PMU third/fourth year Clinical pathonanatomy Part 1
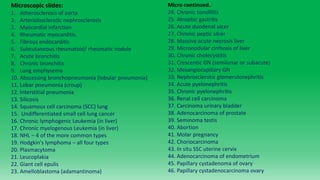
- 1. Microscopic slides: 1. Atherosclerosis of aorta 2. Arteriolosclerotic nephrosclerosis 3. Myocardial infarction 4. Rheumatic myocarditis. 5. Fibrous endocarditis 6. Subcutaneous rheumatoid/ rheumatic nodule 7. Acute bronchitis 8. Chronic bronchitis 9. Lung emphysema 10. Abscessing bronchopneumonia (lobular pneumonia) 11. Lobar pneumonia (croup) 12. Interstitial pneumonia 13. Silicosis 14. Squamous cell carcinoma (SCC) lung 15. Undifferentiated small cell lung cancer 16. Chronic lymphogenic Leukemia (in liver) 17. Chronic myelogenous Leukemia (in liver) 18. NHL – 4 of the more common types 19. Hodgkin's lymphoma – all four types 20. Plasmacytoma 21. Leucoplakia 22. Giant cell epulis 23. Amelloblastoma (adamantinoma) Micro continued.. 24. Chronic tonsillitis 25. Atrophic gastritis 26. Acute duodenal ulcer 27. Chronic peptic ulcer 28. Massive acute necrosis liver 29. Micronodular cirrhosis of liver 30. Chronic cholecystitis 31. Crescentic GN (semilunar or subacute) 32. Mesangiocapillary GN 33. Nephrosclerotic glomerulonephritis 34. Acute pyelonephritis 35. Chronic pyelonephritis 36. Renal cell carcinoma 37. Carcinoma urinary bladder 38. Adenocarcinoma of prostate 39. Seminoma testis 40. Abortion 41. Molar pregnancy 42. Choriocarcinoma 43. In situ SSC uterine cervix 44. Adenocarcinoma of endometrium 45. Papillary cystadenoma of ovary 46. Papillary cystadenocarcinoma ovary
- 2. Micro continued… 47. Fibrocystic disease of breast 48. Fibroadenoma 49. Breast cancer 50. Nodular goitre 51. Graves disease (hyperthyroidism) 52. Diabetic Glomerulosclerosis 53. Acute polio encephalitis 54. Acute poliomyelitis 55. Tuberculous leptomeningitis 56. Astrocytoma 57. Glioblastoma multiforme 58. Neurinoma (schwannoma) 59. Meningioma 60. Miliary TB lungs
- 3. 1. Atherosclerosis of Aorta (Microscopic) Numerous thin elongated “needle-like” empty spaces – cholesterol clefts or crystals. Multiple lipophages (foam cells) Media can be atrophic – dark blue stripes or intact. Ulceration of fibrous cap Mural thrombi Focal hemorrhage – red blood cells Calcifications Complications of an atheromatous plaque include: erosion, ulceration, plaque rupture, hemorrhage, arterial aneurysmal dilation, calcification and thrombosis.
- 4. 2. Nephrosclerosis Arteriolosclerotica (Microscopic): Lumen of arteriole is narrowed Thickening of wall Hyalinization At first only arteriolar changes but later – loss of nephrons, fibrosis, thickening and hyalinization of glomeruli. Hyperplastic changes: concentric laminations of arteriolar smooth muscle – “onionskin appearance” Interstitium – patchy fibrosis, chronic inflame, occasional infarction/ hemorrhage – RBC infiltrates
- 6. 3. Myocardial Infarction (Micro): Earliest stage: First 6hrs Contraction band necrosis (Irregular, dark, eosinophilic, wavy bands extending transversely across myofiber.) Myofibers lose their cross-striations After 12 hours to 2/3 days – Coagulative necrosis Central nuclei disappear Wavy fibres Outlines of myofibers remain Neutrophil infiltration at margin of infarct Macrophages filled with hemosiderin Haemorrhages 1 week – months Onset of capillary and fibroblastic proliferation at margins Fibrosis and granulation tissue/scar formation Fewer inflammatory cell infiltrates 1 Early stage – contraction band necrosis (acute MI)
- 7. Stage 2 – Coagulative necrosis evident after 6 – 12 hours and clearly visible by 24 hours; karyolysis, eosinophilia, wavy fibers, and onset of leucocyte infiltration.
