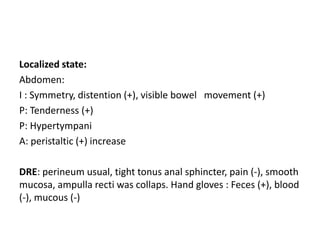
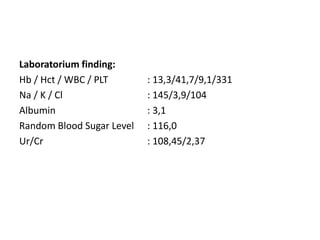
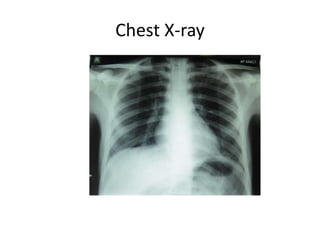
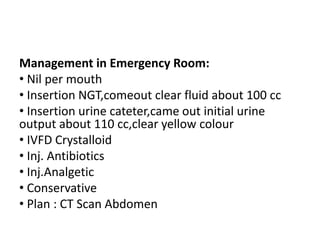
The patient presented with inability to defecate for 7 days, abdominal pain, fever, vomiting, weight loss, and cough with green sputum for a month. On examination, the patient had a fever, abdominal distension and tenderness, increased bowel sounds, and tight anal sphincter tone with collapsed rectal ampulla. Laboratory findings were notable for anemia. The working diagnosis was partial mechanical bowel obstruction possibly due to peritoneal tuberculosis based on the history and physical exam. The patient received NG tube decompression, IV fluids, antibiotics, analgesics, and was planned for CT scan of the abdomen.