Documentation Electronic Health Record· DocumentationVitals
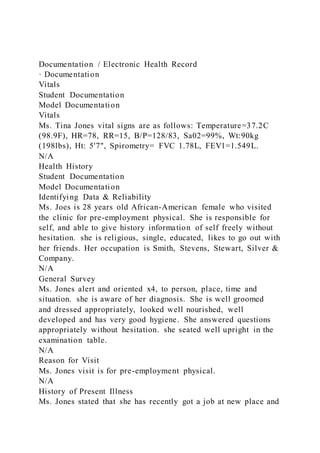
- 1. Documentation / Electronic Health Record · Documentation Vitals Student Documentation Model Documentation Vitals Ms. Tina Jones vital signs are as follows: Temperature=37.2C (98.9F), HR=78, RR=15, B/P=128/83, Sa02=99%, Wt:90kg (198lbs), Ht: 5'7", Spirometry= FVC 1.78L, FEV1=1.549L. N/A Health History Student Documentation Model Documentation Identifying Data & Reliability Ms. Joes is 28 years old African-American female who visited the clinic for pre-employment physical. She is responsible for self, and able to give history information of self freely without hesitation. she is religious, single, educated, likes to go out with her friends. Her occupation is Smith, Stevens, Stewart, Silver & Company. N/A General Survey Ms. Jones alert and oriented x4, to person, place, time and situation. she is aware of her diagnosis. She is well groomed and dressed appropriately, looked well nourished, well developed and has very good hygiene. She answered questions appropriately without hesitation. she seated well upright in the examination table. N/A Reason for Visit Ms. Jones visit is for pre-employment physical. N/A History of Present Illness Ms. Jones stated that she has recently got a job at new place and
- 2. she is supposed to provide a physical examination. Ms. Jones did not voice any acute concerns. The gynecologist diagnosed her with polycystic ovary syndrome (PCOS). She was prescribed oral contraceptives that helped improve her acne. She has history of diabetes and asthma. And she stated that she has modified her lifestyle habit. N/A Medications Metformin 850 mg PO BID, Flovent 110 mcg/spray, albuterol 90 mcg/spray MDI 1 to 3 puffs every 4 hours as needed. Tylenol 500 to 1000 mg PO PRN for headaches, ibuprofen 600 mg PO TID PRN for menstrual cramps. N/A Allergies Ms. Jones is allergic to penicillin (PNC), cats, dust. Denies food and latex allergies. N/A Medical History Ms. Jones was diagnosed with asthmas when she was 2 and half years old, and the she had asthma attack 3 months ago. She was diagnosed with diabetes when she was 24 years of age. she was diagnosed with PCOS 4 months ago, and N/A Health Maintenance She had pap smears 4 months ago, had eye examination 3 months ago, had dental checkup 5 months ago. Abide by the car seat belt by putting seat on while driving. She uses sun screen to prevent sun burnt, PPD was done 2 years ago and it was negative. N/A Family History Ms. Jones stated that her maternal grand-mother died of stroke, history of hypertension and high cholesterol, at age 75. Maternal grand-father died of stroke, hypertension and high cholesterol at age of 78. Paternal grand-father died of colon cancer at age 65, also had type 2 diabetes. Paternal uncle died
- 3. suddenly of cancer, kidney disease, sickle cell anemia and thyroid problems. Paternal grand-mother is 82 years old and still living, and she has hypertension. N/A Social History Ms. Jones is currently living with her mother and her sister, but had lived independently since she was 19 years old. She will be moving to her own place in one month. she will be starting her new job in two weeks’ time at Smith, Stevens, Stewart, Silver, & Company. She and her friends started a book club and read one book each month. She goes to bible study, go to talks at church, watch science documentary on TV sometimes when she is alone. she reported no drug any kind used, she stated that she had smoked marijuana when she was young, and never smoked cigarette. She drinks alcohol occasionally when she is out with her friends. Her breakfast is smoothie made with frozen fruit and yogurt, lunch sandwich on wheat bread, then for dinner is chicken of fish with vegetables and brown rice or quinoa. she denied drinking coffee, but drinks diet soda occasionally, i to 2 soda per day. she takes a walk 4 to 5 time a week with yoga and swimming incorporated. She has gone outside the country recently. And she does not have any pets. N/A Mental Health History Ms. Jones is very alert and oriented x 4, to person, place, time, and situation. She is well groomed and responded appropriately to questions without difficulties, very cooperative, also focused and engaged in the conversation. Denied any feeling of depression, less stress, no anxiety, no suicidal thoughts. She reported sleeping better with good coping abilities and decrease stress. She seems very pleasant, speech flows and clear, no tics or any facial fasciculation. N/A Review of Systems - General Ms. Jones did not report any recent health problems, no fever, no chills, no tiredness, no night sweats. Ms. Jones stated that