- 8. Left = Later stage MI; A – Necrotic myocyte (pink) B – Fibroblast C – Collagen deposition Stage three; 10 – 12 days old: extensive granulation tissue, few necrotic myocytes are left as they have mostly been replaced. Abundant capillarisation, macrophages
- 10. Myocardial cicatrix – HE vs. Van Gieson staining 3 – several weeks post-MI Patches of fibrosis replace the myocardial cell dropout with intervening healthy myocardium. Size of scar is directly proportionate to the degree of preserved ejection fraction. Larger scars lead to complication: heart failure and arrhythmia Scar is rich in eosinophilic staining collagen, healthy myocardium appears as yellow - brown Scar tissue has low cellularity, scanty chronic inflammatory infiltrate, only a scattering of fibroblasts Some semi-damaged myocytes experience decreased size (atrophy). Other undamaged myocytes undergo reactive hypertrophy Cicatrix HE Cicatrix
- 11. 5. Fibrous endocarditis (micro); Fibrose endocarditis is one of four subtypes of rheumatic endocarditis; the other three being 1). Diffuse valvulitis/ recens/ incipiens, 2). Verrucous endocarditis and 3). Recurrent endocarditis. These are classified morphologically based on the prevailing type of damage. In fibrose type: Valve leaflets become thickened and deformed Neovascularization and calcifications Commissures are frequently fused Chordae tendineae are thickened, shortened and fused together. Metachromasia due to redistribution of glycosaminoglycans Other pathological processes of rheumatic heart disease can simultaneously be occurring in the myocardium: Modest dilation of ventricles Mural softening, myocyte necrosis Chronic interstitial inflammation and myocardial necrosis Don’t forget the pathognomonic feature: Aschoff bodies (granular fibrinoid lesions) – perivascular and subendocardial location Right: Normal valve has three clearly defined layers Fibrose endocarditis Fibrose endocarditis
- 12. 6. Subcutaneous rheumatoid/ rheumatic nodule (micro); Associated with BOTH juvenile rheumatic fever and adult rheumatoid arthritis Occur mainly over bony prominences in the extremities. Mostly non-tender, pea sixed, last 6-10 weeks and coincide with concurrent heart involvement. The lesion is typified by fibrinoid necrosis and granulomatous reaction. Usually subcutaneous location, large, firm, dome shaped mass that may or may not be painless Typically the nodule may be surrounded by adipocytes, may extend deep into reticular dermis. Fibrin deposition and necrosis in centre of nodule (acellular area) Surrounded by well-developed palisading histiocytes, vascular granulation tissue, Ly, plasma cells, eosinophiles, giant multinucleated cells. Older lesions are more severely fibrotic.
- 13. 4. Rheumatic myocarditis (Microscopic): Cause post-infection of pharynx with GABHS. Aschoff bodies = granulomatous inflammation/ nodular perivascular collection of mainly mononuclear inflammatory cells found near blood vessels characterised by “aschoff giant cells” (orange arrow) – cells with two or more nuclei and prominent nucleoli, mononuclear cells – activated macrophages called “aschoff caterpillar cells” and some neutrophils. Eosinophilic collagen representing site of antigen – antibody reaction. Aschoff bodies = areas of fibrinoid necrosis. Leads to “spindle- form” scars
- 14. Fibrinous pericarditis (Microscopic): Strands of pink/ eosinophilic, amorphic fibrin extending out from surface. Neutrophils (PMNs) can often be seen in this exudate. Unlike other forms of pericarditis, leucocytes do not invade the myocardium!
- 15. Left: Normal. Right: Acute bronchitis – debris and mucus in lumen, thickened oedematous mucosa 7. Acute bronchitis (microscopic); Purulent exudate Increased number of leucocytes mostly neutrophils and macrophages. Very little pathological change from normal anatomy Mucus glands normal Goblet cells – slightly increased in number Smooth muscle is normal
- 16. Chronic bronchitis: A= epithelial thickening B=Mucous gland hypertrophy and metaplasia C=Prominent smooth muscle Chronic bronchitis (left) A=Bronchiole wall with accumulation of mucus, wall thickening, mucous gland hypertrophy and metaplasia and scattered mononuclear inflammatory cells. B=Squamous cell metaplasia and hyperplasia of seromucous gland. 8. Chronic Bronchitis - Microscopic Increased number of inflammatory cells in submucosa. Infiltrate is mostly lymphocytes and plasma cells. Hyperplasia of glands (increased number), muscular layer and hyperplastic “cupped” cells. Metaplastic mucosa – from ciliated cylindrical to squamous. Mucous and catarrhal-purulent exudate in lumen, mucus plugging and fibrosis.
