be assessed immediately upon presentation and resuscitative measures begun as needed (Strong recommendation). • Blood transfusions should target Hgb ≥ 7 g / dl, with higher Hgbs targeted in patients with clinical evidence of intravascular volume depletion or comorbidities, such as coronary artery disease (Conditional recommendation). • Risk assessment should be performed to stratify patients into higher and lower risk categories and may assist in initial decisions such as timing of endoscopy, time of discharge, and level of care (Conditional recommendation). • Discharge from the ED without inpatient endoscopy may be considered in patients with urea nitrogen < 18.2 mg / dl; Hgb ≥ 13.0 g / dl for men (12.0 g / dl for women), systolic blood pressure ≥ 110 mm Hg; pulse < 100 beats / min; and absence of melena, syncope, cardiac failure, and liver disease, as they have < 1 % chance of requiring intervention (Conditional recommendation). Laine & Jensen Am J Gastroenterol 2012; 107:345–360
- 34. Management of Ulcer Bleeding: ACG Guidelines Pre-endoscopic interventions • Intravenous infusion of erythromycin (250 mg ~ 30 min before endoscopy) should be considered to improve diagnostic yield and decrease the need for repeat endoscopy. However, erythromycin has not consistently been shown to improve clinical outcomes (Conditional recommendation). • Pre-endoscopic intravenous PPI (e.g., 80 mg bolus followed by 8 mg / h infusion) may be considered to decrease the proportion of patients who have higher risk stigmata of hemorrhage at endoscopy and who receive endoscopic therapy. However, PPIs do not improve clinical outcomes such as further bleeding, surgery, or death (Conditional recommendation). • If endoscopy will be delayed or cannot be performed, intravenous PPI is recommended to reduce further bleeding (Conditional recommendation). • Nasogastric or orogastric lavage is not required in patients with UGIB for diagnosis, prognosis, visualization, or therapeutic effect (Conditional recommendation). Laine & Jensen Am J Gastroenterol 2012; 107:345–360
- 35. Management of Ulcer Bleeding: ACG Guidelines Timing of endoscopy • Patients with UGIB should generally undergo endoscopy within 24 h of admission, following resuscitative efforts to optimize hemodynamic parameters and other medical problems (Conditional recommendation). • In patients who are hemodynamically stable and without serious comorbidities endoscopy should be performed as soon as possible in a non-emergent setting to identify the substantial proportion of patients with low-risk endoscopic findings who can be safely discharged (Conditional recommendation). • In patients with higher risk clinical features (e.g., tachycardia, hypotension, bloody emesis or nasogastric aspirate in hospital) endoscopy within 12 h may be considered to potentially improve clinical outcomes (Conditional recommendation). Laine & Jensen Am J Gastroenterol 2012; 107:345–360
- 36. Management of Ulcer Bleeding: ACG Guidelines - Endoscopy • Stigmata of recent hemorrhage should be recorded as they predict risk of further bleeding and guide management decisions. The stigmata, in descending risk of further bleeding, are active spurting, non-bleeding visible vessel, active oozing, adherent clot, fl at pigmented spot, and clean base (Strong recommendation). • Endoscopic therapy should be provided to patients with active spurting or oozing bleeding or a non-bleeding visible vessel (Strong recommendation). • Endoscopic therapy may be considered for patients with an adherent clot resistant to vigorous irrigation. Benefi t may be greater in patients with clinical features potentially associated with a higher risk of rebleeding (e.g., older age, concurrent illness, inpatient at time bleeding began) (Conditional recommendation). • Endoscopic therapy should not be provided to patients who have an ulcer with a clean base or a fl at pigmented spot (Strong recommendation). Laine & Jensen Am J Gastroenterol 2012; 107:345–360