- 4. she has change her diet and exercise more, and has lost 10lbs in the process. N/A HEENT Student Documentation Model Documentation Subjective Ms. Jones stated that she has no headache currently, and no history of head injury, no change in visual. She said that she has no eye pain, no itchy eyes, no redness, no dry eyes noted. She wears corrective glasses, and last eye checkup was 3 months ago. No hearing or ear problems noted, no ear pain or discharge noted. She said there is no change in the sense of smell, nose sneezing, no sinus pain or pressure noted, epistaxis, and no rhinorrhea noted. She denied mouth and gum problems, no change in taste, no dry mouth, no sore and no pain noted. The tongue is pink and moist without lesions, no pain to the jaw. Stated no dental issues and had dental checkup 5 months ago. She said that she has no problem swallowing, no sore throat, no change in voice and no swollen nodes noted. N/A Objective Head is normocephalic, no trauma, scalp full of hair and hair line is well distributed. Equal hair distribution on the eye lashes bilaterally, eye brows and eyelids without lesions, no eye dropping or edema noted. The conjunctiva is pink without any lesions and the sclera is white. Eyes reacted to light, PERRLA bilaterally. Bilateral EOMs intact, no nystagmus. Noted mild retinopathic changes on the right eye, left fundus is with sharp disc margins, and no hemorrhages noted. Performed Snelling test and the right eye is 20/20, and the left eye is 20/20, and she wears glasses which is a corrective lens. The ITM is intact bilaterally and pearly gray. Whispered words heard bilaterally. No tenderness noted on frontal and maxillary sinuses upon palpation. Both nasal and oral mucosa are pink and moist without ulceration or any lesions noted, and the uvula ri ses in
- 5. the middle on phonation. Gag reflex good and intact, no dental issue noted, no infection. The tonsils were 2+ bilaterally, thyroid is smooth without nodules, no goiter noted, and no palpable lymph nodes. N/A Respiratory Student Documentation Model Documentation Subjective Ms. Jones stated that she has asthma and uses inhaler for management. She said there is no current breathing issues. She also stated that occasionally she experiences shortness of breath, wheezing and chest tightness. N/A Objective Ms. Jones chest wall is symmetrical with respiration upon auscultation clear bilaterally. No coughing or wheezing noted. It resonates to percussion all around. N/A Cardiovascular Student Documentation Model Documentation Subjective Ms. Jones reported no palpations, no heart raising (tachycardia), stated no bruises, but may have had one or two in the past six month., and no sign and symptom of edema reported. N/A Objective Ms. Jones heart rate is regular, S1 and S2 indicated no murmurs, no gallops, no friction robs. Bilateral carotids arteries are equal bilaterally upon auscultation without bruit. PMI at the midclavicular line, 5th intercostal space, there no heaves or any lifts noted. Bilateral peripheral pulse is present, no peripheral edema noted. Capillary refill is less than 3 seconds. N/A Abdominal