- 18. 9. Emphysema bullosa (Micro): Loss of distal airspaces Diminished number of capillaries and loss of elastic tissue Remaining spaces become dilated with less SA for gas exchange. Thinning and destruction of acinar walls. Alveolar ducts are dilated. Acanthotic pigment deposits (smoking)
- 19. 10. Bronchopneumonia (lobular pneumonia) with abscesses – micro: Most common pattern of lung infection. Bilateral, involving lower zones of lungs, common in terminally ill patients/classically hospital acquired pneumonia (HAP). Different stages of development are seen in different areas. Neutrophil predominant infiltration, patchy intra-alveolar fibrino-purulent exudates. Acute bronchiolitis (hyperaemic with suppurative exudate). Desquamated alveolocytes, macrophages Hemorrhages may occur occasionally. Complications: - Bronchiolar fibrosis - Bronchiectasis - Pulmonary fibrosis - Abscess formation
- 20. 11. Pneumonia crouposa (Lobar) – Micro HE: 90% = Streptococcus pneumoniae. Congestion phase: Predominantly eosinophilic edema fluid with bacteria visible and congested capillaries. Red hepatisation: RBCs (hemorrhage) and fibrin exudate. Congested capillaries in alveolar wall. Grey Hepatisation/ organizing pneumonia: (As seen in images) Alveolar spaces filled with neutrophils, and fibrin fibers. Due to fibrin the exudate detaches from the alveolar wall leaving a clear peripheral space. Later “Resolution;” More macrophages (predominant cell) and fibroblasts and collagen deposition.
- 21. 12. Interstitial pneumonia – micro: Commonly caused by Viruses; RSV, CMV, influenza, parainfluenza, adenoviruses, coronaviridae, rhinoviruses (cold virus), coxsackie viruses as well as the bacteria mycoplasma pneumoniae. This pneumonia is quite distinctively without alveolar exudates. Thickening of alveolar walls – congestion, edema and mononuclear infiltrate (lymphocytes, plasma cells and macrophages) Bronchiolar and alveolar epithelial proliferation – may form giant multinucleated cells and syncytia Squamous metaplasia may occur on occasion. Sometimes interstitial viral pneumonias precipitate a secondary bacterial pneumonia. Diffuse alveolar damage may be almost identical to that seen in ARDS If the disease becomes chronic, a fibrotic stage occurs.
- 22. 13. Silicosis - Microscopic Large silicotic nodules that can become confluent Consist of concentric lamellated bundles of pink collagen fibers with central “hyalinization”. Usually occur near a bronchus or bronchiole Surrounded by an encasing wall of chronic inflammatory infiltrate – mostly macrophages. Anthracotic (Coal/carbon) pigments are often seen in tandem in surrounding interstitium and some laden macrophages Polarizing light may reveal the silica crystals within the nodule
- 23. 14. Squamous cell cancer lung (microscopic) Sheets or islands of large polygonal malignant cells with abundant pink cytoplasm containing keratin. Grows as anastomosing nests and chords. Mitotic figures and intercellular bridges. Stromal reaction Tumour often infiltrates lymph vessels. Adjacent bronchial dysplasia Classified as well, moderate or poorly differentiated based on the presence of “Keratin pearls” Tumour obliterating alveolar spaces or filling alveoli Adjacent bronchial dysplasia Palisading granulomas can sometimes be seen.
- 24. 15. Parvocellular carcinoma or undifferentiated small cell lung cancer (microscopic): Small dark blue cells resembling “Oat grains” – minimal cytoplasm, very high nuclear: cytoplasmic ratio. Cells are packed together in sheets and irregular nests A highly malignant form of neuroendocrine tumour with paraneoplastic syndromes due to hormonal secretion: ACTH producing Cushing syndrome and ADH producing SIADH leading to hyponatremia. Others may produce calcitonin or parathyroid hormones, gonadotropins as well as serotonin (carcinoid syndrome). Nuclei are hyperchromatic, tumour stroma is scant. Immunohistochemistry reveals presence of markers: chromogranin, synaptophysin, pancytokeratin and neuron specific enolase. Clinical symptoms include: cough, dyspnea, anorexia, weightloss, fatigue and haemoptysis as well as clubbing, acanthosis nigricans, new onset diabetes, polymyositis, migratory thrombophlebitis and thrombotic endocarditis.