- 37. Management of Ulcer Bleeding: ACG Guidelines - Endoscopy • Epinephrine therapy should not be used alone. If used, it should be combined with a second modality (Strong recommendation). • Thermal therapy with bipolar electrocoagulation or heater probe and injection of sclerosant (e.g., absolute alcohol) are recommended because they reduce further bleeding, need for surgery, and mortality (Strong recommendation). • Clips are recommended because they appear to decrease further bleeding and need for surgery. However, comparisons of clips vs. other therapies yield variable results and currently used clips have not been well studied (Conditional recommendation). • For the subset of patients with actively bleeding ulcers, thermal therapy or epinephrine plus a second modality may be preferred over clips or sclerosant alone to achieve initial hemostasis (Conditional recommendation). Laine & Jensen Am J Gastroenterol 2012; 107:345–360
- 38. Management of Ulcer Bleeding: ACG Guidelines - Therapy after initial endoscopy • After successful endoscopic hemostasis, intravenous PPI therapy with 80 mg bolus followed by 8 mg/h continuous infusion for 72 h should be given to patients who have an ulcer with active bleeding, a non-bleeding visible vessel, or an adherent clot (Strong recommendation). • Patients with ulcers that have flat pigmented spots or clean bases can receive standard PPI therapy (e.g., oral PPI once daily) (Strong recommendation). • Routine second-look endoscopy, in which repeat endoscopy is performed 24 h after initial endoscopic hemostatic therapy, is not recommended (Conditional recommendation). • Repeat endoscopy should be performed in patients with clinical evidence of recurrent bleeding and hemostatic therapy should be applied in those with higher risk stigmata of hemorrhage (Strong recommendation). • If further bleeding occurs after a second endoscopic therapeutic session, surgery or interventional radiology with transcathether arterial embolization is generally employed (Conditional recommendation). Laine & Jensen Am J Gastroenterol 2012; 107:345–360
- 39. International Consensus on Nonvariceal Upper Gastrointestinal Bleeding: Postdischarge ASA and NSAIDs • In patients with previous ulcer bleeding who require an NSAID, it should be recognized that treatment with a traditional NSAID plus PPI or a COX-2 inhibitor alone is still associated with a clinically important risk for recurrent ulcer bleeding. • In patients with previous ulcer bleeding who require an NSAID, the combination of a PPI and a COX-2 inhibitor is recommended to reduce the risk for recurrent bleeding from that of COX-2 inhibitors alone. Barkun AN, et al. Ann Intern Med. 2010;152:101-113.
- 40. International Consensus on Nonvariceal Upper Gastrointestinal Bleeding: Postdischarge ASA and NSAIDs • In patients who receive low-dose ASA and develop acute ulcer bleeding, ASA therapy should be restarted as soon as the risk for cardiovascular complication is thought to outweigh the risk for bleeding. • In patients with previous ulcer bleeding who require cardiovascular prophylaxis, it should be recognized that clopidogrel alone has a higher risk for rebleeding than ASA combined with a PPI. Barkun AN, et al. Ann Intern Med. 2010;152:101-113.
- 41. • Diverticulosis • Colitis – IBD (UC>>CD) – Ischemia – Infection • Vascular anomalies • Neoplasia • Anorectal – Hemorrhoids – Fissure • Dieulafoy’s lesion • Varices – Small bowel – Rectal • Aortoenteric fistula • Kaposi’s sarcoma • UPPER GI BLEED Acute LGIB Differential Diagnosis
- 42. DIAGNOSES % OF TOTAL Diverticulosis 40 Vascular anomalies 30 Colitis 21 Neoplasia 14 Anorectal 10 Upper GI sites 10 Acute LGIB Diagnoses in pts with hemodynamic compromise. Zuccaro. ASGE Clinical Update. 1999.
- 43. Diverticulosis
- 45. Hemorrhoids
- 46. Bleeding AVM
- 48. • Incidence 0.3 - 3.0 % • Etiology Incomplete obliteration of the vitelline duct. • Pathology 50% ileal, 50% gastric, pancreatic, colonic mucosa • Complications – Painless bleeding (children, currant jelly) – Intussusception Acute LGIB Meckel’s Diverticulum
- 49. Study Yield % Comments Colonoscopy 69-80 Therapeutic Arteriography 40-78 1 ml/min, risks Tagged RBC Scan 20-72 Localization Acute LGIB Evaluation Zuccaro. ASGE Clinical Update. 1999.
- 50. • Resuscitation • UGI source • Most bleeding ceases • Colonoscopy • No role for barium studies Acute LGIB Key Points
- 51. SUMMARY GI Bleeding Management • Assessment and stabilization of hemodynamic status • Determine the source of bleeding • Stop active bleeding • Treatment of underlying abnormality • Prevent recurrent bleeding