- 6. Student Documentation Model Documentation Subjective For gastrointestinal, Ms. Jones denied nausea and vomiting, no constipation, no diarrhea, no bloating and no food intolerance. She denied dysuria, nocturia, polyuria, hematuria, no flank pain verbalized, denied vaginal discharge or itching. N/A Objective Ms. Jones is observed with no protrusion and the abdomen is symmetrical without any visible masses, scars, or any lesions on the body, hair observed from the pubic area to the umbilicus. Bowel sounds positive and normoactive in all 4 quadrants. Noted tympanic on all percussion. No tenderness, no guarding and no distension noted upon palpation. No tenderness to CVA, and organ enlargement palpated. N/A Musculoskeletal Student Documentation Model Documentation Subjective Ms. Jones denied having any joint pain, muscle pain, muscle weakness, and no swelling. N/A Objective No swollen noted on bilateral upper and lower extremities, no sign of deformities or any masses noted. She is able perform range of motion without any complaints of pain during movement. N/A Neurological Student Documentation Model Documentation Subjective Ms. Jones stated that she has not have any headaches, no light- headedness, no tingling, no seizure, no loss of coordination and
- 7. no disability. N/A Objective Ms. Jones is noted with strength is 5/5 both upper and lower extremities. She has normal graphesthesia, stereognosis and alternating the movements bilaterally rapidly. Test of the cerebellar function is normal. Noted decrease sensation to monofilament in the bilateral planter surfaces. Deep Tendon Reflexes is 2+ (DTRS) and equal bilaterally to the upper and lower extremities. N/A Skin, Hair & Nails Student Documentation Model Documentation Subjective Ms. Jones stated, "I still get zits but my acne is better than it used to be". She said that the birth control medicine is helping with the acne and the skin on her neck. she said sha has moles on her back and nothing seems different about them. She also said that the facial and body hair has improved, and denied any nails and hair changes. N/A Objective Ms. Jones is noted with rashes on the face, facial hair on the upper lip, darkened skin around her neck. N/A Mental Health Nursing Interpersonal Process Recording (IPR) Student Name: Fatumata Wongbay Date: 07/16/21 Brief information about this
- 8. client________________________________________________ ___________________________________________ Student Goal for this interaction____________________________________________ ________________________________________________ Setting/Time:_________________________________________ _____________________________________________________ _____________ Nurse Communication (Verbal & Non-verbal) Client communication (Verbal & Non-verbal) Nurse’s Thoughts & Feelings Related to the Interaction Communication Technique (Therapeutic/Non-Therapeutic) Alternative or Revised Response 1. 2.
- 10. 9. Nurse Communication (Verbal & Non-verbal) Client communication (Verbal & Non-verbal) Nurse’s Thoughts & Feelings Related to the Interaction Communication Technique (Therapeutic/Non-Therapeutic) Alternative or Revised Response 10. 11.
- 12. 18. 19. 20. Week 9 Shadow Health Comprehensive SOAP Note Template Patient Initials: _______ Age: _______ Gender: _______ SUBJECTIVE DATA: Chief Complaint (CC): History of Present Illness (HPI):
- 13. Medications: Allergies: Past Medical History (PMH): Past Surgical History (PSH): Sexual/Reproductive History: Personal/Social History: Health Maintenance: Immunization History: Significant Family History: Review of Systems: General: HEENT: Respiratory: Cardiovascular/Peripheral Vascular: Gastrointestinal: Genitourinary: Musculoskeletal: Neurological: Psychiatric: Skin/hair/nails: OBJECTIVE DATA: Physical Exam:
- 14. Vital signs: General: HEENT: Neck: Chest/Lungs: Heart/Peripheral Vascular: Abdomen: Genital/Rectal: Musculoskeletal: Neurological: Skin: Diagnostic results: ASSESSMENT: PLAN: This section is not required for the assignments in this course (NURS 6512), but will be required for future courses. © 2021 Walden University, LLC Page 2 of 3 Rubric Detail Select Grid View or List View to change the rubric's layout. Content Name: NURS_6512_Week_9_DCE_Assignment_3_Rubric Description: Note: To complete the Shadow Health assignments it is helpful to use the text and follow along with each chapter correlating to the area of assessment to assist in covering all the subjective questions. Review the Advanced Health Assessment Nursing Documentation Tutorial located in the Week 4 Resources, the model documentation in Shadow Health, as well as sample documentation in the text to assist with narrative