- 25. 16. Chronic lymphogenic leukaemia in liver (micro): More common in males 2:1 , often seen in older adults. Enlarged portal tracts Cells often have B cell markers CD19+, CD20+ and CD23+ and T cell marker CD5+. Preserved lobular structure “Round cell” infiltration of perivascular area - by lymphocytes and lymphoblasts. Tumour Lymphoid cells resemble healthy ones; small, mononuclear, round hyperchromic nuclei, one small nucleolus and scanty cytoplasm Pseudofollicles are common – pale, ill-defined germinal/ proliferative centres Lymphoblasts are larger with vesicular nuclei and mild polymorphism. CLL peripheral smear showing smudge cells – fragile lymphocytes easily damaged due to abnormal cytoskeletal structure, a characteristic finding for the disease
- 26. 17. Chronic Myelogenic leukaemia Liver (Micro): Lobular structure is erased. Pleomorphic leucocyte Infiltrate containing numerous myelocytes, granulocytes in several phases of maturation as well as (more rare) early undifferentiated cells; myeloblasts, promyelocytes Sinusoids fill with tumour cells. “Flows” of hyperchromic cells are observed. Periportal infiltration but not to the same degree as CLL. Hepatocytes are atrophic and separated in arcs due to the pressure- necrosis. In bone marrow: • Increased basophils and eosinophils • Hypercellular marrow with large immature myeloid cells 5-10 layers thick • Shrunken and hypo- segmented megakaryocytes
- 28. 18. Non- Hodgkin's lymphoma: • NHL 80% = B cell. NK-cell are rare. • In children: most common types are Burkitt lymphoma, acute lymphoblastic, large B cell lymphomas and anaplastic large cell lymphomas. • In adults: follicular lymphoma and marginal zone lymphoma are more common. • More likely than HL to be extranodal (Skin, CNS, disseminated, peripheral blood, bone marrow and GIT – most common extranodal site) but less likely than HL to have constitutional “B” symptoms – drenching night sweats, fever and weight-loss. NHL often has insidious onset with dysphagia and odynophagia (painful swallowing) being the chief complaints, chest/abdominal pain, pruritis, splenomegaly and weightloss also occur frequently. 1). Acute lymphoblastic lymphoma - microscopic: Effacement of tissue mass or bone marrow by round, blue cells. Large primitive cells resembling either pre-B or Pre-T cells These large blast cells may contain cytoplasmic vacuoles Oval shape, indented nuclei, finely dispersed chromatin, inconspicuous nucleoli. •Non-Hodgkin lymphomas arise from monoclonal expansion of malignant B or T cells • B cell lymphomas • B cell acute lymphoblastic lymphoma (ALL) • Chronic lymphocytic lymphoma / small lymphocytic leukemia (CLL / SLL) • Mantle cell lymphoma • Follicular lymphoma • Marginal zone B cell lymphoma • Extranodal MALT type • Hairy cell leukemia • Plasmacytoma / plasma cell myeloma • Diffuse large B cell lymphoma (DLBCL) • Burkitt lymphoma • T / NK cell lymphomas • T cell acute lymphoblastic lymphoma (ALL) • T cell CLL • Mycosis fungoides / Sézary syndrome • Peripheral T cell lymphoma • Angioimmunoblastic T cell lymphoma • Enteropathy associated intestinal T cell lymphoma • Hepatosplenic T cell lymphoma • Anaplastic large cell lymphoma (ALCL) • Extranodal NK / T cell lymphoma, nasal type
- 29. : Above panel: acute lymphoblastic (NHL “precursor type”) lymphomas. Below: Follicular lymphoma with numerous crowded follicles 2). Follicular cell lymphoma – micro: 22% of all NHLs. Extranodal involvement is rare, occurs in older patients as painless (indolent) widespread peripheral lymphadenopathy. Partial or complete effacement of lymphnode Capsule is often invaded Numerous crowded irregularly shaped lymph follicles. If sclerosis is present, nodular growth pattern is seen Small to large cleaved/ indented nuclei Mitotic figures are rare and growth is slow
- 30. 3). Diffuse large B-cell lymphoma: Many NHL’s in adults are of the large cell variety, most of which are sporadic and B cell type (CD19+/ CD20+). Large cleaved cells with large eccentric nuclei and prominent nucleoli (1-2) and moderate amount of metachromatic/ amphophilic pale cytoplasm Mitotic figures are frequent Diffuse growth pattern Tend to be localised in early stages but with rapid aggressive nodal enlargement and higher tendency to become extranodal in later stages than other NHLs. 4). Burkitt's lymphoma – microscopic: Very common in children (30% of cases) but rare in adults. Highly aggressive but often curable. Three subtypes: African endemic – associated with EBV and usually presents in the jawbone, Sporadic form – more pleomorphic/ multinucleated than the others and immunodeficiency-related form – in children with HIV. Sheets of monotonous intermediate sized cells with “Starry sky pattern” – produced by cellular debris phagocytosed by large macrophages Mitosis is commonly seen. Round nuclei, finely clumped chromatin and several nucleoli Neoplastic cells have squared-off borders from pressing against one- another.