- 15. documentation of the assessments. Do not copy any sample documentation as this is plagiarism. Shadow Health exams may be added to or repeated as many times as necessary prior to the due date to assist in achieving the desired score. You must pass this assignment with a total cumulative score of 79.5% or greater in order to pass this course. Grid ViewList View Excellent Good Fair Poor Student DCE score (DCE percentages will be calculated automatically by Shadow Health after the assignment is completed.) Note: DCE Score - Do not round up on the DCE score. Points:
- 16. Points Range: 56 (56%) - 60 (60%) DCE score>93 Feedback: Points: Points Range: 51 (51%) - 55 (55%)
- 17. DCE Score 86-92 Feedback: Points: Points Range: 46 (46%) - 50 (50%)
- 18. DCE Score 80-85 Feedback: Points: Points Range: 0 (0%) - 45 (45%)
- 19. DCE Score <79 No DCE completed. Feedback: Documentation in Provider Notes Area Subjective documentation of the comprehensive exam in Provider Notes is detailed, organized, and includes documentation of identifying data, general survey, reason for visit/chief complaint, history of present illness, medications, allergies, medical history, health maintenance, family history, social history, mental health history, and review of systems. The review of systems is clearly defined by each body system (skin, eyes, cardiac, etc.) and all conditions or illnesses asked of the patient are documented along with the patient response.
- 20. Points: Points Range: 16 (16%) - 20 (20%) Documentation is detailed and organized with all pertinent information noted in professional language. Documentation includes all pertinent documentation to include Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS). Feedback:
- 21. Points: Points Range: 11 (11%) - 15 (15%) Documentation with sufficient details, some organization and some pertinent information noted in professional language. Documentation provides some of the Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS). Feedback:
- 22. Points: Points Range: 6 (6%) - 10 (10%) Documentation with inadequate details and/or organization; and inadequate pertinent information noted in professional language. Limited or/minimum documentation provided to analyze students critical thinking abilities for the Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS).
- 23. Feedback: Points: Points Range: 0 (0%) - 5 (5%) Documentation lacks any details and/or organization; and does not provide pertinent information noted in professional language. No information is provided for the Chief Complaint (CC), HPI,
- 24. Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS). or No documentation provided. Feedback: Objective Documentation in Provider Notes - this is to be completed in Shadow Health Physical exam: Document in a systematic order starting from head-to-toe, include what you see, hear, and feel when doing your physical exam using medical terminology/jargon. Document all normal and abnormal exam findings. Do not use "WNL" or "normal". Diagnostic result- Include any pertinent labs, x-rays, or diagnostic test that would be appropriate to support the differential diagnoses mentioned Differential Diagnoses (list a minimum of 3 differential diagnoses). Your primary or presumptive diagnosis should be at the top of the list (#1).
- 25. Points: Points Range: 16 (16%) - 20 (20%) Documentation detailed and organized with all abnormal and pertinent normal assessment information described in professional language. Each system assessed is clearly documented with measurable details of the exam. Feedback:
- 26. Points: Points Range: 11 (11%) - 15 (15%) Documentation with sufficient details and some organization; some abnormal and some normal assessment information described in mostly professional language. Each system assessed is somewhat clearly documented with measurable details of the exam. Feedback:
- 27. Points: Points Range: 6 (6%) - 10 (10%) Documentation with inadequate details and/or organization; inadequate identification of abnormal and pertinent normal assessment information described; inadequate use of professional language. Each system assessed is minimally or is not clearly documented with measurable details of the exam.
- 28. Feedback: Points: Points Range: 0 (0%) - 5 (5%) Documentation with no details and/or organization; no identification of abnormal and pertinent normal assessment information described; no use of professional language. None of the systems are assessed, no documentation of details
- 29. of the exam. or No documentation provided. Feedback: Show Descriptions Show Feedback Student DCE score (DCE percentages will be calculated automatically by Shadow Health after the assignment is completed.) Note: DCE Score - Do not round up on the DCE score.--
- 30. Levels of Achievement: Excellent 56 (56%) - 60 (60%) DCE score>93 Good 51 (51%) - 55 (55%) DCE Score 86-92 Fair 46 (46%) - 50 (50%) DCE Score 80-85 Poor 0 (0%) - 45 (45%)
- 31. DCE Score <79 No DCE completed. Feedback: Documentation in Provider Notes Area Subjective documentation of the comprehensive exam in Provider Notes is detailed, organized, and includes documentation of identifying data, general survey, reason for visit/chief complaint, history of present illness, medications, allergies, medical history, health maintenance, family history, social history, mental health history, and review of systems. The review of systems is clearly defined by each body system (skin, eyes, cardiac, etc.) and all conditions or illnesses asked of the patient are documented along with the patient response.-- Levels of Achievement: Excellent
- 32. 16 (16%) - 20 (20%) Documentation is detailed and organized with all pertinent information noted in professional language. Documentation includes all pertinent documentation to include Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS). Good 11 (11%) - 15 (15%) Documentation with sufficient details, some organization and some pertinent information noted in professional language. Documentation provides some of the Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS). Fair 6 (6%) - 10 (10%)
- 33. Documentation with inadequate details and/or organization; and inadequate pertinent information noted in professional language. Limited or/minimum documentation provided to analyze students critical thinking abilities for the Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS). Poor 0 (0%) - 5 (5%) Documentation lacks any details and/or organization; and does not provide pertinent information noted in professional language. No information is provided for the Chief Complaint (CC), HPI, Current Medications, Allergies, Past Medical History, Family History, Social History and Review of Systems (ROS). or No documentation provided. Feedback:
- 34. Objective Documentation in Provider Notes - this is to be completed in Shadow Health Physical exam: Document in a systematic order starting from head-to-toe, include what you see, hear, and feel when doing your physical exam using medical terminology/jargon. Document all normal and abnormal exam findings. Do not use "WNL" or "normal". Diagnostic result- Include any pertinent labs, x-rays, or diagnostic test that would be appropriate to support the differential diagnoses mentioned Differential Diagnoses (list a minimum of 3 differential diagnoses). Your primary or presumptive diagnosis should be at the top of the list (#1).-- Levels of Achievement: Excellent 16 (16%) - 20 (20%) Documentation detailed and organized with all abnormal and pertinent normal assessment information described in professional language. Each system assessed is clearly documented with measurable
- 35. details of the exam. Good 11 (11%) - 15 (15%) Documentation with sufficient details and some organization; some abnormal and some normal assessment information described in mostly professional language. Each system assessed is somewhat clearly documented with measurable details of the exam. Fair 6 (6%) - 10 (10%) Documentation with inadequate details and/or organization; inadequate identification of abnormal and pertinent normal assessment information described; inadequate use of professional language. Each system assessed is minimally or is not clearly documented with measurable details of the exam. Poor
- 36. 0 (0%) - 5 (5%) Documentation with no details and/or organization; no identification of abnormal and pertinent normal assessment information described; no use of professional language. None of the systems are assessed, no documentation of details of the exam. or No documentation provided. Feedback: Total Points: 100
- 37. Name: NURS_6512_Week_9_DCE_Assignment_3_Rubric Description: Note: To complete the Shadow Health assignments it is helpful to use the text and follow along with each chapter correlating to the area of assessment to assist in covering all the subjective questions. Review the Advanced Health Assessment Nursing Documentation Tutorial located in the Week 4 Resources, the model documentation in Shadow Health, as well as sample documentation in the text to assist with narrative documentation of the assessments. Do not copy any sample documentation as this is plagiarism. Shadow Health exams may be added to or repeated as many times as necessary prior to the due date to assist in achieving the desired score. You must pass this assignment with a total cumulative score of 79.5% or greater in order to pass this course.