- 31. 19. Hodgkin's lymphoma 4 types (micro): Classic finding = Reed-Sternberg cells (large multinucleated cells, bi-lobed with “mirror-like” symmetry, 1-5% of neoplastic cell population, nuclei appear like owl eyes due to prominent nucleoli.) Normal lymphnode structure is effaced/ destroyed. Reactive cells include lymphocytes, macrophages, eosinophils and fibroblasts. Cell-mediated immunity is usually reduced in these patients (immunocompromised) There are four subclasses of Hodgkin's disease: Patients often have splenomegaly 1). Mixed cellularity 2). Nodular sclerosing 3). Lymphocyte predominant and 4). Lymphocyte depleted 1). Mixed cellularity type: Many different types of cells are see; small Lymphocytes, Mafs and eosinophils. Many large pale lacunar cells: multinucleated, nuclei frequently overlap or have surrounding vacuolar halos – “coins on a plate appearance”). Reed-Sternberg cells present Right: mixed cellularity type HL Below: Lacunar cells – money on a plate
- 32. More likely to occur in older age and B symptoms are very common Capsule of affected LN is fibrotic, thickened and infiltrated. Moderate vascularisation, necrosis and fibrosis 2). Nodular sclerosing Type: Prominent bands of pink collagenous tissue divides the cellular infiltrate into nodular growth pattern. Lacunar cells may aggregate into syncytiates. usually cells are confined within the thickened capsule Mitotic figures are uncommon. Most common form of HL (60% of all cases, most common in young adults) Background infiltrate = lym, plasma, eos (often numerous) and mafs (may be foamy). Reed-Sternberg cells and lacunar cells are frequent Necrotic foci Most cases when diagnosed are low stage: I or II Top right: Mixed cellularity HL, all other images = Nodular sclerosing HL with eosinophilic connective tissue bands clearly visible
- 33. 3). Lymphocyte predominant HL: Lacks many Reed- Sternberg cells – therefore difficult to distinguish from small cell lymphomas. Characteristic cell present = “Popcorn cells” – these are multilobulated, large nuclei histiocytic and lymphocytic cells. Unlike lymphocyte depleted HL this variant is dominated largely by presence of lymphocytes, the lymphnodes are very frequently destroyed and usually there is still some nodularity and rarely diffuse pattern with lack of nodularity. T zone attenuation: Germinal centres (bright) are regressed and small/ absent 4). Lymphocyte depleted HL: Has very numerous RS cells, look very bizarre, often in sheets Few lymphocytes or other reactive cells Least common form, mostly in old men, assoc. with EBV Diffuse fibrosis is usually present Complete effacement of LN, not order to the connective tissue and no clear nodules like in nodular sclerosing HL Focal coagulative necrosis Right and below: lymphocyte predominant Left and below: lymphocyte depleted HL
- 34. 20. Plasmacytoma (Microscopic HE): • Composed of malignant cells that resemble plasmacytes but with larger, eccentric and peripheralized nuclei and abundant basophilic cytoplasm. • Grossly the mass is jelly-like and induces local osteolysis. • May contain mature (pear-shaped or oval), immature, plasmablastic (dispersed chromatin and much larger cells) and anaplastic plasma cells • Amyloidosis may be present in extraosseous plasmacytomas and presents as a pink amorphous material scattered with multi-nucleated giant cells. • Most common extraosseous location is near the nasopharynx and sinuses as focal accumulations of submucosal lymphoid tissue.
- 35. 21. Leucoplakia - micro: Squamous epithelium is thickened – hyperplasia of basal and keratin layers with enlarged papillae which deeply invaginate the underlying supporting tissue (acanthosis). Parakeratosis is seen – abnormal preservation of nuclei in the upper strata of the epithelium. Hyperkeratosis – excessive accumulation of corneous substance There are several subtypes: classic, hairy, verrucous, and erythroplakia. Erythroplakia (grossly red and eroded type) have higher chance of malignant transformation Nuclear hyperchromasia or increased nuclear: cytoplasmic ratio may be seen. Inflammatory infiltrate is scanty or absent in this lesion. Underlying submucosa has increased collagen deposition. There is no cellular atypia however leucoplakia is a pre- cancerous lesion due to its tendency for squamous metaplasia. Mechanical irritation (ill-fitting dentures), alcohol and tobacco use are etiological factors. Left: verrucous subtype with undulating structure, no cellular atypia but marked hyperkeratosis Left: classic type with increased collagen deposition in stroma and acanthotic squamous cell epithelium but no cellular atypia.
- 36. 22: Giant Cell Epulis (giant cell granuloma) – microscopic: o Epulis is a tumour-like process in the gingiva. o It is a hyperplastic reaction of the connective tissue to repeated trauma and inflammation. o It is covered with multi-layered squamous epithelium with parakeratosis (retention of nuclei in the upper layers of the epithelium – stratum corneum). o Epulis is often ulcerated with granulation tissue below the epithelium. o Two constituent cells are: A). Fibroblast-like cells, B). Giant multinucleated cells resembling osteoclasts. This cellular zone is separated from the epidermis by a layer of connective tissue. o The giant cells are surrounded by a vacuolar halo separating them from the rest of the tissue. They are round, basophilic and with dozens of oval nuclei. o Epulis is very highly vascularised, they hemorrhage very frequently and evidence for this is seen in the often abundant hemosiderin deposits. o Variable mitotic activity o Non-encapsulated growth o Most common type is giant cell epulis but other types include angiomatous and fibromatous epulis. Above circle: a giant cell with halo, right: oblong cut-out showing dark brown hemosiderin deposits, rectangle highlights connective tissue dividing multi-layered squamous epithelium (orange arrow) from cellular region.
- 37. : 23. Ameloblastoma (adamantinoma) – microscopic: Rare, non-cancerous/ benign tumour that develops in the jawbone near the molars. Though benign, the tumour is locally aggressive and often grows rapidly. It is derived from the germinal tooth epithelial cells that produce enamel. Follicular type: most common, germinal epithelium is arranged on oval follicles, with clear linear palisade arrangement around the periphery but haphazard organisation in the centre. Follicles are multiple and of various size with fibrous septae between. Centrally the cells have a starry-like appearance, cells show reverse polarisation of nuclei away from basement membrane. Cystic spaces form between tumour nests, cystic destruction of bone shows on radiograph as characteristic “soap bubbles” lesion. Other variants include plexiform , acanthomatous, granular, desmoplastic and basal cell variants. Left close-up: Reverse polarisation of nuclei away from basement membranes
- 38. 24. Chronic tonsillitis - microscopic: During active infection bacteria colonies and purulent exudate may be seen in the tonsillar crypts Has two forms: atrophic and hypertrophic Atrophic type: epithelial atrophy, fibrosis and inflammatory infiltrate. Hypertrophic type: hyperplasia and hypertrophy of lymph follicles with light germinal centres. Sclerotic tissue is found in bands below them. Lacunae are dilated Epithelium is desquamated (flaking off). Some cellular debris may be concentrically compacted into cholesterol deposits that over time calcify – amygdalites (tonsil stones).
- 39. 25. Atrophic gastritis – microscopic: • Glandular atrophy – their height is significantly diminished. Covering epithelium looks squished/ flattened. • Glands are compressed and later destroyed. • Intraglandular areas widen as glands are reduced in number and in them we find chronic inflammatory infiltrate (lympho + plasma cells). • Thinned mucosa is interspersed with fibrous CT between the glands. • Often duodenal or gastric ulcers are seen in association with this condition • Intestinal metaplasia is seen in gastric epithelium – increased number of vacuolated mucous producing goblet cells. • Giemsa staining can visualise blue-grey stick like organisms; helicobacter pylori. • A subtype exists; follicular gastritis where lymphoid follicles develop. Left: Normal gastric mucosa Right: atrophy and sparsity of glands, intestinal metaplasia, increased connective tissue and leucocytes
- 40. 26. Acute duodenal ulcer – microscopic: • Ulcer is usually small <1cm and round. • The margins are sharply circumscribed with abrupt change from normal mucosa to ulceration. • Ulcer base may contain brownish-black deposit – digested blood (hematin). • Mucosal defect that penetrates through muscularis mucosae (unlike an erosion) to reach muscularis propria. • The cavity is filled with fibropurulent exudate and lymphocytic infiltrate in surrounding tissue. • Glands in the ulcerated area are destroyed. • Underlying duodenal layers are not fibrosed and there is no blood vessel thickening unlike gastric ulcers. • Helicobacter pylori is often present (Grey-blue on giemsa staining) • Often surrounding proximal duodenal villi are edematous (active duodenitis). • Gastric foveolar metaplasia may be present when chronic.
- 41. 27. Chronic peptic ulcer – microscopic: Focal loss of gastric epithelium Ulcer extends down to lamina muscularis of the submucosa. The ulcer is well-demarcated. Vessels at the base of the ulcer are often eroded and local hemorrhage is often observed Nearby vessels are hyperaemic and often have thickened walls (endarteritis and endophlebitis) due to stimulation by chronic inflammatory cytokines. Peripheral nerves in the affected area may hypertrophy reactively to become amputation neuromas Bacteria, pus (neutrophils) and necrotic debris may be seen in and around the ulcer if active. Muscular wall replaced by fibrose tissue, proximal gastric glands are hypertrophic. Lymphoid follicles may develop close to the ulcer or pre-existing ones will be hyperplastic. Base of ulcer shows fine dark pink line (fibrinoid necrosis). Below the base we can see an inflammatory infiltrate consisting of mafs, lymphocytes and plasma cells. Immature connective tissue is laid in proximity to the lesion Granulation tissue can be seen in the lesion. Non-active ulcers that are healing will show regeneration of fresh epithelium over the ulcer as well hyalinisation of submucosal and intestinal metaplasia.
- 42. 28. Massive acute necrosis Liver – microscopic: Entire liver lobules are necrotic and microscopic lobular structures are unclear/ ill-defined. Panacinar necrosis with collapse of the reticular framework. Peripherally there may be some small concentrations of spared healthy hepatocytes. Hepatocytes show balloon (hydropic) degeneration. Nuclei undergo karyolysis and karyorrhexis. Proliferated and dilated bile ductules Scanty inflammatory infiltrate Regeneration is sparse and where it does occur it is highly irregular and disorganised Unlike cirrhosis, fibrosis is not a prominent feature of acute fulminant hepatitis (no time to form). Clinically, the patient will be experiencing severe haptic failure; jaundice, ascites, coagulopathy, edema, hepatic encephalopathy, hepatorenal/ hepatopulmonary syndromes. Left: healthy normal hepatic lobular structure Right: severe widespread destruction of hepatic architecture
- 43. 29. Micronodular Cirrhosis of Liver – microscopic Micronodules are less than 3mm this type is associated with alcoholic disease. No normal lobular architecture Central veins difficult to see. Early: Delicate fibrous septae spanning from central vein to portal triad or from portal –to portal regions. Extensive fatty change is also typical at this stage. Late: fibrous septae become much thicker, denser and confluent with one another. Fatty change is replaced/ not as prominent as before. Regenerative nodules (pseudo-lobules) can be observed – islands of isolated/ stranded hepatocytes proliferate in a disorganised mass, mostly without development of a central vein. These nodules are at increased risk for malignant transformation (HCC). Bile ducts may proliferate in response to biliary stasis as may additional blood vessels. Mallory bodies (eosinophilic hyaline globule inclusions in hepatocytes that indicate injury/ disease especially alcohol consumption) become rarer to spot as cirrhosis progresses. Fibrose septae around the micronodules usually have mild macrophage/ lymphocyte infiltration and hemosiderin deposits.
- 44. 30. Chronic Cholecystitis – microscopic: • Almost always seen in conjunction with gallstones but can happen with thickened sludgy bile alone (acalculous cholecystitis) • 2 histological forms exist; A). Hypertrophic and B). Atrophic. • hypertrophic type: epithelium intact, wall and mucosal folds are abnormally thickened, blunting of villi, infiltration by lymphocytes and plasma cells. • Atrophic type: usually due to long standing increase in intraluminal pressure due to gallstones. Thinned wall with shrunken, small villi, muscle in the wall is atrophic and almost completely replaced with fibrose tissue. The wall is infiltrated with leucocytes. • Deep invaginations between mucosal folds are called Rokitansky-Aschoff sinuses. • Difference with acute cholecystitis: In acute cholecystitis, the inflammatory reaction is neutrophilic not lymphocytic. Also the acute form tends to be purulent with the presence of bacterial overgrowth while infection is rarely implicated in the chronic form.
- 46. Acute proliferative Glomerulonephritis (micro): • Associated with NEPHRITIC SYNDROME • Lots of neutrophils infiltrate around capillary loops. Capillary loops are poorly defined. • Increase in number of mesangial, epithelial and endothelial cells. • Interstitial edema varies. • No tubular changes • Usually occurs 1-4 weeks after strep (GABHS) infection as a result of immune-complex deposition, but one third of cases are non- strep; pneumococci, staph, meningococci, pseudomonas etc. • Enlarged/ inflamed and hypercellular glomeruli. • All glomerular capillary loops are involved • Inflammation = “diffuse”/ “Global”
- 47. 31. “Rapidly progressive” or Crescentic (semi- lunar glomerulonephritis) - microscopic: • Obliteration of bowmans capsule • Semi-lunar “fibrin” cap develops – proliferation of epithelial cells/ podocytes and mafs (basophilic) in response to leaking fibrin. • Crescents in >50% of Glomeruli. • Compressed capillary loops • Narrowing and closure of bowmans space. • RBCs in bowmans space • Causes NEPHRITIC SYNDROME Causes: idiopathic, post-infectious with streptococcus, SLE immune complex deposition, vasculitis (pauci immune – little evidence of hypersensitivity), Goodpastures syndrome (auto- antibodies to basement membrane). • Tends to have fulminant course, poor prognosis.
- 48. Membranous GN (micro): • Looks “Pink” / eosinophilic due to thickened glomerular capillary wall membranes. • No hypercellularity • Later in disease there is doubling” or duplication of the basement membrane which can be seen as black with silver impregnation. • Most common cause of nephrotic syndrome in adults. • Loss of anticoagulant proteins from blood pre-disposes patient to renal venous thrombosis. Silver impregnation (above)
- 49. 32. Membranoproliferative (Mesangiocapillary) GN: • Hypercellular but unlike Acute GN there are no neutrophils (PMNs). • Mesangium proliferation and increased matrix pushes on endothelium increasing the lobular appearance of the tuft. • Capillary wall thickens (GBM) • 50% of patients develop renal failure within a decade. Some cases become rapidly progressive. Corticosteroids seem to be ineffective. • Causes are numerous: Hep B/C, Malignancies, Jones silver stain will show “tram-track” doubling of GBM.
- 50. Focal proliferative or “mesangioproliferative” GN – micro: • Only affects a portion of some of the glomeruli (focal). • Hyalinosis is involved (sclerotic) – as disease progresses the affected glomerular retract/ shrink. • Thickened pink glomerular looks can sometimes be seen – “wire loops” appearance. • Not hypercellular. • Causes: vasculitis, IgA nephropathy, SLE, goodpastures (autoimmune).
- 51. Focal segmental GN- micro: • Only some glomeruli are affected (focal) and only small parts of their tufts (segmental). • Characterised by sclerosis and hyalinosis – hardening – of one or more lobules. • Eosinophilic, PAS (collagen =red) positive, homogenous hyaline material can be seen on inner side of peripheral capillary loops. • Tubular epithelium is atrophied and degenerates. • Interstitial fibrosis and infiltration by leucocytes can be seen.
- 52. Very important to understand which GN types cause which syndrome , as well as the key differences between these renal syndromes!